The structure of the male and female reproductive systems
Include a diagram for each of the two systems. For the structures given below explain structure to function points.
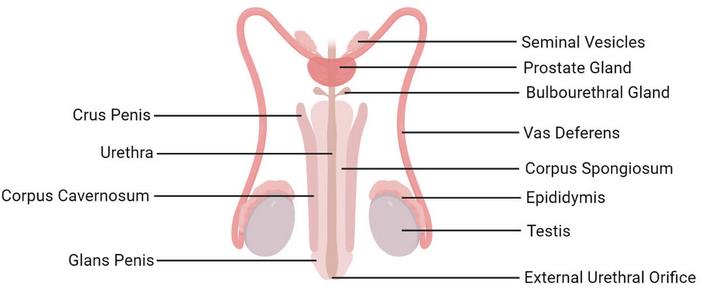
Functions of male reproductive system
Testis
They are the oval-shaped organs in the scrotum which are secured by the spermatic cord and are usually two in most men. The main functions of the testes are to produce testosterone which is main male sex hormone and generating sperm (Sapkota 2021).
Epididymis
The epididymis refers to the long, coiled tube at the back of the testicles. Their main function of the epididymis is transporting and storing sperm cells produced by the testes. It also ensures sperms are up to maturity before they can be released (Sapkota 2021).
Vas deferens
It is a long, muscular tube, which runs from the epididymis, to the pelvic cavity behind the bladder. Its main function is to transport mature sperms to the urethra which removes urine and sperms (Sapkota 2021).
Scrotum
The scrotum is a pouch-like sac of skin which usually hangs behind and below the penis. It holds the testicles or testes besides many blood vessels and nerves (Sapkota 2021). The scrotum provides a climatic control system for the testes by keeping the testes temperature slightly cooler than the body temperature to increase sperm count and quality.
Prostate gland
It is a walnut sized structure located below the urinary bladder in front of the rectum. The prostate gland contributes additional ejaculation fluid which also helps to nourish the sperm (Sapkota 2021).
Seminal Vesicles
These are sac-like pouches attached to the vas deferens at the base of the bladder. They produce a sugar-rich fluid called fructose which provides energy to the sperm for movement. The seminal vesicles fluid makes up the most volume of the ejaculatory fluid (Sapkota 2021).
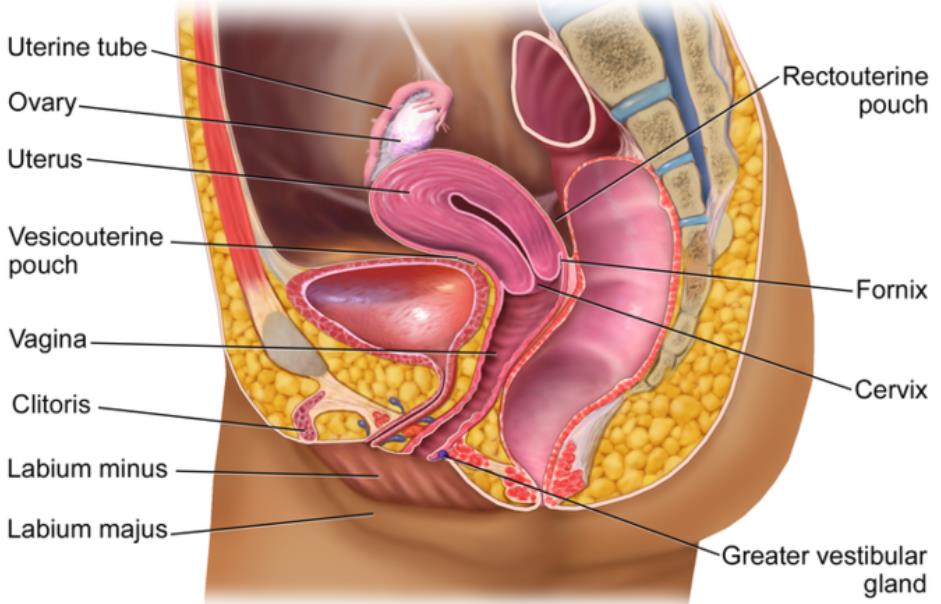
Functions of female reproductive system
Ovary
The ovaries are small, oval-shaped glands found on the either side of the uterus. They are responsible for producing eggs also called the ova. They also produce the main female sex hormones (oestrogen and progesterone) which are released to the bloodstream.
Fallopian tubes
These are narrow tubes attached to the upper part of the uterus in the female reproduction system. They are the tunnel in which ova travel from the ovaries to the uterus. The fertilization of the egg by the sperm or conception takes place in the Fallopian tubes.
Uterus
It is also called the womb, which a hollow, pear-shaped organ which acts as development home for a foetus. It consists of the cervix and the corpus. The corpus enlarges or expands with the help of myometrium to hold a developing baby.
Cervix
The cervix is the lower part of the uterus which opens into the vagina.
Vagina
It is the area between the cervix or the lower part of the womb and the outside of the body. The main function of the vagina is to receive the penis during intercourse and providing the passageway for childbirth (“Embryonic Development,” 2021).
Describe one function, brought about by the process of meiosis that spermatogenesis and oogenesis have in common
Please write the similarities between spermatogenesis and oogenesis in a paragraph rather than a table.
Spermatogenesis and oogenesis are similar in some ways of the gametogenesis processes. In both processes, the progenitor cell for spermatogonia and oogonia is the stem cell. They both experience meiosis type of cell division during gametogenesis. Meiosis refers to the process where a single cell divides twice to produce four cells containing half the original amount of genetic information (“Differences between spermatogenesis and oogenesis,” 2021). The spermatogenesis cells are the sperms while oogenesis cells are the ova which results in a haploid type of cells after meiosis. Haploid refers to a quality of a cell or organism having a single set of chromosomes. The spermatogenesis and oogenesis processes are both completed in three phases – multiplicative, growth, and maturation phases.
Describe how the end product cells of spermatogenesis and oogenesis differ
Write a paragraph on the differences between spermatogenesis and oogenesis. You can use the resource listed below for reference.
Spermatogenesis and oogenesis occur in different individuals hence they differ right from the definition. Spermatogenesis refers to the production sperms from spermatogonia while oogenesis refers to the production of ovum from the oogonia (“Differences between spermatogenesis and oogenesis,” 2021). Spermatogenesis occurs in the testis in males while oogenesis occurs in the ovaries of females. While all stages of spermatogenesis occur in the testis, the last stage of oogenesis occurs in the oviduct. Millions of sperms are produced every day in the testis while one ovum is produced per month by the ovary. This implies spermatogenesis takes place daily while oogenesis takes place once in a month. The resulting sperms in spermatogenesis are motile while ova from oogenesis are not. Equal cytokinesis producing four sperms in spermstogenesis while unequal cytokinesis in oogenesis producing one ovum and four polar bodies.
Name THREE hormones involved in the control of the female menstrual cycle and describe their function
List three hormones and state what their function in the menstrual cycle are.
Please write three separate paragraphs, one for each hormone and its function in detail.
The first hormone involved in the control of the female menstrual cycle is the Follicle Stimulating Hormone (FSH). FSH stimulates the follicular growth in ovaries through stimulation of development of egg cells or ova in the follicles. It also stimulates estrogen secretion from the developing follicles (“Menstrual cycle,” 2021). The overall function of the FSH is to ensure the maturation of the egg or ovum in the ovary.
The second hormone involved in the female menstrual cycle is the Luteinizing Hormone (LH) secreted in the pituitary gland. The surge of the LH causes ovulation in the ovaries once the ovum is mature. LH plays a very important role in ova development, ovulation induction, and stimulation of estradiol and progesterone production. The LH generally stimulates the release of the egg and results in the formation of a corpus luteum.
The third important hormone involved in the female menstrual cycle is the estrogen hormone produced by ovaries. Estrogen is responsible in the thickening of uterine lining or the endometrium. It also inhibits FSH and LH for most part of the cycle and also stimulates FSH and LH release pre-ovulation. Estrogen helps in endometrium regrowth, ovulation, and calcium absorption. It is generally involved in repairing and thickening the uterus lining. It is maintained by the progesterone hormone which inhibits FSH and LH. The drop in oestrogen and progesterone signals shed of endometrium layer resulting in menstrual bleeding.
Summarize the timeline of events in embryonic and fetal development
- Add a diagram to show the stages of fetal development.
- Name the three stages of fetal/prenatal development (Germinal, Embryonic and foetal)
- Explain the major events in each stage.
- The process of child development or prenatal development occurs in three main stages as shown in the Figure 3 below.
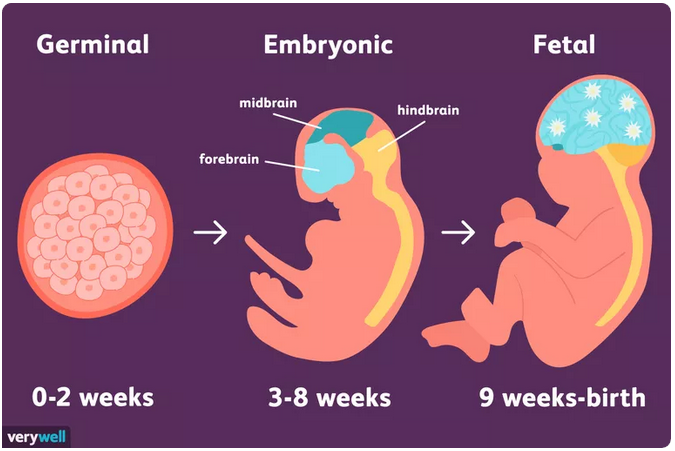
The germinal stage starts at the conception stage when fertilization occurs in the fallopian tube by the union of the sperm and egg cell. After fertilization, the fertilized egg becomes a zygote and starts to move down to the uterus via the fallopian tube. After 24 to 26 hours upon conception, cell division begins through the process of mitosis where the zygote divides into two cells, then four, eight, sixteen, and so on in a process called cell differentiation (“How a baby develops during the prenatal period,” 2021).
The continued cell multiplication results in two distinctive masses where the outer cells become the placenta while inner cells form the embryo. Rapid cell division occurs throughout the week-long journey to the uterus forming a blastocyst. The blastocyst is made of the ectoderm which develops into the skin and the nervous system, the endoderm which develops into the digestive and respiratory systems, and the mesoderm which develops into muscle and skeletal systems. The blastocyst reaches the uterus and attaches to the uterine wall in a process called implantation which results in hormonal changes halting the normal menstrual cycle and physical body changes.
In the embryonic stage, the cell masses become the embryo at the beginning of the third week after conception when the cell mass becomes distinct as human. The cell masses become distinct as a human hence the stage becomes an important brain development stage (“How a baby develops during the prenatal period,” 2021). The neural tube forms approximately four weeks after conception. The neural tube later develops into the central nervous system with the spinal cord and brain. During the fourth week, the head begins to form, followed by the eyes, nose, ears, and mouth. The blood vessels which later becomes the heart start to pulse. The buds, which later develop into legs and arms, appear during the fifth week. The embryo shows all the basic organs except for the sex organs by the eighth development week. The basic structures of the brain and the central nervous system become fully developed by the end of the embryonic period.
The fetal stage occurs in the period where most cell differentiation is complete and a fetus is formed. The stage is characterized by brain development, gross change, and growth during the ninth week through to birth (“How a baby develops during the prenatal period,” 2021). All body systems and structures formed during the embryonic period continue to develop. The neural tube develops into brain and spinal cord and neurons which move to their correct positions as time goes by. The fetus begins to make reflexive motions with their arms and legs between the ninth and twelfth week (“Embryonic development,” 2021). Sex organs form during the third month hence all organs become formed by the end of the third month. Between the fourth and sixth months, the heartbeat grows stronger and other body parts become fully formed. The brain begins to mature around week 23 as the fetus continues to develop, put on weight, and prepare life outside the womb between the seventh month and birth.
Explain the relationship between structure and function of the placenta
Add a diagram of Placenta.
The diagram in Figure 4 below shows a diagram of the structure of placenta.
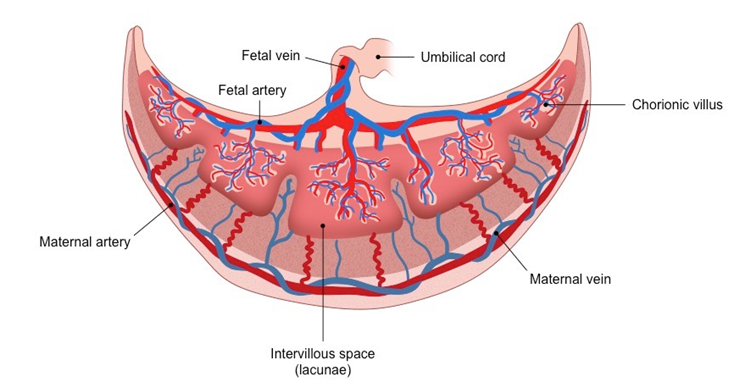
Explain how the placental structure is suited to carry out its function.
The placenta refers to structure which establishes a strong connection between the fetus and the mother. It facilitates the exchange of materials between the fetus and the mother and also secretes hormones for maintaining pregnancy upon degeneration of the corpus luteum. It is disc-shaped to increase the surface area for the exchange of materials between the mother and the fetus. It is thin, with a mature one 3cm thick hence reducing the distance in which materials travel from mother to the fetus (“Placenta,” 2021). The outer surface of the chorion is made of finger-like projections called chorionic villi, which grow into the tissue of the uterus. The villi penetrate the tissue of the uterine wall of the mother, ensuring faster and rapid transfer of materials between the mother and the fetus.
Explain the importance of the changes to the fetal circulation, lungs and liver in the readiness for birth
Add a diagram to show the fetal condition.
The diagram in Figure 5 below shows the circulation of blood in the fetus.
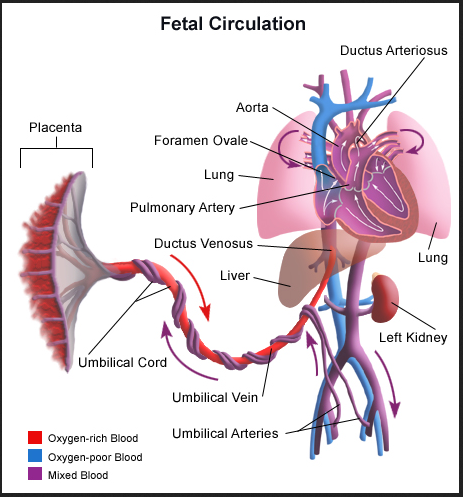
In three separate sections, circulation, lungs and liver, explain how the differences between the environment in the womb and the environment after birth mean, in later stages of fetal development certain preparations need to be made for before birth.
Circulation
The circulation of blood in the fetus occurs through the placenta where oxygenated blood penetrates to the fetus while blood with carbon dioxide moves from the fetus to the mother via the same placenta (“Stanford Children’s Health,” 2021). Most of the blood from the mother goes to the fetus heart and then flows through the body.
Lungs
The lungs of a baby are filled with fluid at birth; they are not usually inflated. The baby takes the first breath approximately 10 seconds after birth. The first breath is usually in the form of a gasp as the baby’s central nervous system reacts to the sudden change in temperature and environment. On the first breath, oxygen is increased in the lungs causing a decrease in blood flow resistance to the lungs (“Stanford Children’s Health,” 2021). The baby’s blood flow resistance also increases. The lungs inflate and start working on their own.
Liver
The liver in the baby acts as a storage site for sugar or glycogen and iron. Upon birth, the baby’s liver produces substances which help clot blood, starts breaking down waste products like excess blood cells, and also produces a protein which helps beak down bilirubin (“Stanford Children’s Health,” 2021). Proper break down of bilirubin is very important as it can lead to newborn jaundice.
Complete the table of the changes to fetal circulation lungs and liver before and after birth like the one below.
Identify and explain the function of the stages of birth
Add a diagram to show each stage.
The diagram in Figure 6 below shows the three main stages of childbirth.
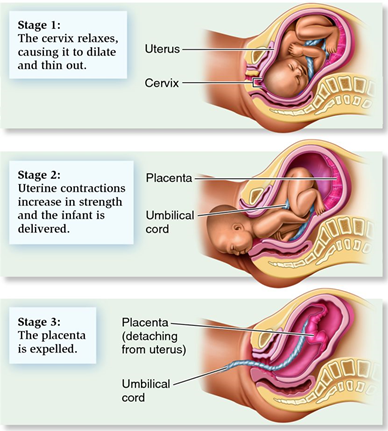
List the stages of birth and explain what the function of each stage is.
The first stage of birth is when contractions gradually open up the cervix or the neck of the womb or uterus. It is accompanied by early labor, active labor and the transitional phase. The cervix dilates or opens so the baby can be born (“The stages of childbirth,” 2021). The oxytocin hormone stimulates the contractions that help dilate the cervix, moving baby out of birth canal, pushing the placenta out, and limiting bleeding of the placenta. Womb muscles tighten upon contractions and release, drawing the cervix at the lower section of the womb. The early phase of the first stage shows the gradual opening of the cervix; the active phase is associated with 4cm dilation of the cervix and longer, frequent and stronger contractions, while the end of the first stage exhibits intense labor and the urge to push.
The second stage of birth is when the mother pushes out the baby, and the baby is born. The baby starts to move down the birth canal or the vagina. The mother may have the urge to push with the contractions, but they may be passive. When the baby descends though the birth canal and can be seen by the midwife, the stage is called an active second stage. During the stage, the pressure of the baby down can be felt in the pelvis (“The stages of childbirth,” 2021). The baby moves further through the pelvis upon more contractions, push, and release. The pelvic muscles gradually stretch with continued push until the baby’s head is visible at the vagina entrance. The midwife signals the mother to stop pushing to ensure the baby is born gently and slowly. The second stage ends once the baby is birthed, wiped, and placed on the tummy or chest for a skin-to-skin cuddle.
The third stage of birth or labor is when the placenta is delivered. It begins with the birth of the baby and ends when the placenta is delivered together with the empty bag of water attached to the placenta (“Stages of labor q,” 2021). An injection may be offered by the midwife to help contract the womb down and the placenta to come out. Few minutes after a managed or natural third stage, the midwife continues with clamping of the cord. The process ends when the midwife does the standard newborn checks such as baby weight, head size, and temperature.
References
The stages of childbirth. (2021). Web.
Embryonic development: Anatomy and physiology II. (2021). Web.
The female reproductive system: Boundless anatomy and physiology. (2021).
Menstrual cycle. (2021). BioNinja. Web.
Placenta. (2021). BioNinja. Web.
Stages of labour. (2021). Web.
Sapkota, A. (2021) Human male reproductive system: Organs, structure, functions. Web.
Stanford Children’s Health. (2021). Web.
Differences between Spermatogenesis and Oogenesis. (2021). Web.
How a baby develops during the prenatal period. (2021). Web.
Blood Circulation in the Fetus and Newborn. (2021). Web.