Psychosis, in the broadest sense, is a disorder of mental activity that leads to disturbance of the real-world perception and disorganization of behavior. In severe cases, patients’ mental and behavioral reactions may be grossly in conflict with the actual situation. Researchers note that as of 2013, there were 23.6 million prevalent cases of psychotic disorders worldwide.
Nosologies of the end of the 19th century and the beginning of the 20th century described psychosis as the destruction of personality that results in alterations in certain psychological functions. At present, scientists and psychiatrists have extensive scattered data on the types, causes, and symptoms of psychotic disorders, although there is no single theoretical description and approach to its treatment.
At the same time, there is a developed conceptual framework on psychosis that includes, in addition to the notions mentioned, the first episode of psychosis, its phases, and treatment methods. Researchers note that in general, psychosis is treatable, and psychopharmacological interventions can reduce particular symptoms. This paper defines psychosis and examines the first episode psychosis. It also analyzes different types of psychosis, its causes, and symptoms.
Rationale for the Subject and its Importance in the Field of Addiction and Healthcare
It should be emphasized that psychotic disorders are still a serious challenge to psychiatry. According to research data, one in two people with such a psychotic disorder as schizophrenia does not have appropriate treatment. Furthermore, psychosis remains one of the most prominent causes of disability, and recovery rates have not been improving in the last decades and constitute one case in seven.
Approximately $100 billion is spent worldwide annually on the treatment of psychotic disorders, and the risk of mortality from these diseases is still high. These statistics indicate a great danger of psychosis and a lack of data available to physicians in this regard. For this reason, the analysis and consideration of information on this disorder appear to be pertinent and relevant to the field of addiction and healthcare.
What is Psychosis?
It should be emphasized that the term “psychosis” is a theoretical label referring to actual psychological experiences. Depending on the disorder type, these can be hallucinations such as hearing, seeing and feeling things that are unavailable to others, strong beliefs in insane ideas, confused thinking, difficulties in concentration, unemotionality, and apathy.
These experiences are primarily associated with psychosis, although it is impossible to distinguish it from other disorders clearly. Such psychological phenomena may occur due to post-traumatic stress disorder, depression, or personality disorders. Moreover, certain psychotic experiences may have unique individual characteristics in a particular patient, as well as be hidden from other people.
It should be noted that these factors make defining psychosis rather challenging. Researchers note that about 10 percent of people have various psychotic experiences, such as hearing voices, at some point in their lives. At the same time, about one person in every hundred is diagnosed with schizophrenia. Therefore, psychiatrists need a consistent definition of psychotic disorders and criteria for their detection for therapeutic purposes.
Currently, the fifth edition of the diagnostic and statistical manual of mental disorders (DSM-5) contains a section on the schizophrenic spectrum and other psychotic disorders. Although the term “psychosis” previously had different meanings, its use in DSM-5 is now associated with the experience of disconnection from reality. Thus, the criterion of severe disturbances in the perception of the world and, consequently, cognition and behavior problems assist psychiatrists in diagnosing.
The first time a person experiences any psychotic symptoms or a psychotic episode is referred to as the first episode psychosis. This episode consists of three phases: prodrome, acute, and recovery. At the first stage, the person can notice insignificant changes in perception and unusual experiences, though they can be vague and imperceptible. The second phase is characterized by clear and explicit psychotic experiences such as hallucinations, confused thinking, and delusions.
Recovery is commonly referred to as remission and restoration of normal functioning. These experiences may appear unfamiliar, confusing, and frightening, which can cause increased anxiety and fear. Stereotypes and misconceptions regarding this disorder can only exacerbate stress. However, these experiences can be caused by a variety of factors, including physical issues and diseases, substance use, nutritional problems, and lack of sleep.
Moreover, studies indicate that early treatment can effectively deal with potential danger if the first episode is related to psychotic disorders. Many people who approached health care professionals have fully recovered and had no more psychotic episodes.
Different Types of Psychosis
It should be pointed out that various types of psychotic disorders differ in symptomatology, intensity, duration, and prognosis. Schizophrenia is the most prominent and widespread diagnosis of all psychotic disorders. It is an endogenous mental disease characterized by the disorganization of thought processes and emotional reactions. Schizophrenic disorders, in general, are distinguished by fundamental impairments of thought and perception.
The most common symptoms are auditory hallucinations, such as commenting voices, persistent delusional beliefs, paranoia and fantasy delirium, catatonic behavior, disorganized speech, and thinking with significant social dysfunction and impaired performance. The diagnosis of schizophrenia is made when the symptoms last for at least six months and have a significant impact on the patient’s ability to function.
According to DSM-5, psychotic symptoms can be considered schizophrenia if they are not caused by drugs, medications, or somatic illnesses. The schizophreniform disorder has some clinical features of schizophrenia and a relatively benign course and prognosis. As opposed to schizophrenia, it is diagnosed when the symptoms last from one to six months. Over time, it can either completely resolve or progress to a more severe psychotic disorder.
Schizoaffective disorder combines the signs of schizophrenia with an affective disorder such as bipolar disorder or depression and is characterized by abnormal thought processes and mood disorders. A diagnosis is usually made when the patient has typical psychotic symptoms accompanied by emotional instability. It should be noted that affective features may influence the characteristics of psychotic symptoms. For example, patients with depressive tendencies may have delusions of guilt and disasters.
The brief psychotic disorder is characterized by a sudden outbreak of at least one psychotic symptom or episode. The spectrum of symptoms is similar to those of other psychotic disorders, but this diagnosis is made if it lasts up to one month. This disorder may be caused by traumatic events in the patient’s life that result in increased levels of stress, such as the loss of a loved one or home. It should be noted that it can be exogenous and originate from situational and psychological reasons, although there is no fixed point of view on this issue. Recovery from this disorder usually takes a short period of approximately one month.
In contrast to schizophrenia, delusional disorder is marked by a well systematized and internally consistent dominant delusion without intense psychotic manifestations. For example, a patient may be convinced that his spouse is cheating on him or that he is being surveilled by the intelligence agency in the absence of objective evidence. At the same time, this condition is not accompanied by hallucinations, affective disorders, or thought disorders, and the patient can function normally in other areas of his life.
This diagnosis is made when delusions last a month or more. There is also such an unusual mental illness as a shared delusional disorder. In this case, two or more people with close emotional ties usually share the same delusional symptoms. According to DSM-5, shared psychotic disorder is considered a separate disease included in the section on the schizophrenic spectrum and other psychotic disorders. It is referred to as delusional symptoms in a partner of an individual with delusional disorder.
In addition, substance-induced psychotic disorder and psychotic disorder due to a medical condition are worth mentioning. In the first case, psychotic symptoms, including delusions and hallucinations, are caused by taking or withdrawing certain substances such as alcohol, amphetamines, cannabinoids, or opioids. In the second instance, they occur due to a chronic illness or other medical condition such as a traumatic brain injury or brain tumor.
Psychotic symptoms can dissolve if the causing factor is eliminated, or intensify in the opposite case. Paraphrenia is a mental disorder with similar symptoms to schizophrenia, which can be marked by a system of delusional beliefs with or without hallucinations and thought disorders. It generally progresses less severely and intensively than schizophrenia and occurs in people around 60 years of age. Paraphrenia is not identified in DSM-5 and is usually diagnosed as another psychotic disorder.
Causes
As a rule, the causes of psychotic experiences are associated with biological and neurophysiological factors. One of the main theses in this respect is the assumption of a major contribution of genetics. A person who has cases of psychotic disorder in his or her family history has an increased risk of developing this mental illness. Researchers point out that the results of adoption and twin studies indicate a statistical significance of the correlation between biological connections with people with psychotic disorders and the probability of disease development.
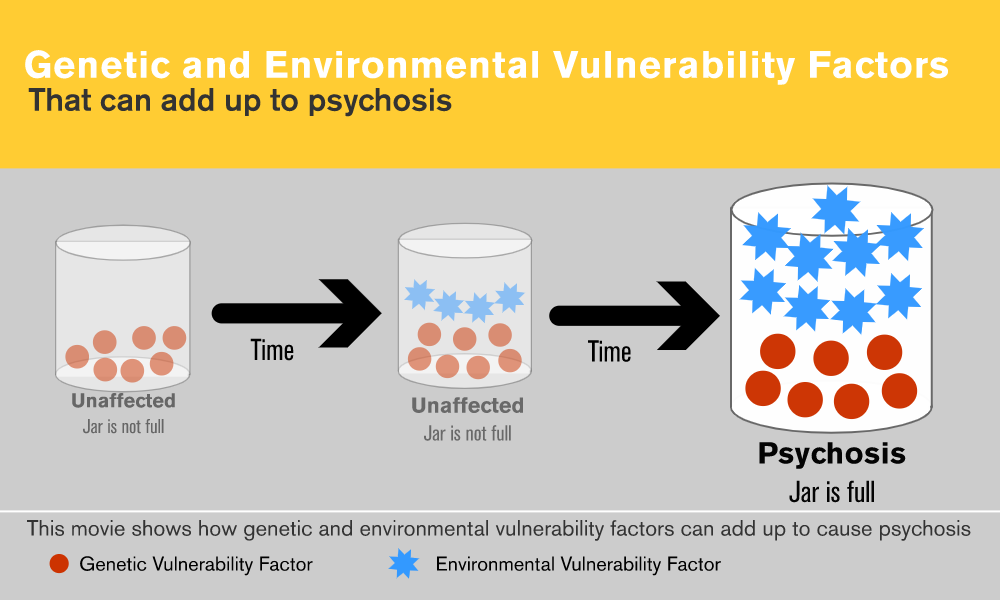
Several candidate genes have been identified as contributors to schizophrenia, but the crucial role of gene-environmental correlation is also emphasized. When environmental vulnerability factors are increasing significantly, it may affect the expression of genes associated with psychosis, as shown in Figure 1.
There are also popular hypotheses that associate the progression of psychotic disorders with neurochemical imbalances in the brain. First, neurotransmitters have a clear, statistically significant relationship with a person’s subjective experiences. Second, medications and particular substances, such as cannabis, amphetamines, and hallucinogens, that primarily affect the nervous system of the brain, can lead to the experiencing of psychotic symptoms.
Researchers primarily attribute the emergence of schizophrenia and similar diseases with disruptions in the dopamine, serotonin, and glutamate neurochemical systems.
These neurotransmitters are involved in maintaining the activity of higher psychological functions and, accordingly, are associated with cognitive disorders. At the same time, it is impossible to determine the exact cause-and-effect relationship, since alterations in patient’s neurophysiology can be both a cause and a consequence of psychotic symptoms. Thus, neurochemical theories still have limited explanatory potential and can only be defined as accompanying descriptions.
There is reliable evidence that brain impairment, for example, caused by injuries or tumors, can lead to psychotic symptoms. Moreover, differences in the characteristics of brain structures and neurosynaptic compounds correlate with the probability of psychotic disorders progression. Specific psychological and somatic diseases, such as central nervous system infections, epilepsy, cerebrovascular disease, and Huntington disease, also often supplement the clinical picture of patients with psychosis.
Thus, a range of biological reasons can cause or correlate with psychotic disorders. At the same time, there is still no single explanatory theory, and psychiatrists have to deal with numerous disparate factors. Moreover, researchers note that pathomechanisms, conditions, and causes of psychotic spectrum symptoms differ in affective disorders, on the one hand, and schizophrenia and related diseases, on the other.
It should be noted that situational and environmental conditions are also connected with the occurrence of different types of psychosis. For example, as mentioned earlier, the brief psychotic disorder is often caused by experiencing traumatic events and resolves with successful psychotherapeutic treatment. Geneticists have noted the impact of certain living conditions or experiences on gene expression.
Thus, the combination of biological, psychological, and environmental factors determines the progression of the schizophrenic spectrum and other psychotic disorders. As a rule, psychiatrists analyze the patient’s anamnesis and identify possible causes in each particular case.
Symptoms
Symptoms of psychotic disorders are usually divided into positive and negative, although some specialists also distinguish cognitive and mood ones. The disturbance of memory activity and executive functions, as well as distractibility, refer to cognitive symptoms, and depression and mania are considered to be mood symptoms.
Negative symptoms are associated with the loss or absence of normal reactions and conditions, such as the inability to maintain a focused activity or reduced intensity of the emotions experienced. This group includes a lack of motivation and affect, poverty of thought and impoverished speech, social isolation, and reduced ability to enjoy things. As a rule, they appear in the prodromal stage of the psychotic episode and precede positive symptoms.
On the contrary, positive symptoms imply excessive mental phenomena, that is, psychological reflection in the absence of a real object. Hallucinations and delusions are the most prominent and typical positive symptoms of patients with psychosis. Hallucinations refer to perceptual and sensory experiences that occur in the absence of an external stimulus.
Patients most often report hearing voices, although hallucinations can occur in any sensory modality. Visual and tactile hallucinations are usually caused by substance- and medically-induced disorders. Their intensity may vary depending on the frequency, obsession, level of distress, and impact on the patient’s behavior and social conditions.
Delusions are persistent false beliefs that are not supported by objective evidence and are clearly untrue to others. In psychiatric practice, there is a list of typical delusions, including grandiose, nihilistic, persecutory, erotomanic, and others. Delusions of control are a special form of positive symptoms when the patient believes that someone can control or know his or her feelings, thoughts, and experiences. The level of complexity of the delusional system and the patient’s conviction in its validity, as well as the impact on the patient’s behavior and life, can be used to assess the severity of delusions.
Conclusion
It may be concluded that there are still many gaps in scientific and medical data on the pathogenesis of psychotic disorders. At the same time, researchers and psychiatrists have information about the common causes, progression patterns, and symptoms of these diseases, and DSM-5 contains their up-to-date typology. The main criterion for identifying psychotic disorders and related symptoms is the patient’s experience of disconnecting from reality. These disorders are treatable, and timely medical attention can prevent severe consequences.
Reference List
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, Fifth edition. Washington: American Psychiatric Association Publishing.
Bromley, S., Choi, M. A. and Faruqui, S. (2015) First episode psychosis: An information guide. Toronto: CAMH Publications.
Carey, E. (2018) ‘Psychosis’, Healthline. Web.
Cooke, A. (2017) Understanding psychosis and schizophrenia. Leicester: British Psychological Society.
Fusar‐Poli, P., McGorry, P. D. and Kane, J. M. (2017) ‘Improving outcomes of first‐episode psychosis: an overview’, World Psychiatry, 16(3), pp. 251-265.
Gaebel, W. and Zielasek, J. (2015) ‘Focus on psychosis’, Dialogues in Clinical Neuroscience, 17(1), pp. 9-18.
Keks, N. and Blashki, G. (2006) ‘The acutely psychotic patient: Assessment and initial management’, Australian Family Physician, 35(3), pp. 90-94.
Lincoln, T. M. et al. (2015) ‘Do people with psychosis have specific difficulties regulating emotions?’, Clinical Psychology & Psychotherapy, 22(6), pp. 637-646.
Moskowitz, A., Dorahy, M. J. and Schäfer, I. (eds.) (2019) Psychosis, trauma and dissociation: Evolving perspectives on severe psychopathology. Hoboken: John Wiley & Sons.
National Alliance on Mental Illness (2016) Understanding psychosis: Resources and recovery. Web.
‘Positive and negative symptoms of psychosis: The care transitions network’ (2018). Web.
Primer, A. (2000) Early identification of psychosis. Web.
Sharon, I. (2018) ‘Shared psychotic disorder’, Medscape. Web.
Strik, W. et al. (2017) ‘Systems neuroscience of psychosis: mapping schizophrenia symptoms onto brain systems’, Neuropsychobiology, 75(3), pp. 100-116.
Substance Abuse and Mental Health Services Administration (2017) Understanding a first episode of psychosis caregiver: Get the facts. Web.
What causes psychosis? (no date). Web.
Zwicker, A., Denovan-Wright, E. M. and Uher, R. (2018) ‘Gene–environment interplay in the etiology of psychosis’, Psychological Medicine, 48(12), pp. 1925-1936.