Introduction
Wartime operations continue to ravage the world, so uncovering more effective health service delivery in crisis conditions is quintessential. This paper aims to evaluate the problems that military medical personnel may face in combat zones. Therefore, the research question for this paper asks in what ways are military medical personnel prevented from serving their duty in active conflict regions. The following objectives were set: identifying critical obstacles in healthcare delivery in a combat context (RQ1); exploring the challenges healthcare workers encounter in their daily operations (RQ2). Overall, shortages in supplies, staffing, inappropriate infrastructure, increased insecurity, and even direct attacks on personnel prevent the providers from delivering healthcare to patients.
Materials and Methods
Relevant scholarly literature sources were obtained using school library databases and search engines like PubMed, Google Scholar, and others. Recent works (published no earlier than five years ago) were selected and reviewed for this study. Primary common themes were then identified, and the literature was organized and synthesized according to the related subjects: violence against medical personnel, practicing in a conflict setting, ethics, and mental health.
Results
Violence Against Health Workers
One of the most widely discussed topics regarding the operational flow of healthcare delivery in a military setting concerns attacks on healthcare staff and the facilities at which they work. Some may be less destructive, like blocked roads or checkpoints that may delay or stop the movement of ambulances (Patel et al., 2017). Some are direct and harmful: the armed attacks on the healthcare providers, patients, or resource providers outside of hospitals or entry to the facilities; unfriendly fire targeting the health facilities directly (Patel et al., 2017). Thus, these attacks may be intentional or not and vary drastically in manifestations.
Practicing in Conflict Setting
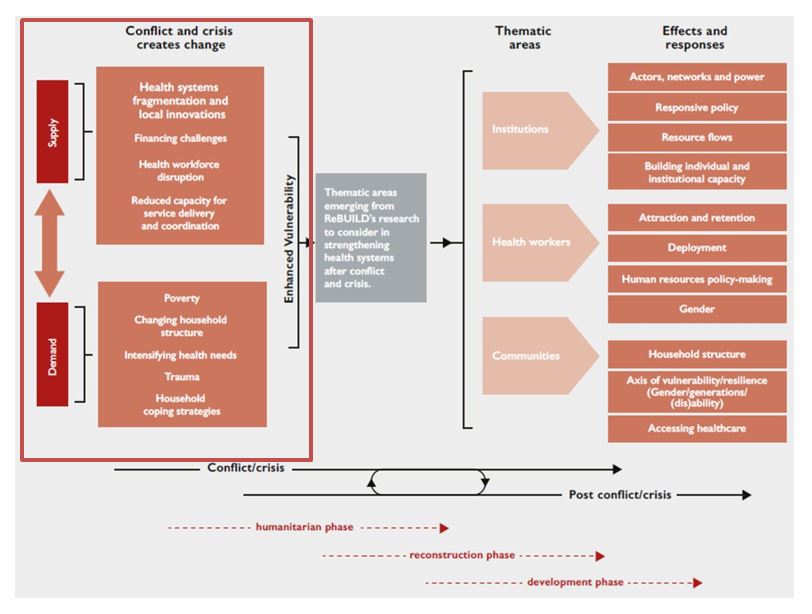
One of the significant challenges of healthcare delivery is the impairment of providers’ ability to provide quality care. This challenge may arise out of various circumstances and their combinations (Pic. 1). Discussed below are the most common factors, such as the destruction of infrastructure, barriers between patients and providers, and patient distribution.
Infrastructure Breakdown
The first type of obstacle that the healthcare staff face is related to the organization of the health system in the areas of humanitarian crisis. The parties participating in an armed conflict may destroy or significantly damage the infrastructure required for health delivery (Debarre, 2018). This destruction not only deprives the staff of physical spaces to operate safely – it leads to medicine, supplies, staff, and finance deficits (Debarre, 2018). Often, medical staff struggles to provide appropriate care since essential items like “oxygen, gloves, gauze, cotton, stethoscopes, cannulas, anesthesia, and antibiotics” are absent (Elnakib et al., 2021, p. 5). The healthcare systems already stretched thin due to a large volume of incoming patients are further burdened by those shortages.
Patient-Provider Barriers
Second, armed conflict puts the barriers between the medical personnel and the populations in need of their services, making it much more challenging to reach each other. The barriers’ nature may be physical, like the destroyed or heavily patrolled streets due to increased security. The barriers may also be legal and administrative: healthcare systems may be militarized or politicized; poor authority may lead to ineffective operational flow; extant workers may be displaced (Debarre, 2018). Lastly, the trust barrier may be created when patients blame the providers for not having enough supplies and accuse them of stealing or concealing vital supplies (Elnakib et al., 2021). The resulting tensions and mistrust may compromise the healthcare delivery process.
Patient Distribution
Another challenge of operations during wartime relates to patient intake. Healthcare centers may experience a cyclical pattern in the influx of patients with certain types of trauma (Bouchet-Saulnier & Whittall, 2018). Patients, predominantly with violent trauma, come in waves, which often requires emergency care and surgical treatment for many at once (Bouchet-Saulnier & Whittall, 2018). In times of slower influx, the providers may focus more on stabilizing and normalizing patients’ states; full recovery is rarely made in the warzone hospitals (Bouchet-Saulnier & Whittall, 2018). Since several patients require the same treatment at once the same members of the medical team may be excessively overwhelmed.
Ineffective Aid
The organization is another challenge that the healthcare system may experience that subsequently has implications for regular workers. Friendly states’ funding they provide may be insufficient, securitized, or short-lived, which causes difficulties with the purchases of appropriate materials or equipment (Debarre, 2018). Moreover, the aid may not always align with the needs of the local healthcare system: for instance, providing supplies for the equipment that local hospitals do not have or providing supplies that are not in shortage (Debarre, 2018). Overall, the short-lived and ineffective aid may undermine healthcare delivery operations.
Ethical Issues
One of the most prominent differences in operation on the battlefield versus operating in non-combat circumstances is the reversed resource allocation. Typically, those with the gravest injuries are ethically required to be prioritized in hospitals as they need the most urgent and extensive care (Kenny & Kelley, 2019). However, operating in the conflict context often requires medics to be as resourceful as possible, focusing first on those with the highest chances and avoiding any ‘waste’ for the severely injured (Kenny & Kelley, 2019). While specialized army personnel may be more accustomed to operating under such conditions, war induces the need for all medical practitioners to operate under such circumstances. Making those decisions can be incredibly difficult for the personnel since it is the opposite of the usual care delivery paradigm.
Mental Health
Working under warzone conditions places increasing pressure on providers’ mental health. The surge in patient demand, and service disruption, coupled with lack of support, results in the providers feeling powerless and unable to provide as good care as they could in better conditions (Elnakib et al., 2021). Another challenge that military medical personnel experienced was the requirement to provide equal care to all, even the assailants (Kenny & Kelley, 2019). The contradicting feelings, frustration, and lack of safety may be severely detrimental to operations.
Discussion
Healthcare workers encounter many constraints in operating in active armed conflict zones. Many of the challenges are pertinent to both specifically trained army doctors and those who have been converted from civil practitioners after a war commenced in their region. Some obstacles to warzone healthcare delivery included limited supplies, broken or absent appropriate equipment, or lack of appropriate medications. These factors may impair the ability to treat patients effectively even if personnel are available. Additionally, the barriers may be put between the providers and the patients, whether physical, legal, or personal. Physical ones limit the ability to get to the patient, the ineffective operational flow may compromise treatment effectiveness, and the lack of trust may preclude patients from obeying providers. One of the most direct ways providers are prevented from doing their jobs is the lack of personal safety, compromised by violent attacks on staff. Therefore, the RQ1 regarding critical obstacles is answered by finding obstacles in movement, operations, and communication of healthcare workers.
As a result of being severely deprived of suitable infrastructure and resources, the strain on the already compromised system of healthcare delivery increases. Friendly states’ humanitarian aid is at times sporadic, unreliable, or not the type needed most in the specific scenario. These issues are often compounded because patients’ influx increases drastically, and most of them are severely wounded, while other illnesses do not disappear either. As a result, military medical personnel had to prioritize which patients should be put first, often going against the principles ingrained in them during the civil time. Thus, overcoming the excessive workload, navigating tension and violence, and providing equal care for all are significant challenges that military medical professionals confront in the field.
Conclusion
Operating in a situation where personnel safety is compromised, working conditions are dire, supplies are lacking, humanitarian aid is politicized, and the system is overwhelmed causes an enormous strain on the providers. The last challenge that the providers have is performing these tasks while attempting to take care of their mental and physical health. Having to care for the opposite side fighters or making choices in survival is tough for many providers. Therefore, the RQ2 regarding critical challenges is answered by evaluating the effects of violence, overworking, difficult prioritization choices, and balancing self-care with caring for others on the medical staff.
References
Bouchet-Saulnier, F., & Whittall, J. (2018). An environment conducive to mistakes? Lessons learnt from the attack on the Médecins Sans Frontières hospital in Kunduz, Afghanistan.International Review of the Red Cross, 100(907–909), 337–372. Web.
Debarre, A. (2018). Hard to reach: Providing healthcare in armed conflict (pp. 1–32). International Peace Institute.
Elnakib, S., Elaraby, S., Othman, F., BaSaleem, H., Abdulghani AlShawafi, N. A., Saleh Al-Gawfi, I. A., Shafique, F., Al-Kubati, E., Rafique, N., & Tappis, H. (2021). Providing care under extreme adversity: The impact of the Yemen conflict on the personal and professional lives of health workers.Social Science & Medicine, 272, 1–10. Web.
Kenny, D. J., & Kelley, P. W. (2019). Heavy burdens: Ethical issues faced by military nurses during a war.The Online Journal of Issues in Nursing, 24(3). Web.
Martineau, T., McPake, B., Theobald, S., Raven, J., Ensor, T., Fustukian, S., Ssengooba, F., Chirwa, Y., Vong, S., Wurie, H., Hooton, N., & Witter, S. (2017). Leaving no one behind: Lessons on rebuilding health systems in conflict- and crisis-affected states.BMJ Global Health, 2(2), 1–6. Web.
Patel, P., Gibson-Fall, F., Sullivan, R., & Irwin, R. (2017). Documenting attacks on health workers and facilities in armed conflicts.Bulletin of the World Health Organization, 95(1), 79–81. Web.