Introduction
Pancreatic pseudoaneurysms are uncommon complications of acute or chronic pancreatitis (7). They form from pseudocyst that erodes the adjacent arteries. Pseudoaneurysm formation is the commonest of these vascular accidents in the middle age population with the male to female ratio of 4.5:1. Pseudoaneurysms affect the arterial wall, the medial and intimal layers, and their prevalence is higher than that of true aneurysms (8).
Since pancreatic pseudoaneurysms associated with bleeding, the splenic artery is very vulnerable to bleeding when compared to the gastroduodenal arteries. The splenic artery runs along the bed of the pancreas and extends to the spleen, and thus, it is vulnerable to bleeding due to its close proximity to the pancreas (8). The gastroduodenal artery has a bleeding incidence rate of between 10 to 15% compared to the pancreaticoduodenal artery’s 10% (8).
Overall, the small intrapancreatic, and left gastric arteries have the lowest incidence of bleeding. The pathogenesis of gastroduodenal artery aneurysm is unclear, but it usually occurs due to blunt trauma or secondary to pancreatitis (4). Given that pseudoaneurysm is deadly when it ruptures, early diagnosis and management is necessary (10). Thus, this case report aims to alert sonographers and ultimately improve the diagnosis and management of pancreatic pseudoaneurysm.
Case Study
A 72-year-old female with a history of alcohol abuse, a right frontal metastatic deposit in the brain, and adenocarcinoma of the lungs presented herself to Nepean hospital with recent acute epigastric pain, vomiting, and weakness. A physical assessment revealed that the patient had jaundice, high blood pressure (100/60mmHg) and HR of 110 per min. The pathology results indicated that she had high levels of amylase and lipase, which suggested acute pancreatitis, while hemoglobin level was 83g/L, (normal range 130–170g/L).
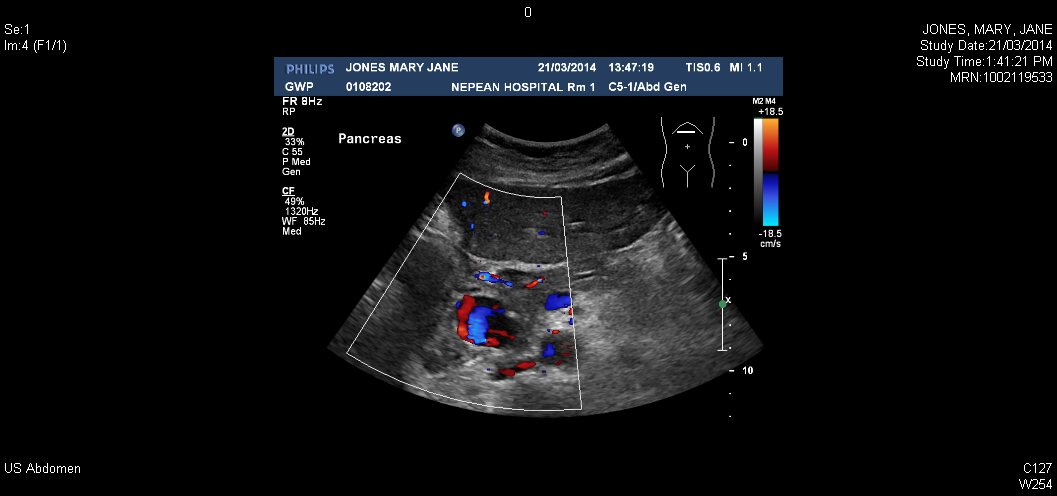
An Abdominal ultrasound was requested to determine the presence of gallstones and was performed in the medical imaging department, Nepean Hospital. A Phillips IU22 ultrasound machine with a curved array 5MHz transducer was used for B-mode imaging. The patient was positioned supine for imaging of the abdomen.
A transverse scanning of her pancreas depicted a dilatation of a hypoechoic area (3 cm x 2.2 cm x 2.8 cm) with a solid rim containing cystic central portion was observed anterior to the head of the pancreas in conjunction with marginally dilated pancreatic duct measuring 3.8mm. In addition, Doppler sonography revealed that a typical swirl flow (Yin- Yang sign) within the central portion was consistent with the pseudoaneurysms with a trace of gastroduodenal artery (1).
The rest of the abdominal ultrasound scan showed that the liver measures 9.8 cm in length with normal echotexture. The portal vein was mildly dilated; it measured 1.5cm with intrahepatic while the common bile duct dilatation is 9.8mm. During the examination, the patient said that she had cholecystectomy seven years ago, which was a very important clinical information. The absence of gall bladder throughout the scanning confirmed the removal of the gall bladder.
The right kidney and left kidneys were normal in size, 10.4 and 9.4 cm respectively, with normal echotexture. The size of the spleen was also normal because it measured 7.5 cm in length, while the aorta showed a normal diameter of 2.3cm. Further scanning showed that the urinary bladder contained debris, which represented a possible urinary tract infection.
The ultrasound findings were reported as a pancreatic pseudocyst with pseudoaneurysm formation. The report was sent to the referring doctor, with a recommendation to confirm the findings using computed tomography (CT) of the abdominal angiogram.
CT scan was performed with a Siemens Somatom 64 slice CT scanner, using 100 ml of iodized intravenous contrast with an injection rate of 4ml/ second. Further evaluation with CT angiogram showed contrast enhancement of the hypoechoic region of the gastroduodenal artery, which confirmed that pseudoaneurysm was rising at its distal bifurcation.
Following this diagnosis, the patient was referred to as immediate Digital Subtraction Angiography. After confirmatory angiography, the lesion was embolised successfully by using embolization particles. The particles occluded the distal section, which reduced gastroduodenal aneurysm. After the procedure, the patient was admitted in the ward.

Discussion
The gastroduodenal artery branches from the hepatic artery. The gastroduodenal artery links with the pancreas at the superior and the right sides of the pancreas. It supplies blood to the pancreas, the stomach, the duodenum, and the distal bile duct. Over drinking and gallstones, which block the gall ducts, increase the risk of developing pancreatitis.
Ample evidence accumulated for over decades shows that gastroduodenal artery aneurysm, ethanol abuse, peptic ulcer disease, and cholecystectomy account for about 47%, 25%, 17%, and 3% of all cases of pancreatitis respectively (2). Congenital abnormalities like liver cirrhosis, Marfan syndrome, and Ehlers-Danlos syndrome are other causes of pancreatitis. Moreover, vascular abnormalities like polyarteritis nodosa, fibro-muscular dysplasia, septic emboli, and trauma predispose individuals to pancreatitis.
Obstruction of the pancreatic duct is believed to be responsible for increased intraductal pressure and release of pancreatic proteolytic enzymes such as amylase and lipase (7, 6). Pseudocysts are common complications that arise within or around the pancreas in patients with pancreatitis. These are walled off fluid collections containing pancreatic enzymes surrounded by a fibrous capsule, which lacks the epithelial lining (6).
The occurrence of pseudocyst varies according to the nature of pancreatitis because of 5 % to 15% of patients with acute pancreatitis and 20% to 40% of patients with chronic pancreatitis experience pseudocyst (2). Fundamentally, pseudoaneurysms and pseudocysts are pancreatic conditions, which arise from acute and chronic pancreatitis and complicate the treatment of pancreatitis. Due to high mortality rates of bleeding from a pseudocyst, medical researchers have extensively studied vascular complications.
The erosion and digestion of arterial walls cause pseudocyst to rapture and become a hemorrhagic pseudocyst, and then turn into pseudoaneurysms (4). The bleeding due to the erosion of the pseudocyst can rarely bleed internally from pseudoaneurysms, which can be an extremely serious complication. Since the rupture results in internal bleeding, the hemorrhagic cyst causes abdominal pain. The internal bleeding causes the hemorrhagic cyst to swell up and form a pseudocyst.
Pseudocysts affect many areas of the body, including the duodenum, the colon, the gastric wall, the groin area, and the mediastinum (4). In chronic pancreatitis, pseudocyst may cause thrombosis of the portal vein and its branches, leading to portal hypertension and variceal hemorrhage. Among these vascular complications, pseudoaneurysms are the commonest causes of gastrointestinal hemorrhage.
Pseudoaneurysms are detected incidentally on imaging because they can be either asymptomatic or symptomatic. The common symptom of gastroduodenal artery aneurysms is right upper quadrant pain. Recent advancements in the diagnostic imaging modalities have increased the chances of detecting aneurysms.
The sonography is the basic diagnostic procedure done when one experiences abdominal pain. It is an appropriate test because it is cheap and does not require radiopaque contrast material (2). The sonography plays an important role in evaluating the biliary tract for the presence of possible obstruction by gallstones, the existence of pseudocysts, and pseudoaneurysms. While greyscale US scan detects the existence of pseudoaneurysm, colour-Doppler ultrasound effectively detects the vascular nature of pseudocyst (9).
However, the limitation of the ultrasound is that obese patients and overlying bowel gas restrict the detection rate to as low as 33% (5). Some techniques can be used to overcome these problems include increased transducer pressure, varying patient position, and breathing techniques. Since vascular angiography accurate and sensitive in detecting pseudoaneurysms, it has become the gold standard (2).
Angiographic embolization and surgical intervention are two main treatment interventions for pseudoaneurysms. Multiple studies have documented the efficacy of angiographic embolization in the management of hemorrhagic pseudocysts, while the surgical procedure is effective because it entails surgical ligation of pseudoaneurysms (3, 2, 4, and 8). Thus, the surgical procedure is reliable because it removes the diseased pancreas and thus addresses the root cause of the disease.
Conclusion
Pseudoaneurysms are common among patients with acute and chronic pancreatitis. Their occurrence complicates the pancreatic pseudocysts, although they can occur on their own. In this view, early detection is imperative to the prevention of the rapture of aneurysms in the vessels and causes lethal complications.
The imaging techniques such as computed tomography, Doppler ultrasound, magnetic resonance imaging, and angiography are currently applicable in the diagnosis of aneurysms. The patient, in the case study, was very lucky because she received prompt and effective diagnosis using ultrasound and CT scan, and obtained successful treatment with angiographic micro-coil embolization.
This case study is important because of the following three reasons. Firstly, I noted that early diagnosis and critical imaging improve the detection rate of pseudoaneurysms and thus, saves the patient from fatal complications associated with pancreatitis. Secondly, the case study made me understand the essence of patient-doctor communication.
If poor communication occurs or referring doctors make mistakes, unnecessary imaging will arise and complicate the job of sonographers. In our workplace, poor communication is a common occurrence, which affects the diagnosis and treatment of patients. Thirdly, I was involved in all imaging procedures in the diagnosis and treatment process of angiographic embolization.
References
- Habib, N., Hassan, S., Abdou, R., Torbey, E., Alkaied, H., Maniatis, T., Azab, B., Chalhoub, M. & Harris, K. 2013, ‘Gastroduodenal artery aneurysm, diagnosis, clinical presentation and management: a concise review’, Annals of Surgical Innovation and Research, vol. 7, no. 4, pp. 1- 6. Web.
- Hourani, S., Badour, N., Rashaideh, A., Nawayseh, R., Alasmar, A., Alakasasbeh, A. & Gazaleh, A. 2008, ‘Pseudo Aneurysm complicates Pancreatic Pseudo Cyst: Importance of Early Detection and Management’, Journal of Surgery Pakistan, vol. 13, no. 1, pp. 42 -45. Web.
- Irwine, C., Kay, D., Kirsch, D., & Milburn, J. 2013, ‘Renal artery embolization for the treatment of renal artery Pseudoaneurysm following partial nephrectomy,’ The Ochsner Journal, vol. 13, no. 2, pp. 259-263.
- Jain, C., Joshi, S., Subramanyam, G. & Sinha, N. 2013, ‘Rupture of Gastroduodenal Artery Pseudoaneurysm,’ International Journal of Case Reports in Medicine, vol. 2013, no. 2013, pp. 1-5. Web.
- Matsuzaki, Y., Inoue, T., Kuwajima, K., Ito, Y., Okauchi, Y., Kondo, H., Horiuchi, N., Hasegawa, K., Iwata, M., & Yoden, M. 1998, ‘Aneurysms of the Gastroduodenal Artery,’ Japanese Society of Internal Medicine, vol. 37, no. 11, pp. 930-933. Web.
- Middleton, D., Kurtz, B. & Hertzberg, S. 2004, Ultrasound: The requisites, Mosby, Missouri.
- Patel, B., Shah, R., Shah, S., Patel, B., Jain, S., & Kumar, A. 2003, ‘Case report: Pseudoaneurysm from Gastroduodenal Artery Associated with Chronic Pancreatitis; An Unusual Complication.’ Indian Journal of Radiology Imaging, vol. 13, pp. 311- 313. Web.
- Salinas, G. & Sickle, V. 2008, ‘Intermitted Gastrointestinal Bleeding from Left Gastric Artery Pseudoaneurysm Successfully Treated with Coil Embolization,’ The Internet Journal of Surgery. Vol. 20, no. 1, pp. 1- 4.
- Tandazo, W., Ortega, J., & Mariscal, C. 2013, ‘Spontaneous regression of splenic artery pseudoaneurysm: A rare complication of acute pancreatitis,’ International Medical Case Reports Journal, vol. 6, no. 1, pp. 17-20.
- Young, R., Gagandeep, S., Grant, E., Palmer, S., Mateo, R., Selby, R., Genyk, Y. & Jabbour, N. 2004, ‘Gastroduodenal Artery Pseudoaneurysm Secondary to Pancreatic Head Biopsy,’ Journal of Ultrasound Medicine,’ vol. 23, pp. 997-1001.