Introduction
Minimally invasive gastrostomy is the transabdominal insertion of a tube into the gastrointestinal to supply feed, relax, and offer medication. The first of these is the most frequent source of gastrostomy tube (G-Tube) implantation and is essential for preserving nutritional intake and enhancing prognosis across a broad spectrum of diseases (Rajan et al., 2022). The insertion of a G-Tube provides enteral accessibility for nourishment, dilatation, and medical treatment. Percutaneous endoscopic gastrostomy (PEG) is one of the minimally invasive enteral feeding implantation techniques (Rajan et al., 2022). Since this is an intrusive operation with various possible adverse events (AEs), it is vital to pick the proper patients and approach. Therefore, this essay aims at providing a deeper understanding on G-Tubes since they have proven essential in the management of illnesses or disorders that may require their utilization. Moreover, the paper provides an explanation of the different types of G-Tubes and how the insertion is done to meet the healthcare needs of affected patients. Finally, the essay offers a discussion concerning the information consent of people who need G-Tubes for their treatment.
Gastrostomy Tubes Indications
Installing a G-Tube is typically advised to deliver nourishment and bypass blockage regardless of the clinical setting. Certain diseases, such as stomach volvulus, may need a G-Tube during the gastropexy surgery. However, in patients who suffer from illnesses requiring more than four weeks of supplemental enteral nourishment, insertion of the gastrostomy tube is recommended (Shellnutt, 2019). Hyperemesis gravidarum, Guillain-Barré syndrome, severe bruising, cerebral trauma, gastroesophageal dysfunction, starvation, acute stroke, eating disorders, face trauma, particularly in individuals before transplantation, and head and neck cancers receiving therapy are examples of such disorders (Rajan et al., 2022). Additionally, irreversible gastrostomy tubes may be necessary to enhance the quality of life in specific illnesses with an adverse prognosis. Examples include neurodegenerative diseases such as amyotrophic lateral sclerosis and multiple sclerosis, developed head and neck carcinomas, oropharyngeal deformities, and sophisticated esophageal or gastric neoplasms (Rajan et al., 2022). Other illustrations encompass rheumatologic-related disorders with esophageal abnormalities, such as cystic fibrosis, scleroderma, and amyloidosis.
Methods of Gastrostomy Tube Placement
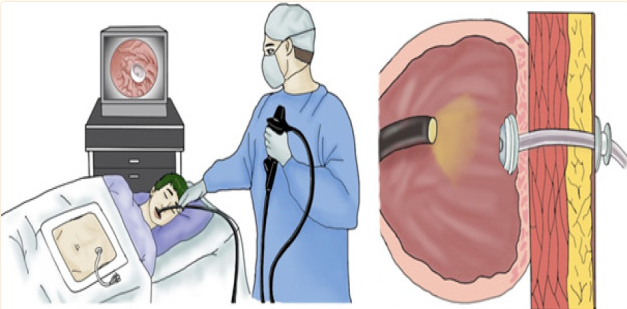
Endoscopic G-Tube Placement
With endoscopic monitoring for PEG, the pull methodology, the push-over-wire procedure, and the introducer procedure may be utilized based on instruction or practitioner choice. The introducer procedure is the only real transabdominal way to avoid transoral entry of the PEG catheter (Yasin et al., 2020). If fluoroscopy cannot be utilized, the SLiC procedure can be conducted with a small-bore endoscope on individuals with near-obstructive head and neck cancer. Using the pull technique, the needle is then withdrawn, and a thread of silk stitch is inserted through the residual tube and into the stomach. The yarn is caught by the hook that passes through the endoscope. The thread is extracted using an endoscope inserted into the mouth. The string’s wire loop is attached to the PEG tube’s cable. The device is then drawn back via the mouth, the belly, and the abdominal wall using a string. Unlike the push-over-wire and pull approaches, the introducer technique prevents PEG tube interaction with the oropharyngeal region (Yasin et al., 2020). This method is usually performed by radiologists for fluoroscopic insertion, though endoscopists can also execute it.
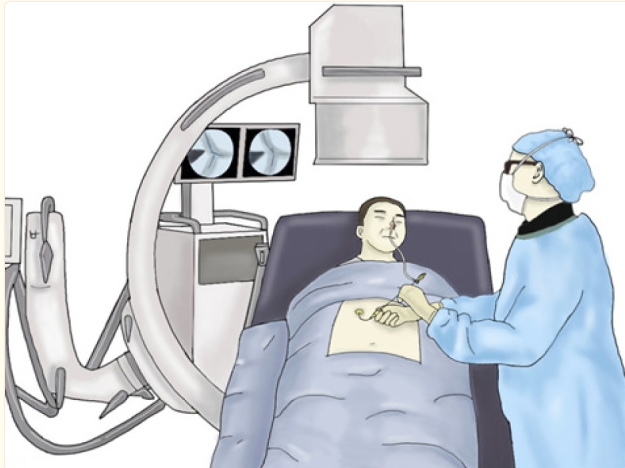
Radiologic G-Tube Placement
Percutaneous radiological gastrostomy (PRG) can be accomplished trans-abdominally with push type A methodology, Seldinger, and push type B strategy, Peel-away sheath. The mentioned tactic is accomplished under imaging studies, computerized tomography (CT), or ultrasonography supervision (Rajan et al., 2022). If required, PRG can perform gastropexy using T-fasteners or other instruments comparable to the introducer approach. For transoral administration, the composite per-oral image-guided gastrostomy approach (PIG) has also been utilized (Rajan et al., 2022). When gastrostomy is inappropriate, as in the case of major intractable hydrocephalus, belligerent abdomen, or severe abdominal carcinomatosis, percutaneous transesophageal gastro-tubing (PTEG) with imaging monitoring can be utilized to insert an esophagostomy (Rajan et al., 2022). As shown in figure 2, below is a pictorial representation of radiologic G-Tube placement.
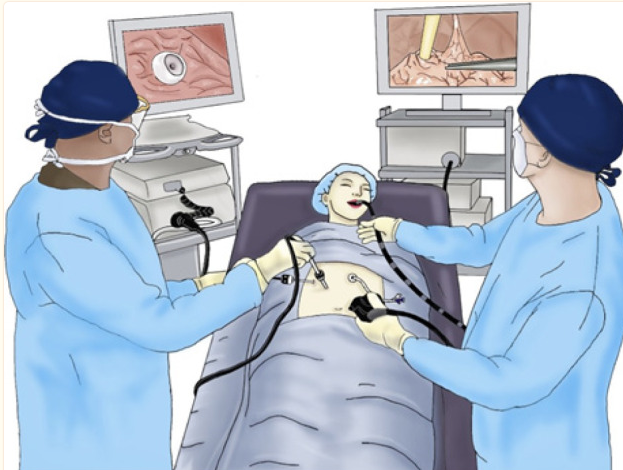
Laparoscopic G-Tube Placement
The implantation of a gastrostomy tube can be accomplished laparoscopically. Percutaneous laparoscopic-assisted gastrostomy (PLAG) necessitates two transverse trocars for gastropexy with stitches and catheter placement (Rajan et al., 2022). Exclusion criteria for laparoscopic G-Tube insertion include the inability to withstand pneumoperitoneum, significant lung or cardiovascular problems, persistent skin wounds, or poor treatment for a chronic condition, as this is neither an emergency nor an urgent intervention (Rajan et al., 2022). An open Stamm gastrostomy requires a laparotomy, four threads to connect the stomach to the front stomach membrane, and purse-string stitches to attach the nasogastric tube to the belly. With the aid of endoscopic intraluminal imaging of the stomach, a catheter is inserted through the skin and into the abdomen during a PEG (Rajan et al., 2022). As demonstrated in Figure 3, a unique composite laparoscopic-assisted PEG (LAPEG) is a mixture of gastroenterology and laparoscopic imaging.
Effective Informed Consent and Medical Management
To honor individual freedom over presumed beneficence, the installation of a G-Tube should incorporate the patient’s informed and knowledgeable permission. Legal precedent over the past three decades has concluded that artificial nourishment is not distinct from other medical interventions and that there is no need to supply it if it is not desired. If the patient cannot offer authorization, the approval of the healthcare insurance proxy named in a living will be acquired. If the individual is believed to be terminally ill, the written will must be executed. The patient must have reasonable goals for the G-Tube’s potential benefits.
Clinical signs can initiate the decision-making procedure but are infrequently sufficient. The importance of social support in lowering G-Tube reliance should also be explored. Due to the inability to use nourishment from feeding, it has been recommended that G-Tubes should not even be supplied in the circumstances such as anorexia caused by advanced cancer (Rajan et al., 2022). In cases such as an irreversible vegetative state, a G-Tube may be provided; however, it is not encouraged due to the participant’s inability to enjoy any kind of life. If, on the other hand, the person has effortless dysphagia and a generally maintained standard of life, a G-Tube should be provided and encouraged due to its clear nutritional advantage.
In addition, in cases of cancerous gastrointestinal blockage, G-Tube ventilation offers a distinct clinical advantage. In the case of equivocal signs, such as repeated seizures, decision-making is particularly challenging and might contribute to judgment remorse among proxy decision-makers (Rajan et al., 2022). Dislodging frequently implanted G-Tubes in elderly or neurologically impaired individuals imposes an immense monetary expense on the healthcare system. The placement of a gastrostomy in such individuals improves the caretakers’ health-related life satisfaction more than the clients’, ostensibly due to the simplicity of medicine administration and the caregiver’s increased sense of success (Rajan et al., 2022). The technique may bring physiological benefits in the form of a longer lifespan, but it may not enhance the quality of life. A small feeding trial can be addressed, but stringent criteria for what comprises a favorable reaction to food should be developed with the patient or their healthcare representative.
Conclusion
In conclusion, a G-Tube is an enteral feeding gadget implanted in the client’s stomach endoscopically, radiologically, or surgically. When giving medication using a G-Tube, the fundamental objective is to maximize the medication’s physiological action without compromising enteral feeding. Regardless of the therapeutic scenario, the placement of a G-Tube to give nutrients and bypass obstruction is often indicated. Certain conditions, like stomach volvulus, may necessitate using a G-Tube during gastropexy treatment. However, the G-Tube is advised for individuals with diseases necessitating more weeks of enteral nutrition supplementation. Endoscopic G-Tube insertion, radiologic G-Tube position, and laparoscopic G-Tube administration are the three types of G-Tube insertion.
To respect human autonomy over presumptive beneficence, G-Tube placement should need the patient’s educated and aware consent. The healthcare insurance proxy appointed in the patient’s written will must consent if the individual cannot is unable. However, clinical indicators might launch the decision-making process, but they are rarely sufficient alone. The significance of social support in reducing G-Tube dependency should also be investigated. Given the inability to utilize nutrients from ingestion, it has been suggested that G-Tubes should not be provided in cases such as severe cancer-related anorexia.
References
Rajan, A., Wangrattanapranee, P., Kessler, J., Kidambi, T. D., & Tabibian, J. H. (2022). Gastrostomy tubes: Fundamentals, periprocedural considerations, and best practices.World Journal of Gastrointestinal Surgery, 14(4), 286-303.
Shellnutt, C. (2019). The evidence on feeding initiation after percutaneous endoscopic gastrostomy tube placement.Gastroenterology Nursing, 42(5), 420-427.
Yasin, J. T., Schuchardt, P. A., Atkins, N., Koch, D., Davis, R. M., Saboo, S. S., & Bhat, A. P. (2020). CT-guided gastrostomy tube placement: A single center case series.Diagnostic and Interventional Radiology, 26(5), 464-469.