The Fishbone Diagram
A framework representing issues in organization.
Main purpose:
- Unearth underlying factors affecting organization;
- Brainstorming these problems;
- Finding solutions;
- Decision making;
- Accurate problem examination.
The fishbone diagram is a framework that allows the root cause analysis team to develop a graphical representation of the issues affecting an organization that has been associated with near misses, errors, adverse events or reduced patient satisfaction
The purpose is usually to unearth the underlying factors that lead to system failures with a view to developing standardized solutions towards the same (Harel et al., 2016).
In utilizing a fishbone, the RCA team has a chance to brainstorm the causes of the problems and the possible alternatives or solutions.
The tool utilizes the cause-effect methodology to examine a problem but in a more accurate way where each condition that has been associated with poor outcomes is managed independently from the others (Abraham, Jones, Baker & Arpino, 2014).
How Fishbone works
- Problem placed on the fish head.
- Divided into sub-problems and sub-solutions.
- Joining sub-solutions.
- Forming the ultimate solution.
A problem, which is usually labeled at the head/mouth of the fish being divided into sub-problems from where the sub-solutions are sought out.
These sub-solutions are then joined, and they form the ultimate solution with different elements but being accomplished in a concurrent approach.
The best aspect of the fishbone tool is that the process of problem solving is not generalized.
The problem is understood in its most abstract form, and the RCA team focuses on each part of the problem as a contributing factor (Harel et al., 2016).
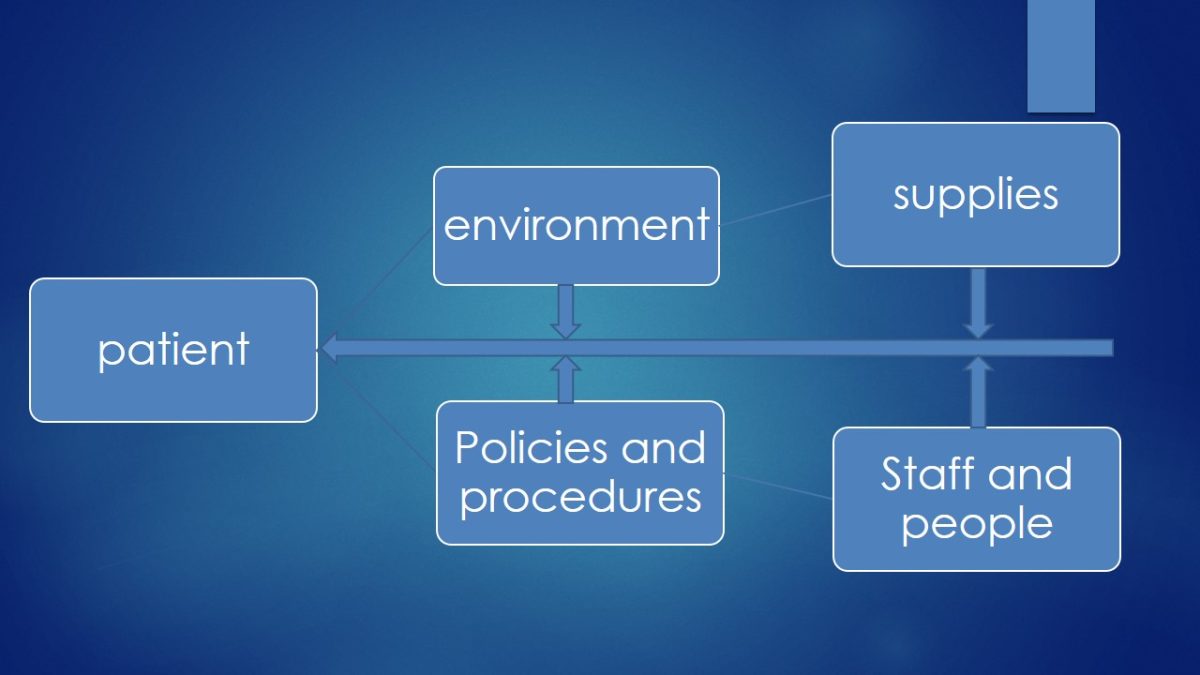
- Used in the health sector to improve services offered to patients;
- The patients at the head;
- Contains sub-problems divided into:
- Staff and People;
- Policies and procedures;
- Environment;
- supplies.
In the health care center, the Fishbone diagram works in a similar manner as the methods adopted by Kendall Regional Medical Center management in restoring patient satisfaction scores in the facility.
The problem was divided into sub-problems into four categories and solutions tailored to each class were sought. At Kendall Regional Medical Center, one of the major issues that were being reported was the low levels of patient satisfaction both on matters affecting direct care delivery and the immediate environment that did not favor the holistic healing and wellness of the patient that the facility is supposed or expected to offer.
Utilizing the Root Cause Analysis (RCA), patient satisfaction scores have significantly declined due to issues across four areas;
- Staff/people.
- Policies, and procedures.
- Environment.
- Supplies (Siddiqui, Wu, Kurbanova & Qayyum, 2014).
- Patient satisfaction with the services and the new processes was at an all-time low.
- Environmental : The new neighbor had installed a gym, and the music was causing significant disturbance to the patients.
- Supplies: Pain medication primary supplier had failed to deliver as required for a week.
- Policies and procedures: Firm tasked with cleaning the area had changed ownership without informing the management.
- Staff/People: Nurses and doctors placed more focus on customer bookings which compromised hospital discharge process.
Strategies for quality improvement
- Better health care.
- Healthy communities.
- Affordable Care.
They aim at:
- Better healthcare: Improve the overall quality, by making health care more patient-centered, reliable, accessible, and safe.
- Healthy communities: Improve the health of the population by supporting proven interventions to address behavioral, social and, environmental determinants of health in addition to delivering higher-quality care.
- Affordable Care: Reduce the cost of quality health care for individuals, families, employers, and government. (National Strategy for Quality Improvement, 2011).
Priorities include:
- Reduce harm in the delivery care.
- Engaging all partners and stakeholders.
- Effective communication and coordination.
- Effective prevention and treatment practices.
- Promote best practices to enable healthy living.
- Affordable quality health care.


Policies Needed To Support Priorities
- Payment.
- Public reporting.
- Quality improvement/technical assistance.
- Certification, accreditation and Regulation.
- Consumer incentives and benefit designs.
- Measurement of care processes and outcomes.
- Health information technology.
- Evaluation and feedback.
- Training, professional certification, and workforce and capacity development.
- Promoting innovation and rapid-cycle learning.

Quality Improvement (QI)
- By far the best strategy.
- Systematic and continuous actions causing improvement in health care.
- Principles of quality improvement include:
- QI work as systems and processes;
- Focus on patients;
- Focus on being part of the team;
- Focus on use of the data.
Quality improvement (QI) consists of systematic and continuous actions that lead to measurable improvement in health care services and the health status of targeted patient groups (HRSA,2011).
The success of this strategy always incorporates the following four key principles:
- QI work as systems and processes;
- Focus on patients;
- Focus on being part of the team;
- Focus on use of the data ( this is very important):
- Separates what is thought to be happening from what is really happening;
- Establishes a baseline;
- Reduces placement of ineffective solutions;
- Allows monitoring of procedural changes to ensure that improvements are sustained;
- Indicates whether changes lead to improvements;
- Allows comparisons of performance across sites;
- Both quantitative and qualitative methods of data collection.

Quality improvement program
Involves systematic activities;
Purposes:
- Improve health care;
- Improved efficiency of managerial and clinical processes;
- Avoid cost associated errors;
- Reactivate problem solving processes;
- Improve communication in the organization.
A QI program involves systematic activities that are organized and implemented by an organization to monitor, assess, and improve its quality of health care. The activities are cyclical so that an organization continues to seek higher levels of performance to optimize its care for the patients it serves, while striving for continuous improvement (National Quality Center, QAP, 2008).
Its purpose is:
- Improved patient health outcomes that involve both process outcomes and health outcomes (e.g., decreased morbidity and mortality).
- Improved efficiency of managerial and clinical processes. By improving processes and outcomes relevant to high-priority health needs, an organization reduces waste and costs associated with system failures and redundancy.
- Avoided costs associated with process failures, errors, and poor outcomes. Costs are incurred when nonstandard and inefficient systems increase errors and cause rework. Streamlined and reliable processes are less expensive to maintain.
- Proactive processes that recognize and solve problems before they occur ensure that systems of care are reliable and predictable
- Improved communication with resources that are internal and external to an organization, such as, funders, civic and community organizations. A commitment to quality shines a positive light on an organization, which may result in an increase of partnership and funding opportunities. When successfully implemented, a QI infrastructure often enhances communication and resolves critical issues.

Using data in quality evaluation
This is done under:
- Performance measures.
- Performance measurements.
- Performance management.
An organization may already have existing data to track improvement. It needs to monitor the data that accurately reflects how a particular system is functioning, which requires an organization to focus on specific and well-defined data sets when monitoring QI.
- Performance measures in a health care setting are derived from practice guidelines.
- Performance measurement is a process by which an organization monitors important aspects of its programs, systems, and processes.
- Performance management is a forward-looking process used to set goals and regularly check progress toward achieving those goals.

A good performance measure is always:
- Relevant.
- Measurable.
- Accurate.
- Feasible.
Good performance measures are always:
- Relevant and based on a condition that frequently occurs and/or has a great impact on the patients at their facility.
- Measurable and can be realistically and efficiently measured with the facility’s finite resources.
- Accurate and based on accepted guidelines or developed through formal group decision-making methods.
- Feasible and can realistically be improved given the capacity of the organization’s clinical services and patient population.
The Quality improvement models
- Care model.
- Lean model.
- Model for improvement.
- FADE: (FOCUS ANALYZE DEVELOP EXECUTE).
- Six sigma.
There are various modes:
- Care Model: There are six fundamental aspects of care identified in the Care Model, which creates a system that promotes high-quality disease and prevention management. It does this by supporting productive interactions between patients, who take an active part in their care, and providers, who have the necessary resources and expertise.
- Lean Model: This model defines value by what a customer (i.e., patient) wants. It maps how the value flows to the customer (i.e., patient), and ensures the competency of the process by making it cost effective and time efficient.
- Model for Improvement: This model focuses on three questions to set the aim or organizational goal, establish measures, and select changes.
- FADE: There are four broad steps to the FADE QI model:
- Focus—define process to be improved;
- Analyze—collect and analyze data;
- Develop—develop action plans for improvement;
- Execute—implement the action plans, and Evaluate—measure and monitor the system to ensure success.
- Six Sigma: Six Sigma is a measurement-based strategy for process improvement and problem reduction (Quality Improvement, 2011).
Connection to the vision and mission
Strategy aims at incorporating the organization’s principles and visions.
These principles include:
- Providing quality and affordable health care services;
- Promoting good health and reducing illness;
- Pursue medical excellence.
Values of interest include:
- Dedication;
- Excellence;
- Professionalism;
- Integrity;
- Care & Compassion;
- Teamwork.
The strategy which is quality improvement, aims at integrating the vision, mission and values of the company and the Nation.
These principles include:
- Providing quality and affordable health care services.
- Promoting good health and reducing illness.
- Pursue medical excellence.
Values of interest include:
- Dedication.
- Excellence.
- Professionalism.
- Integrity.
- Care & Compassion.
- Teamwork (Ministry Of Health, 2016).

References
Abraham, J., Jones, J., Baker, G., & Arpino, P. (2014). An analysis of hcahps scoring and the impact of the pain management dimension on hospital performance. Value in Health, 17(3), 164. Web.
Cherni, K., Ferraro, C., Green, G., Weber, C., & Kalaycio, M. (2012). Increase hcahps scores in autologous stem cell transplant patients at Cleveland clinic. Biology of Blood and Marrow Transplantation, 18(2), 392. Web.
Harel, Z., Silver, S. A., McQuillan, R. F., Weizman, A. V., Thomas, A., Chertow, G. M., … & Bell, C. M. (2016). How to diagnose solutions to a quality of care problem. Clinical Journal of the American Society of Nephrology, CJN-11481015.
Madaras, G. (2014). The effect of implementing an electronic sound masking system into a 42-bed oncology unit on “quiet at night” hospital consumer assessment of healthcare providers and systems (HCAHPS) scores. The Journal of the Acoustical Society of America, 135(4), 2402-2402. Web.
Siddiqui, Z., Wu, A., Kurbanova, N., & Qayyum, R. (2014). Comparison of hospital consumer assessment of healthcare providers and systems patient satisfaction scores for specialty hospitals and general medical hospitals: Confounding effect of survey response rate. Journal of Hospital Medicine, 9(9), 590-593. Web.
National Strategy for Quality Improvement in Health Care. (2011). National Department of Health and Human Services USA. Web.
Quality Improvement. (2011). U. S. Department of Health and Human Services Health Resources and Services Administration. Web.