Executive Summary
Social entrepreneurship involves business activities that are characterized by numerous charitable activities. This kind of a business is tied to primarily social objectives and not geared towards achieving profits. In the event that the business makes surplus profits, the excess is reinvested in the business or better still in the community as opposed to profits benefiting the shareholders.
The proposal addresses poor people’s needs to access better health care services making use of information and communication technology processes. E-Health social enterprise is anchored on the key assumption that health management, information and communication technology are very crucial to the poor members of the society, just like other basic needs.
Members of the society who are not computer literate need to learn and embrace the tools of information and technology in the health care services. E-Health provides the poor members of the society with quality and affordable health care services and addresses the environmental problems affecting them and generally cuts down the level of poverty in various parts of the world.
Social and Business Justification
Africa is a continent where most of the nations are very poor and it will not be contradictory to state that it is the most deprived one, with nine of the ten most deprived countries being its part (Ali, 2010). Our e-health programme is intended to help people of such countries. But initially, we will be targeting people from Namibia and Botswana. We plan to make use of the internet facility in delivering our services. Through internet, we will be able to reach out to several people at a time. This will be done through social networking sites like Facebook, Twitter and LinkedIn.
The benefit of using such sites is that even though we may contact only one person but indirectly, we will be reaching out to numerous people because the communications made will be available for anyone and everyone to read (Carr, 2001) Apart from the financial help, the people of Africa also urgently need medical aid. Their living conditions are very unhygienic and as such, epidemics keep on erupting. So a plan based on doing something towards improving the living conditions seems to be a better option.
Social Performance Target
E-Health plans to reach out to the maximum possible natives of two developing countries of Africa by the first year of its operation. These two countries are Namibia and Botswana. If the E-Health social enterprise is successful in these two countries, then the plan can be applied to other developing countries.
With this plan, E-Health plans to design a conceptual model that takes into account mortality and morbidity considering economic, social and political forces that determine resource allocation and management among the poor community members. E-health plans to invest in database and website development. The e-Health database will provide a platform to offer the best quality healthcare services, referrals and maintaining repeat customers.
On the other hand, the website will make it possible to reach many desperate healthcare consumers across the globe (Reid, 1996, p.32). Evidence of the social end or environmental viability of the plan is supported by relevant case studies and theoretical frameworks and models.
Relevant Case Study
Vodafone e-Health case study for 2009 is relevant for this plan. The Vodafone case study focused on the areas of long-term health care management, healthy living and community clinics (Vodafone, 2010, p.1). Frameworks and models that support the integration of e-Health can be best analyzed by Freemium business model that allows the poor not to pay for the healthcare services offered to them, while the rich members of the society are charged highly for these services.
Evidence of Market, Technical, and Financial Viability of the Plan
These aspects can be analyzed through application of relevant case studies and theories. Like the Vodafone e-health 2009 case study, the plan is market viable in the sense that there are many poor people who are in great need of the social health care services.
This group of people would form a large market base for the e-Health social enterprise. Besides, e-Health is equipped with sound technical knowledge that makes it possible to reach many consumers across the globe at a faster rate. E-Health social enterprise would also manage to gather financial support from major financiers such as World Health Organization (WHO), United Nations Educational Scientific and Cultural Organization (UNESCO) and World Trade Organization (WTO).
In essence, health care delivery models that are clinically driven can be relevant for this plan because the information and communication technology tools are based on patient-centred care frameworks that make it possible to involve all the stakeholders in participative-decision making process. This ensures that financial resources are properly utilized since consumers who are involved in the decision making process are not likely to resist e-Health marketed services (Reid, 1996, p.29).
The Need and Requirements
Poor people from the developing world face problems such as lack of quality and affordable health care services. This is because, healthcare facilities may be located far away from their homes denying them easy access to modern medicine. As a result, most of them rely on traditional medicaments to counteract most of the ailments that they succumb to. Other problems include: lack of access clean water for domestic use, proper sanitation, good transport and communication networks and low levels of education (Field, 1996, p.49).
The majority of the most vulnerable people are located in the developing world, especially the African subcontinent. Due to that, the need for medication that is affordable to all will make it appropriate to establish an online social enterprise (E-Health). This E-health social enterprise will address health care problems in a wide geographical area since it is a global phenomenon that affects many people in the entire world and will mainly target the people of Namibia and Botswana in the African subcontinent.
Implementation Tools and Approach
To provide its services to the people, the E-health social enterprise will need a team of doctors, nurses, pharmacists, environmentalists, voluntary workers and even IT experts. If governments of various countries want to contribute, they can do so by providing the organization with doctors and other health experts. Medical facilities and services can be airlifted to the required areas since road transport networks are poorly developed in these areas (Tidd, 2010, p.49). This can be analyzed under the software, hosting and web service options among others.
E-Health can use File Transfer Protocol (FTP) and Web interface for enterprise web site hosting services. Comprehensive packages such as Java would be used to provide database support, and they can help in providing application development platforms that allow clients to write and install forum application scripts (Tidd, 2010, p.57).
The main element of our E-Health programme is communicating people around the globe. One of the better ways to make such communications is the open source application. There are several open source applications available on the internet. These open source applications facilitate communications with different people and allow mutual co-operation within groups (Chandler).
BitNami is one such open source application that is deployed to the GNAX cloud. Even though the service is nominally charged, the benefits are immense in the sense that we will be able to approach a bigger community. BitNami can be useful in providing E-Health consultations to the people of Namibia and Botswana and the people can also have the option of accessing health services and information related to various diseases.
It also has commercial application deployed in-house that can be chosen for e-health services. E-Health social enterprise plans to incorporate cloud computing in its data centre platform so as to get faster applications that are easier to manage and maintain. It will also facilitate the IT resources adjustment according to the unpredictable or fluctuating demands of the business (Field, 1996, p.62).
Vision, Mission, and Strategy
Here, the plan focuses on the targeted people of Namibia and Botswana, products/services offered and the means to deliver the offerings. The vision of e-Health social enterprise is to provide quality and affordable health care services to the customers.
The mission is to deliver timely and affordable health care services to the customers with the best efficiency and reliability and the strategy is to target the people of Namibia and Botswana in the African subcontinent in order to offer them quality and affordable health care services.
The services will be delivered online through internet websites and mobile phones, but customers who are located in remote areas can get airlifted medical services (Field, 1996, p.39).
The Impact/Social Performance Measures
Under this plan, the social performance measurement framework and social performance targets are analyzed. This includes double bottom line, triple bottom line and balanced scorecard, which can be used in this plan. Among these, social performance measurement frameworks, the most appropriate one for the enterprise is balanced scorecard (Reid, 1996, p.48). The marketing approach based on social performance target is the balanced score card.
Business Revenue Model
This part of the proposal analyzes some of the business and revenue models employed by the e-Health online social enterprise. E-Health online social enterprise plans to use tools such as the Business Model Canvas to create, deliver and capture values.
E-Health social enterprise plans to get funding from World Health Organizations (WHO) and donations from various Non-governmental organizations (NGOs). The enterprise will generate its revenue through medical fees and consultancy services. Other means of generating revenue for the enterprise include promotional campaigns using the firm’s website.
For instance pharmaceutical industries can promote their products in the website and in the process generate revenue for the organization (Field, 1996, p.47). Moreover the organization can get grants from local NGOs and other humanitarian organizations. These bodies can choose to finance various operations of the E-Health social enterprise based on their interests. Occasional contributions from well wishers, social media and the governments of various countries can be other ways of generating revenue for the social enterprise.
To kick start its operations, the organization can develop a good proposal to request funds from big Non Governmental Organizations. Some of the Non Governmental Organizations are Ford Foundation from the United States of America, Hidaya Foundation from Pakistan, Aga Khan Foundation from Afghanistan, and Rockefeller Foundation from the United States of America.
Marketing Approach
This involves the use of social media, public relations approaches and other marketing approaches. Social networks to be used by e-Health online social enterprise include Facebook and Twitter (James, 1984, p.56). The enterprise can might as well use other media channels such as real time television shows. Apart from the tradition public relations, the enterprise can make use of online public relations. The latter will be geared towards promoting the image and brand identity of the enterprise at the global scale.
Other marketing approaches include building business relationships through alliances with other online e-Health social enterprises so as to give the business more strength in terms of human resources capital and finance to acquire more customers as well as maintaining the existing ones (Reid, 1996, p.39).
In addition, the social enterprise can choose to publish newsletters and brochures occasionally which are accessible online and also in printed form. Moreover, help centres can be established in rural areas where people will be able to get more information about the services offered by the organization considering the fact that the level of education may be low in some of the rural areas. Application of the above means will try to make sure that the maximum possible number of people from the target areas (Namibia and Botswana) understand better the organization’s core value and missions.
Required Team and Mechanisms for Recruiting the Members
Since this will be an online business, not many people will be required. But those required should be perfect in their respective fields. The first and foremost requirement is that they have the leadership qualities imbibed in them. They should know how to convince people. They should be logical in their talks with people. Initially, the team required shall consist of a limited number of people. They shall be experts in finance, business, projects and efficient leaders.
Such people can either be sent, as a help, by governments of various nations or they can be recruited online, through social networking websites viz., Twitter, Facebook, LinkedIn, etc. Such networking sites are instrumental in providing useful information that is helpful to the employer as well as the employee. Both can benefit in the sense that the employer can read about the expected employee’s qualifications and experiences and the employee in turn can read about the employer’s business (Doyle, 2011). The skills and competencies of members to be recruited in the team shall be carefully analyzed.
The enterprise will also focus on selection and recruitment of the team members. Areas of key skills and competencies include strong analytical and communication. However, weakness can be witnessed in lack of ability to control emotion. Strong analytical and communication skills are very necessary in my team. Online channels such as career points and skill pages can be used in locating graduates with those skills. Besides, traditional channels that can be applied in the recruitment process include adverts in the local newspapers. Among these selection and recruitment processes, online chances would be the best for the enterprise (James, 1984, p.58).
An Indication of Funding Requirements and Source Options
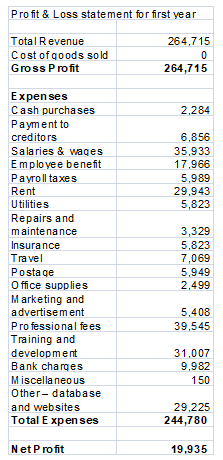
As for the funding requirements, a thorough study has to be done on the expenses to be incurred. The different account statements at the end of this report shall be helpful in understanding the details. The initial requirement of funds shall be those that pertain to purchase of furniture and equipment, building and the website. Other expenses can be taken care of from the sales revenue.
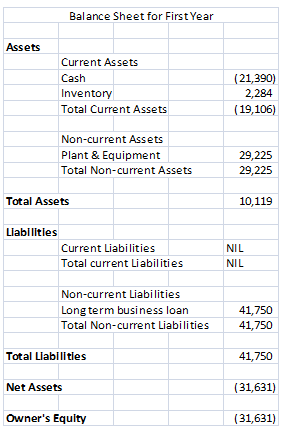
The principals are planning to invest an amount of $41,750. From the table given below, it is evident that an amount of $21,390 shall be required as loans from financial institutions and/or banks. A nominal figure of $10,020 has been taken as the initial sales figure.
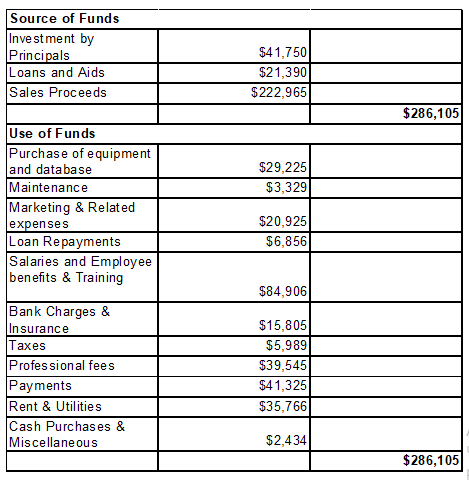
The amount is based on the case study that has been used in this report. It is understood that profits cannot be expected from the very first month. It needs great efforts. Gradually, by virtue of the efforts made by the employees, the sales figure has been shown increasing with each passing month.
The expenses also differ on a monthly basis. It is noticeable that for the first year, the cash flow is continuous in the negative. This is a feature that is not usually witnessed in cash flow statements. The simple reason is that the income is less than the expenditure. The only major source of income shown is the online sales. The loan amount is negligible. Either the income should be increased or the expenditures should be curtailed. Moreover, in the first month, the major expenditure was under the ‘Database and Website’ head. Since there was no initial capital available, the cash flow is seen in negative.
To increase the income, it is a must to increase the online customers. This can be done by promoting the cause of our social enterprise on social networking websites like Facebook, Twitter, and LinkedIn, urging people to participate more for the noble cause. Apart from this, help can be received in the form of loans from various companies engaged in finances to social enterprises.
One such company is Big Issue Invest. The company aims at providing working capital loans, among other features, to social enterprises (BigIssueInvest). It is noticed that by the year end, cash flow has improved but it’s still in the negative Second year onwards, the condition seems to be improving. The figures have been assumed to be on the moderate side.
However, some figures have been calculated as per the approximate rates. Like the ‘Employee Benefit’ has been taken to be half of the employee salary. The ‘Payroll Tax’ has been taken to be one sixth of the salary. As for the requirement of actual funds, it can be studied under a timeline, financial projections, overall funding requirements, and funding source options.
The manager of the e-Health enterprise has to write down his expectations and preferences because a deal breaker may result from the simplest idea. It is essential to ask for references from similar projects, such references should be used to provide a record of questions that the chief executive officer wants to be answered. Moreover, the conversation should not be allowed to proceed in any direction.
It is important to get information that is needed to make a decision. Additionally, the manager needs to spend time documenting the requirements so that the expectations are well conceived. For example, a six month project should not be allowed to go on for more than one year (Reid, 1996, p.57). When project managers are laying out their plans, it is usually a good idea to get information from the top management. Not necessarily talking about the small details of how the project would be managed during the engagement period (Tidd, 2010, p.48).
Excellence could also be manifested in project leadership. The project manager must be a confident leader for his team and should be an individual who maintains control all the times. Project managers who have difficulties in making key decisions throughout the project period may fail to keep the top management’s confidence high (Nijland, 2011, p. 63).
E-Health project manager who does not keep project budget on target for effective resource management should be changed. It is known that project managers; manage tasks, critical paths, budgets and several Gant charts. The ability to efficiently and effectively manage resources has a direct bearing on the project staying within the allocated budget, which is a major determining factor in the success of a project. Likewise, the e-Health social enterprise project managers should check the project status weekly for update so that people can be held accountable to the duties that they have been assigned.
A manager who focuses the budget regularly may prevent the project from delays. Focusing by managers should be based on what is known, what was known and future of the expectation. These change on a weekly basis depending on the progress details.
An effective manager often informs his team by providing them with continuous update both on forecast and actual budget financial (Lawrence & Weisz, 1998, p.37). Since Non-governmental Organizations are no-profit organizations, they are not allowed to have equity. It means that an NGO cannot offer any share in the profit in exchange of any financial assistance. The Non-profit Finance Fund arranges funds from various quarters like affluent people, companies engaged in social services and money lending companies (Ransom, 2008). The table 1 indicates the overall funding requirements.
Plan of Action between 24 to 48 Months Period
It is vital to develop an audit team that reviews the e-Health online social project after every short period during the project cycle. The audit team should be self- dependent without personal interest in the project. Auditing should be carried on project classification, collected data, advantages and disadvantages of carrying out the project, achievements and relevance of the management’s priorities (Schön, 1983, p. 23). Finally, integrative management process that meets the priority, definition, scope, mission, budget schedules, and control must be prioritized.
The manager of e-Health online social enterprise must set clear conditions for schedule, budget and tasks that must be achieved. A standard contract for the signature should be drawn to allow the contract consider all the obligations. The project needs good auditing that depends on appropriate processes, essential setting priorities, goals, schedules, project definition, supportive culture, and budgetary control for project implementation.
The lessons learned from the process should be stored so that other customers can use it. Establishing processes for terminating projects that are not feasible help in achieving objectives and goals of the e-Health online social enterprise as argued by Tidd (2010, p.54).
References
Ali, M 2010, Poorest countries of the world, poorest nations by GDP per capita. Web.
BigIssueInvest n.d., Finance for social enterprises. Web.
Carr, NG 2001, The digital enterprise: How to shape your business for a connected world, Harvard Business Press, USA.
Chandler n.d., Open source applications foundation. Web.
Field, ME 1996, Telemedicine: A Guide to Assessing Telecommunications in Health Care, National Academy Press, Washington DC.
Field, ME 1996, The Oxford Companion to Philosophy: New Edition, Oxford University Press, New York.
James, S 1984, The Content of Social Explanation, Cambridge University Press, Cambridge.
Lawrence, C & Weisz, G 1998, Greater Than the Parts: Holism in Biomedicine, Oxford University Press, New York.
Nijland, N 2011, Grounding eHealth: Towards a Holistic Framework for Sustainable eHealth Technologies, University of Twente, Enscheda.
Ransom, D 2008, Starting up: Funding your social venture. Web.
Reid, JA 1996, Telemedicine Primer: Understanding the Issues, Innovative Medical Communications, Billings, MT.
Schön, D 1983, The Reflective Practitioner: How Professionals Think in Action, Basic Books, New York.
Tidd, J 2010, Gaining Momentum: Managing the Diffusion of Innovations, Imperial College Press, London.
Vodafone 2010, E-Health Case Study: Vodafone. Web.