The human body weakens and deteriorates as a person advances in age beyond adulthood. One of the consequences of this deterioration is pain. Chronic pain differs from acute pain mainly by duration. There is no consensus regarding the duration but it generally falls somewhere between one and six months (Better Health Channel, 2011). Below this duration, the pain is acute, but beyond this duration, it becomes chronic. Some scholars classify pain between the first and sixth month as sub-acute. Chronic pain tends to last for more than a year especially among the older generation.
Age is one of the factors that increase the propensity of an individual to suffer from chronic pain. There is some sort of plateau phase observed among the older people in Victoria above the age of seventy, who do not seem to have any major difference with those slightly younger in their pain profiles. Research reports show that between 27% and 61% of people aged over 65 have chronic pains in Australia (Dewar, 2007). This variance in numbers is because of the difficulty in diagnosis of pain due to its subjective nature (Virir, 2009). Chronic burden also contributes up to 80% of the disease burden in Australia (National Health Priority Action Council, 2006).
Normally, as the human body ages, its capacity to deal with infection and to recover from injury diminishes. Certain conditions such as heart disease, kidney failure, liver problems, and other organ failures increase. In addition, old people tend to take a disproportionately longer time to recover from physical injury due to accidents. Chronic pain in the elderly in Victoria take the form of persistent headaches and migraines, back pains, limn and joint pains and gastrointestinal problems. However, older people above the age of seventy tend to have fewer cases of headaches as compared to younger age groups. Some also develop conditions causing them chronic pain in the ENT system. While these pains mainly affect to the elderly, they tend to be more concentrated among them.
The effects of chronic pain vary from person to person and take different forms. In a general sense, people show two main reactions to chronic pain. The first type of effect that chronic pain has on people is that it reduced the range of options they have relating to physical activities. In this sense, chronic pain limits their participation in physical activities such as sports, manual work and can significantly reduce their mobility. These activities tend to increase the awareness of the pain because of the increased potential for spikes in level of pain when people engage in physical activity. The second effect is psychological. Pain can result in social withdrawal and in some cases can lead to significant stress, paving way for depression. The continued presence of pain makes an elderly person more aware of the physical limitation they experience because of age and serves to limit them even further.
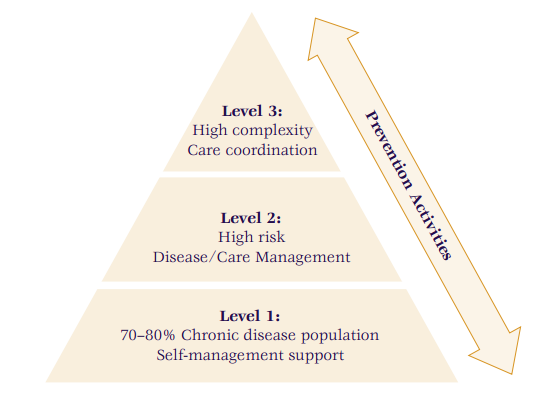
There are two general approaches to pain management available in Victoria. They include the use of drug based therapies (pharmacological) and secondly, the use of non-drug interventions (non-pharmacological) (Better Health Channel, 2011). Drug based therapies generally involve the use of painkillers such as Paracetamol, aspirin, Opioid drugs and local anesthetics (Kumar, 2007). The option used depends on the facts of the case, and the severity of the pain as shown in figure 1.
Non-drug interventions include the use of physical therapy such as exercise, massage, and acupuncture, among many others. These options work for patients who cannot use drugs or are not responding to drugs. It may also be a choice as an alternative to drug based therapies.
References
Better Health Channel. (2011). Pain Management – Adults. Web.
Dewar, A. (2007). Assessment and Management of Chronic pain in the Older Person Living in the Community. Australian Journal of Advanced Nursing , 24 (1).
Kumar, N. (2007). WHO Normative Guidelines on Pain Management: Report of a Delphi Study to Determine the Need for the Guidelines and to Identify the Number and topics of Guidelines that Should be Developed by WHO. Gevena: World health organization (WHO).
National Health Priority Action Council (2006). National Chronic Disease Strategy. Canberra: Australian Government Department of Health and Ageing.
Virir. (2009). Pain Assessment and Management in Residential Aged Care. Victoria: Vivir Healthcare Pty Ltd.