Plan to Implement the Change
Performance Improvement Model
The most feasible performance improvement model for the project at hand is the PDSA (Plan-Do-Study-Act) cycle. According to this model, the first phase of change is a series of steps intended for outlining the intended intervention. Thus, the first necessary step is the assembling of the team responsible for the project. As was explained in the previous part, patient fall rate depends on many factors that cannot be addressed by targeting a single aspect of health care.
Thus, the team should include professionals from different disciplines. For instance, to understand the influence of nursing activities relevant to the issue, it would be beneficial to include nursing practitioners and, possibly, physicians. Next, pharmacists are desirable members of the team since at least some of the falls are associated with medication issues. Finally, a project leader with the necessary interpersonal skills and relevant experience should be included.
The second step is establishing the metrics that will be used to determine the success of the project. The most relevant parameter is the occurrence of falls in the Carolinas Healthcare System’s facilities. Thus, it can be adopted as a primary determinant of success. Other parameters, such as the proportion of falls resulting in injuries and the mortality rate associated with the phenomenon can be included if considered within the scope of the project.
As a part of this step, the estimation of the financial outcomes associated with the project’s implementation may be necessary. The reduction in falls will likely result in the reduction of the expenses caused by the need for additional care. Thus, it will be necessary to identify as many potential improvements as possible and suggest a probable outcome based on the estimated savings.
In the third step, the probable causes of the falls need to be identified and, if possible, weighted to illustrate their relative contribution to the issue. This step is necessary to ensure that the direction chosen by the team will produce favorable results. This assessment can be done using visual aids such as cause and effect diagrams and may require an in-depth inquiry to collect the relevant information. Finally, based on these findings, the team will need to draft the intervention that would provide the desired change. In addition, it would be necessary to determine the scope of the intervention’s implementation. The intervention can be selected based on the evidence of its effectiveness from the academic literature and adjusted by the local conditions.
Once all planning is completed, it is possible to execute the intervention. Importantly, the supervision of the project is to begin simultaneously as required by the PDSA cycle (Taylor et al., 2014). Once sufficient data is gathered, it is then possible to proceed to study the project’s impact. The success will be determined by matching the data to the predetermined milestones. In the case when the milestones are not met, the components of the intervention are inspected to detect the discrepancies. Once the issue is spotted, the intervention is adjusted and reintroduced in an updated form. The cycle continues until the consistency in the outcomes is demonstrated and the change is considered sustainable.
Human and Financial Resources
As was explained above, a balanced team is necessary for the successful completion of the project. The body of the unit will be comprised of the specialists directly involved in the delivery of the practices selected as the intervention components and will include nursing practitioners, clinicians, pharmacists, therapists, and certified nursing assistants, among others. In most cases, it will be possible to assign roles to these team members based on their formal areas of proficiency whereas in some instances, informal experience obtained in the setting may be considered (Renedo, Marston, Spyridonidis, & Barlow, 2015). In addition, several team members will be assigned managerial roles. Their responsibilities will include internal and external communication, resolution of conflicts, progress auditing, and reporting.
The budget necessary for the project will be primarily allocated to the resources for ensuring patient safety and will include the costs of staff education and training, the salaries for project coordinators, and the purchase of equipment in the case when the current state of the facility is considered incompatible with the required level of patient safety (Spetz, Brown, & Aydin, 2015). Given the size of the facility and estimated savings resulting from the project’s success of approximately $30,000, it is possible to suggest a budget of approximately $4,000. In this case, the ROI (return on investment) will be 30,000 – 4,000 / 4,000 = 6.5.
Goals
The ultimate goal of the project is the reduction of adverse effects related to falls among the patients of the facility. However, since the project is focused on the occurrence of falls rather than their outcomes, it would be more appropriate to use this metric as a primary determinant of success. To meaningfully assess this variable, it is recommended to use the proportion of the registered falls among the patients as well as the number of falls per certain amount of bed days. For the project, a fixed number of 1000 patient bed days is recommended since it allows comparing the outcome with the results reported in the academic literature.
After this, the results can be arranged in graphic format to detect trends. A positive trend comprised of four data points can be considered an indication of success. However, due to the complexity of the issue, a certain amount of inconsistency is expected throughout the evaluation process. Therefore, the median needs to be calculated based on the baseline measurements. Once five or more data points form a median that is lower than the initial one, the project can be considered a success.
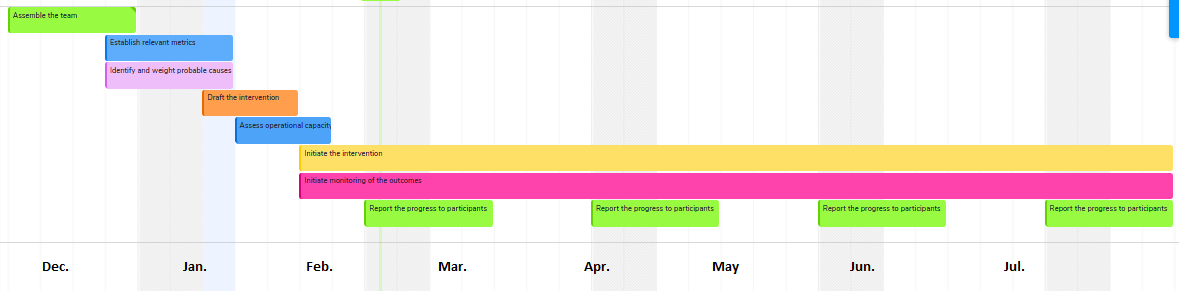
Gantt Chart
Roles of Stakeholders
The stakeholders involved in the process include the team members, the staff of the facility, and the patients and their families. The roles of the latter are limited to participation in the educational programs intended to increase their proficiency with the newly introduced equipment and minimizing the risk of falling both in the hospital setting and at home.
The role of staff members will include the assessment of risk, documentation of the fall prevention practices, reporting the issues, educating the patients, adjusting practices by the reports, and performing care-related tasks. The roles of the members with specific responsibilities (e.g. pharmacists) will include the review of the medication lists and their adjustment by the goals. The role of the team members includes processing and analyzing the data, investigating the inconsistencies and shortcomings, adjusting the intervention, and communicating with the staff.
Plan to Evaluate the Change
Evaluation Plan
The first step of the evaluation process involves the measurement of the operational capacity of the project. To confirm the readiness of the staff for the facilitation of the intervention, the assessment of the initial state of the process must be performed. At this stage, the team will assess the proportion of the unit employees familiarized with the falls prevention program, the proportion of the patients assessed for the risk of falls by the staff, the percentage of the staff members and/or patients who are satisfied with the project and considering it a positive change, and the frequency and consistency of using the fall prevention strategies introduced by the project. This step is necessary to confirm the feasibility of the project, detect the inconsistencies early in the course of its implementation and make the necessary adjustments.
Once the feasibility of the process is validated, it is possible to proceed to the second step – the measurement of the outcomes – the incidence of falls, the proportion of the registered falls among the patients, and the number of falls per 1000 bed days. It is important to note that during the initial phase, the results obtained at this stage are unlikely to be positive. It is reasonable to expect a slight increase in the proportion of patient falls due to the greater awareness of the issue and the increased staff engagement (Morgan et al., 2017).
In addition, some of the intervention’s elements are more effective in the long run and will not produce a statistically significant effect in the short term (Miake-Lye, Hempel, Ganz, & Shekelle, 2013). Finally, it should be noted that since the reporting of the falls is voluntary, the resulting data may not be representative of the issue. It will thus be necessary to create a workplace culture where the reporting of falls is considered a positive contribution rather than a reason for punitive actions.
Once the data is obtained and processed, the results need to be communicated to the stakeholders in the third and final step of the evaluation process. By the PDSA cycle, the information must be available on a timely basis and in an accessible form to ensure the appropriate response. It should be understood that while some metrics (e.g. the rate of falls per 1000 bed days) provide a more accurate and reliable assessment, it may be challenging and obscure to non-experts (Davis, 2014).
Therefore, more straightforward metrics can be used for this purpose (e.g. the total number of falls per month). In the situation where the results are inconsistent with the intended rate of success, it would be necessary to investigate its causes and formulate a response by adjusting the intervention. This step serves two purposes. First, it ensures a timely response from the team. Second, it motivates the participants by providing a sense of progression.
Indicators of the Problem
The indicators of the problem are the adverse effects associated with the issue of patient falls. The most readily recognized one is the injury caused by the fall. This indicator is also the most evident one since it requires reporting and is easily traceable in the medical records. This indicator is relevant primarily for clinicians and administrators due to its impact on the quality of care and patient satisfaction level.
The expenses associated with additional care necessitated by the falls constitute another important indicator. It is worth pointing out that this indicator is both quantifiable and reliably documented. However, it is relevant primarily on the organizational level and is thus a minor concern for the staff of the facility. Finally, the state of the workplace culture, as well as staff’s awareness of and preparedness for the issue, can be considered a meaningful indicator that determines whether the organization is susceptible to the issue. However, this indicator is not readily apparent and requires in-depth inquiry before the conclusions can be made.
Evaluation Criteria
The main criterion of the project is the number of falls occurring in the setting. However, representing the data in the form of total falls occurring in a certain time frame may create a distorted image. Therefore, the criterion can be presented as a rate of falls per 1000 bed days. This criterion can be calculated using a simple formula: number of falls per month / (daily number of patients x days in month x 1000 (number of bed days). As was mentioned in the previous section, it is reasonable to expect that the said rate may not be sufficiently indicative of the project’s success to the hospital staff.
Therefore, reporting the total number of falls is recommended in respective situations. Next, the proportion of patients assessed for the risk of falls is an important secondary criterion that illustrates the project’s progression. Finally, several intermediary criteria can be identified, such as the adherence to the fall prevention guidelines and the satisfaction with the program voiced by the staff and the patients. These criteria can be quantified using the data collection methods such as surveys and interviews.
Performance Improvement Tools
As can be seen from the description of the criteria, some of the data require specific tools for collection. Most notably, the perceived quality of the intervention can be reliably determined by using surveys and interviews. The former has an advantage of a relatively short time required for administration and data analysis and can be used for making snapshots of the project’s progress throughout its course. Modern digital tools offer a simple and streamlined collection process and can instantly compile the collected data into an approachable and visually appealing format. The interviews, on the other hand, require more time to process but may offer in-depth insights into the ways of optimizing the project. Thus, their use should be limited to specific cases.
Once the data is obtained, it should be converted into a visual format for tracking and trending purposes. The most suitable format for the rates of falls is a run chart. This tool is accessible for non-expert audiences and creates a sense of progression necessary for the engagement of stakeholders (Davis, 2014). The data obtained in the surveys can be represented in pie and bar charts, both of which are available through data collection tools.
Roles of Stakeholders
The evaluation process requires the coordinated action of all stakeholders. The nursing staff’s role is the collection of data from patients. In addition, it is expected that the staff can provide their feedback on the project, serving as a source of information. The roles of analyzing information, delivering it to the participants, and incorporating feedback into the intervention are distributed within the project team.
Implications and Conclusion
Patient falls remain one of the primary issues in the healthcare setting. The problem is especially relevant for the older segment of patients due to a variety of additional risk factors such as the loss of strength due to aging, the adverse effects of medications, and environmental hazards. In addition, the falls among older population facilitate a greater risk of severe injury and produce more complications (Ambrose, Paul, & Hausdorff, 2013). However, the most important aspect of the issue is its preventable nature. The majority of falls can be traced to the gaps in care delivery and inappropriate workplace culture.
The successful implementation of a project at hand is expected to provide an improvement in several areas. First, the reduction in falls will minimize the occurrence of the adverse effects associated with it, thus improving patient outcomes. By extension, the reduction in the need for extended care associated with fall-related injuries will reduce the workload and decrease the work-related stress, which is expected to have an indirect positive impact on the quality of care. Finally, the reduction in fall-related care and length of stay is expected to decrease both the operating cost of the facility and indirect costs associated with malpractice allegations (Cumbler, Simpson, Rosenthal, & Likosky, 2013).
It should be acknowledged that the issue of falls is complex and therefore, requires a coordinated effort of several stakeholders. In this regard, a nursing leader becomes an important player in the process. The leader’s roles include the establishment of communication between different groups of participants, reporting the results to the stakeholders, processing feedback for progress tracking, dealing with the emerging issues, and maintaining a healthy workplace culture. Thus, a nurse leader with relevant specialty competencies plays a key role in the project’s success.
References
Ambrose, A. F., Paul, G., & Hausdorff, J. M. (2013). Risk factors for falls among older adults: A review of the literature. Maturitas, 75(1), 51-61.
Cumbler, E. U., Simpson, J. R., Rosenthal, L. D., & Likosky, D. J. (2013). Inpatient falls: Defining the problem and identifying possible solutions. Part I: An evidence-based review. The Neurohospitalist, 3(3), 135-143.
Davis, K. (2014). Different stakeholder groups and their perceptions of project success. International Journal of Project Management, 32(2), 189-201.
Miake-Lye, I. M., Hempel, S., Ganz, D. A., & Shekelle, P. G. (2013). Inpatient fall prevention programs as a patient safety strategy: A systematic review. Annals of Internal Medicine, 158(5), 390-396.
Morgan, L., Flynn, L., Robertson, E., New, S., Forde‐Johnston, C., & McCulloch, P. (2017). Intentional rounding: A staff‐led quality improvement intervention in the prevention of patient falls. Journal of Clinical Nursing, 26(1-2), 115-124.
Renedo, A., Marston, C. A., Spyridonidis, D., & Barlow, J. (2015). Patient and public involvement in healthcare quality improvement: How organizations can help patients and professionals to collaborate. Public Management Review, 17(1), 17-34.
Spetz, J., Brown, D. S., & Aydin, C. (2015). The economics of preventing hospital falls: Demonstrating ROI through a simple model. Journal of Nursing Administration, 45(1), 50-57.
Taylor, M. J., Mcnicholas, C., Nicolay, C., Darzi, A., Bell, D., & Reed, J. E. (2014). Systematic review of the application of the plan-do-study-act method to improve quality in healthcare. BMJ Quality & Safety, 23(4), 290-298.