Introduction
Histopathology can be defined as the microscopic assessment of biological tissues for changes or abnormalities that may have resulted from a disease in the cells and tissues. The histopathology process entails first removing a tissue sample from the patient and then processing the sample using specific histological techniques. The stained sample is then carefully placed on microscope slides before being observed using either a light or electron microscope. There are two main methods of sample preparation namely freeze and chemical fixation. The specimen is usually stained so it can easily be examined using a microscope. Histopathology is mainly employed in clinical medicine by pathologists when they study biopsys but it is also useful in other fields including forensic pathology, histology, and in histopalaeopathology.
Objective
The aim of this experiment is to examine and thereafter represent low and high power illustrations of a normal skin specimen and of skin specimens that have been affected by various forms types of skin cancer. This experiment will also present a detailed comparison of the healthy and unhealthy skin samples.
Materials and methods
The materials used in the experiment include:
- Healthy skin specimen and specimens of skin with nasal cell carcinoma, malignant melanoma, and Squamous cell carcinoma
- Haematoxyline and Eosin staining dye
- Light microscope (Magnification power of up to 400×)
- Pencil
- A4 papers
Method
The specimens were all prepared and stained using the haematoxyline and Eosine staining dye before they were examined. The first examination was done using the naked eye, the second using a ×40 magnification light microscope, and the third examination was done using the light microscope after its magnification power was set between ×100 and ×400. Each one of the observations was drawn on the A4 papers using the pencil.
Results and discussion
Normal human skin
Upon examination of the normal skin under low power magnification of the microscope, the following diagram was drawn:
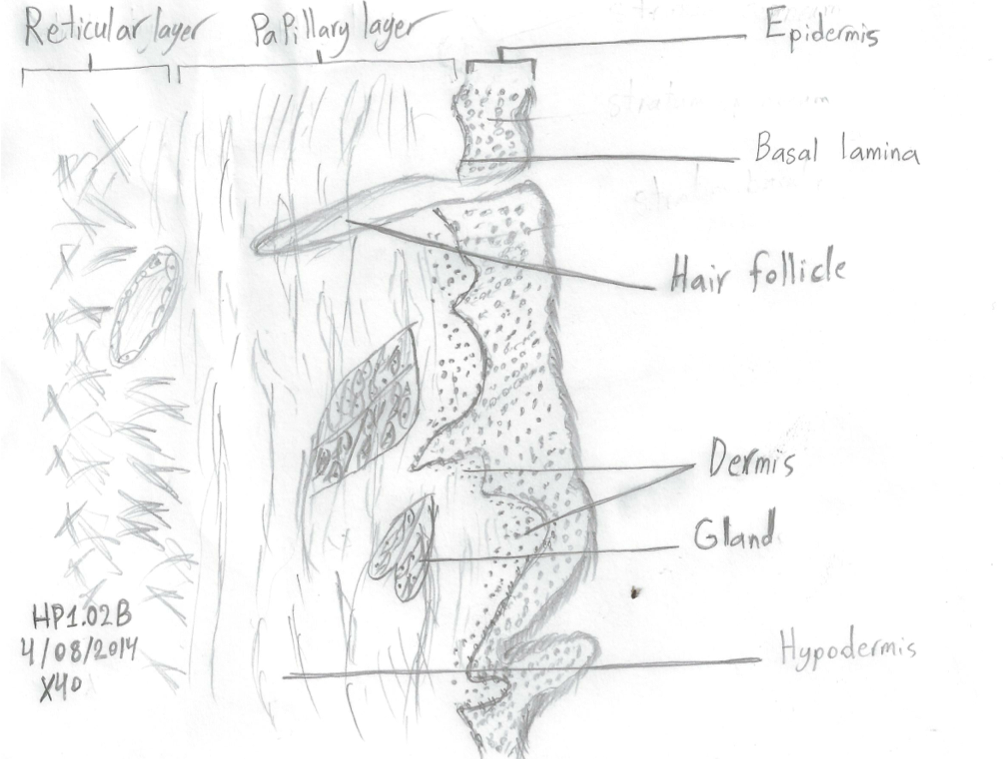
In this diagram, the outermost layer, or epidermis, is shaded darker than the other skin layers. The functions of the epidermis are numerous and these include protecting the internal organs from toxic substances, microorganisms, physical injuries. The strength and therefore effectiveness of the epidermis is directly proportional to its thickness given that thicker epidermis layers are more effective in relation to protecting an organism from foreign molecules (Harper, Oranje and Prose 2000).
Since the epidermis is avascular, it contains no blood vessels. Figure 1 also shows the basal lamina which as observed by Jenniskens et al (2000), contains proteoglycans which, due to their small size, cannot be spotted using a light microscope but can be observed with an electron microscope. The other layer that was observed and drawn in the diagram is the dermis which is not only strong and durable, but is also the skin layer that contains the blood vessels and sweat glands (Harper Oranje & Prose 2002). The main role of the dermis is to supply the epidermis skin layer with nutrients, sebum and sweat. The innermost layer illustrated in the diagram is the hypodermis which is made up of macrophages and adipose tissues.
Upon examination of a high power magnification of normal skin, the following diagram was drawn:
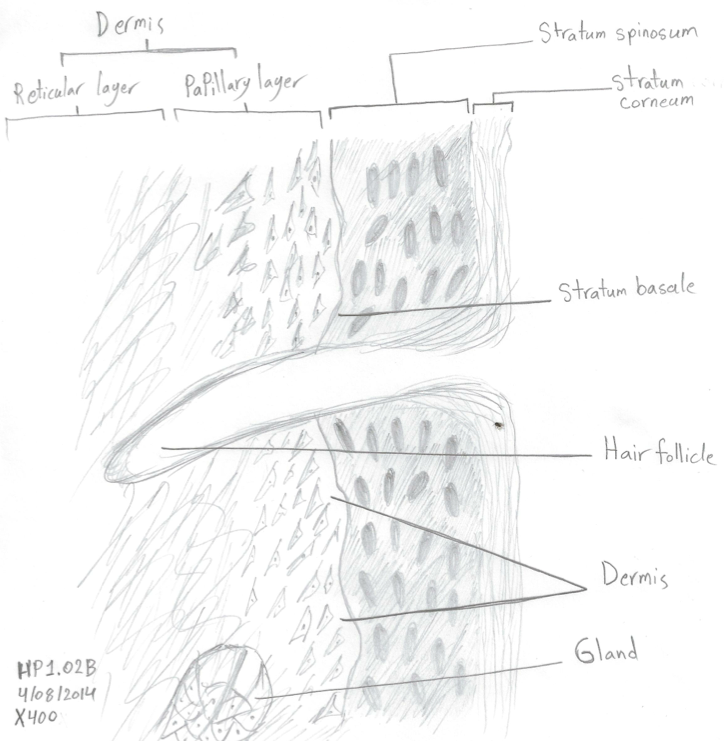
As can be observed in this drawing, the epidermis skin layer is made up of three layers layers namely the Stratum corneum, Stratus spinosum and the Stratum basale. The Stratus corneum is the outermost part of the epidermis skin layer and is made up of tightly arranged cellular membranes and a protein known as keratin. The Stratum spinosum is made up of polyhedral keratinocytes which play a vital role in fibrilar proteins synthesis while the Stratum basale consists of column-shaped cells which normally divide and thereafter push the newly formed calls to the outer layers of the epidermis.
The papillary dermis is made up of fingerlike- projections which nourish the epidermal cells while the reticular dermis is mainly composed of adipose tissue which has several functions including conserving the body’s heat, providing energy when broken down, and protecting the body from physical injury due to its mechanical shock absorbing properties (Pooler 2009).
Human skin affected by squamous cell carcinoma
Upon examination of the specimen of a human skin with squamous cell carcinoma, the following diagram was drawn:
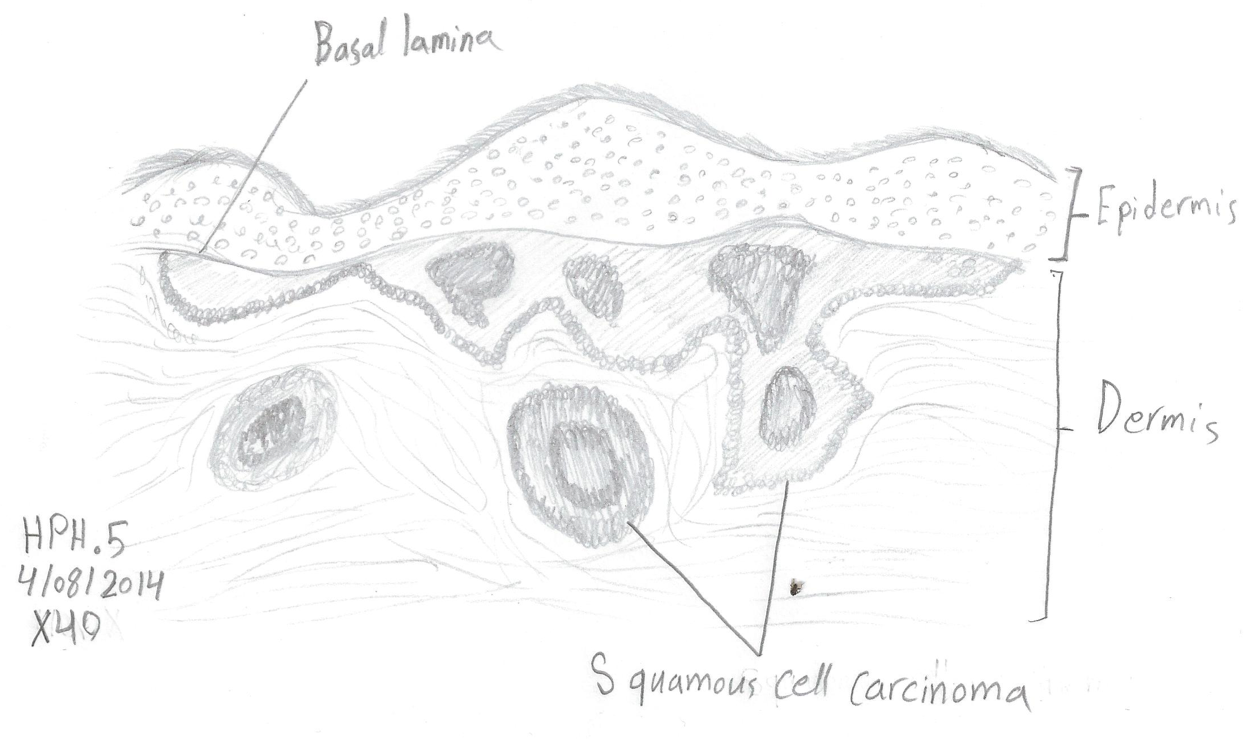
The squamous cell carcinoma represented in figure 3 occurs when there is an abnormal division of cells in the dermis skin layer. In this figure, cancerous cells are labeled as squamous cell carcinoma. These cancerous cells result in the formation of red crusty spots on the skin which easily bleed when bruised. As noted by the Department of Health and Aging (2008), this skin condition results from the excessive exposure of ultraviolet light.
This condition can occur in any part of the body but tends to mostly occur in areas that are frequently exposed to the sun. Squamous cell carcinoma can also be caused by a preexisting lesion of Bowen’s disease or actinic keratosis.
Barnes (2001) adds that patients who are already have xerodema pigmentosum or oculocutaneous albinism tend to be more susceptible to squamous cell carcinoma and this is because these genetic disorders weaken the skin’s ability to prevent damaging rays. Be that as it may, increased exposure to the sun considered the most common risk factor for squamous cell carcinoma. The condition also tends to occur more in men that it does in women, tends to mostly affect individual who are aged below 50, and also tends to occur more in individuals with green or gray eyes, light hair and fair skin.
When it is detected in its early stages, squamous cell carcinoma can very easily be cured with minimal damage to the skin but if it is left untreated, it could penetrate the inner tissues of the body and cause disfiguration. Several effective treatment methods have been developed to rid the skin of squamous cell carcinoma and these depend on the characteristics of the tumor. These methods include Moh’s micrographic surgery, electrosurgery, cryosurgery, and excision surgery, among others (Gross & Steinman 2009).
Upon examination of the human skin with squamous cell carcinoma under a high powered magnification of × 400, the following diagram was drawn:
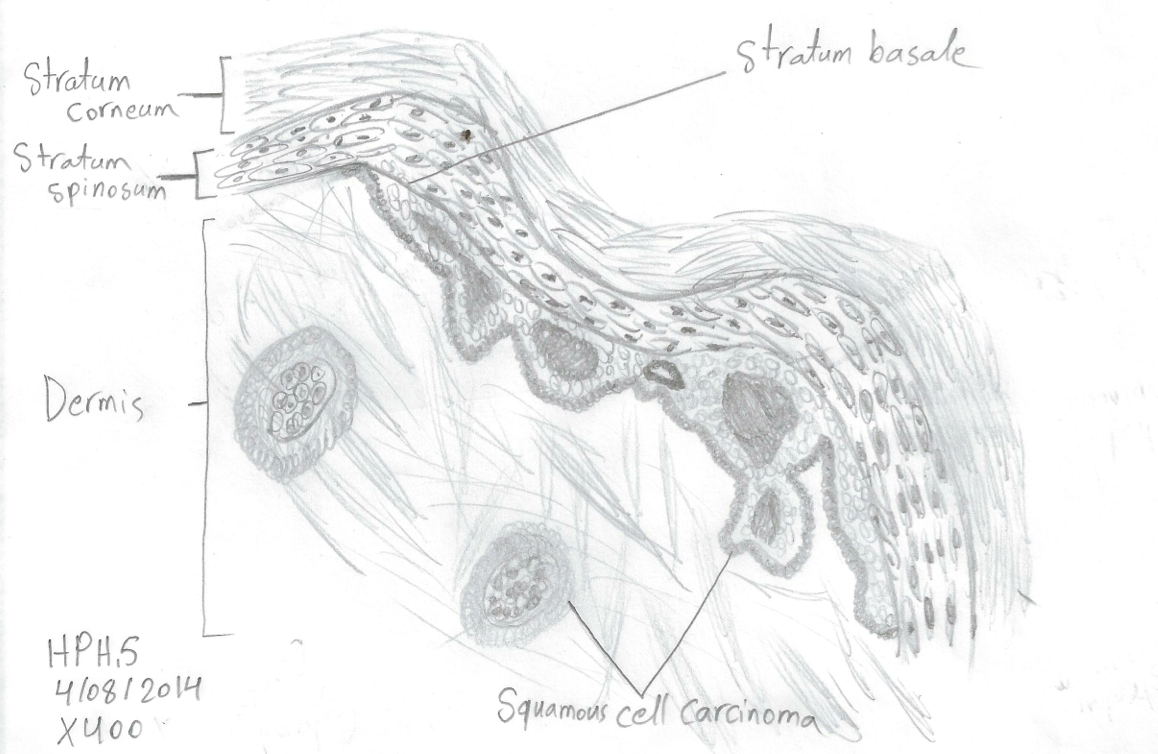
As illustrated in this magnified diagram, the squamous cell carcinoma not only occurs within the dermis but can also be seen on the boundary between the dermis and the Stratum basale.
Malignant melanoma in human skin
Upon examination of malignant melanoma in human skin using a low powered magnification microscope, the following diagram was drawn:
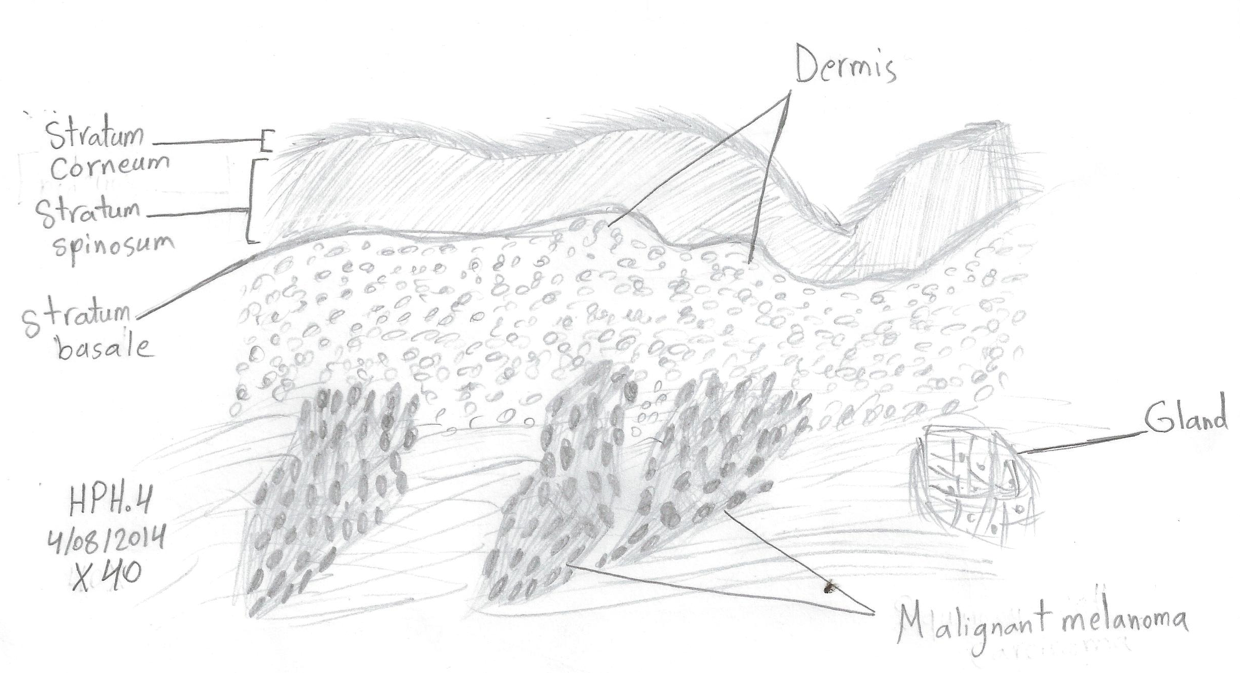
The malignant melanoma illustrated above is caused by the abnormal growth of melanocytes. When observed under the microscope, the malignant melanocytes appear as brown clusters. This abnormal skin condition develops in two stages namely the radial and the vertical. The radial development stage occurs within the dermis layer as irregular plaques but they do not result in a nodule. However, during the vertical developmental stage, the malignant melanoma lesions develop vertically and form a tumor. There are a number of risk factors for this condition and these include having a Caucasian genealogy, fair skin, light colored eyes, and light hair.
Having close relatives suffering from malignant melanoma is also a risk factor just as having a history of intense and sporadic exposure to the sun especially during childhood is. Diagnosis of malignant melanoma is almost impossible during the first seven years of its development. After seven years however, the lesions become visible to the naked eye and can easily be diagnosed. The resultant lesions usually have a diameter that ranges from 0.8-1.2 centimeters. According to Barnhill (2004) the lesions caused by the melanoma change in size and color, can become itchier, and easily bleed when bruised. Surgery is the only available treatment for malignant melanoma. The extensiveness of the surgery depends on the characteristics of the lesions.
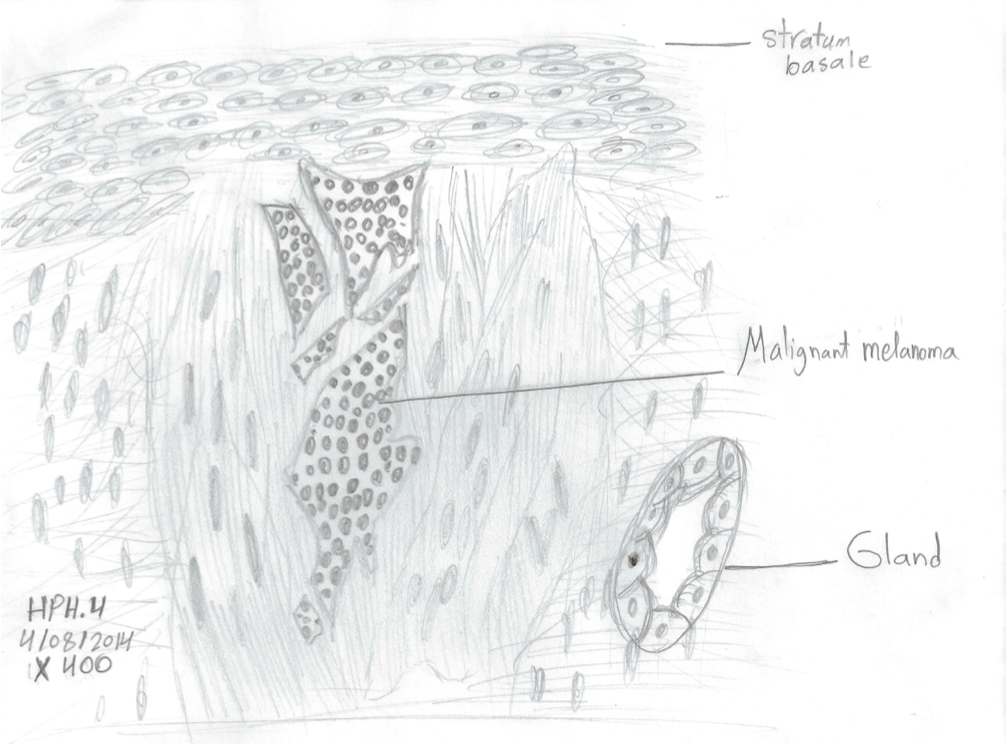
Upon examination of the melanoma under a high powered microscope, the following diagram was drawn:
Basal cell carcinoma in human skin
When basal cell carcinoma was examined under a low power microscope, the following illustration was drawn:
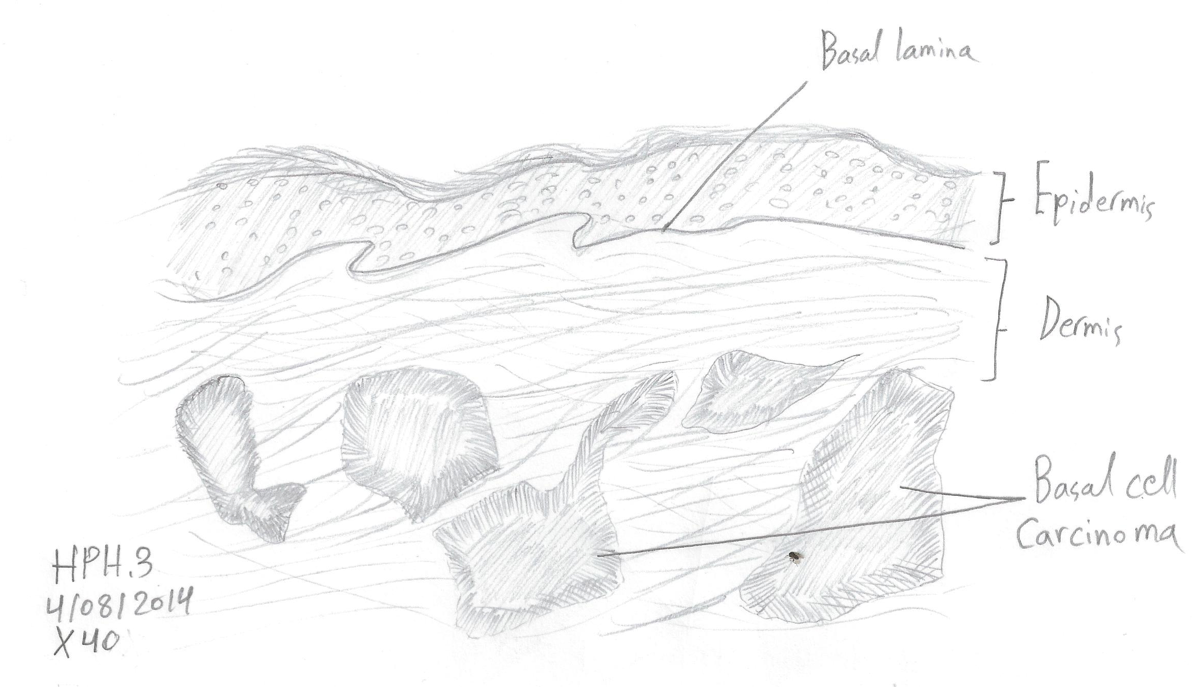
Basal carcinoma may be the most common type of skin cancer in the US but it is also the least harmful type of skin cancer. It is characterized by uncontrolled lesions that appear in the basal layer of the epidermis. The risk factors of this condition include Caucasian genealogy, and having light hair and fair skin. Bernes (2001) states that basal carcinoma develops from the pluripotenstial cell in the basal layer. The affected skin appears red, round and shiny scars which are mostly found around the neck, head and upper parts of the body. This type of skin cancer is also caused by overexposure to radiation from the sun (Department of health and aging 2009).
Moh’s surgery is the main method of treating this skin condition. Moh’s surgery is an effective method of treating both the squamous and the basal cell carcinomas because it effectively gets rid of all the cancerous cells while causing only minimal damage on the healthy cells.
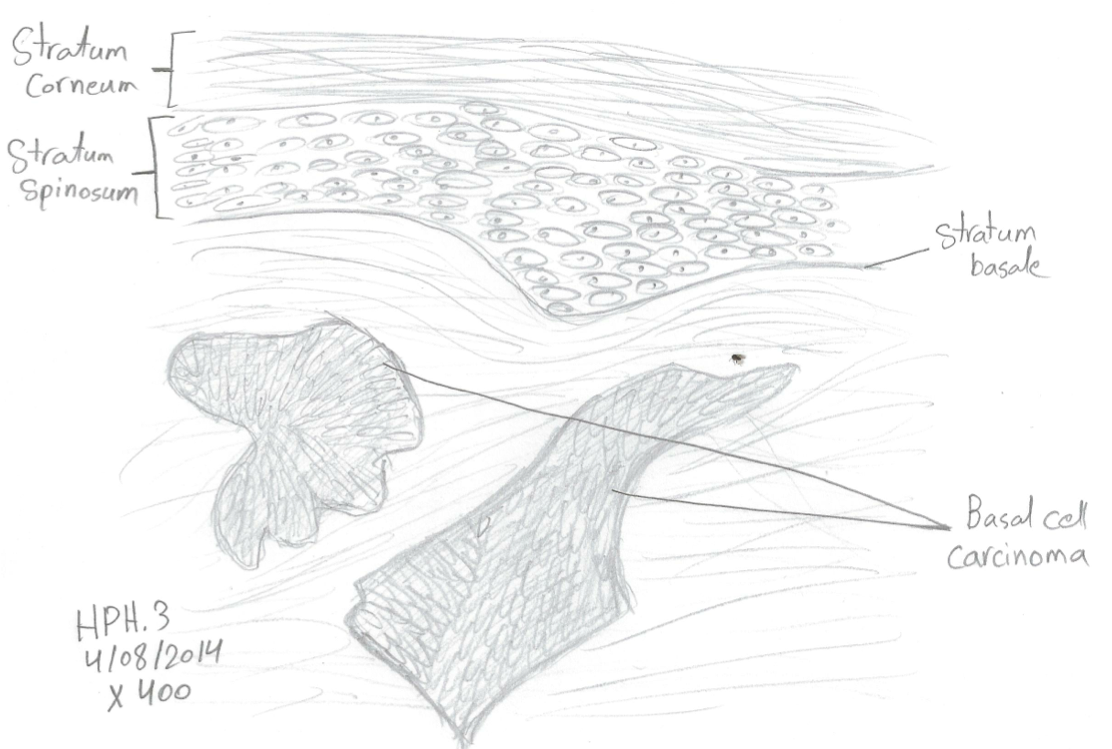
Under a high powered microscope, the specimen appeared as follows:
References
Barnes, L 2001, Surgical pathology of the head and neck, Dekker, New York.
Barnhill, R 2004, Pathology of malignant melanoma, Springer, Florida.
Department of Health and Aging, 2009, Basal cell carcinoma (BCC). Web.
Department of Health and Aging, (2008), Squamous cell carcinoma (SCC). Web.
Gross, K & Steinman, H 2009, Moh’s Surgery and Histopathology: Beyond the Fundamentals, Cambridge University Press, New York.
Harper, J Oranje, A & Prose, N 2002, Textbook of pediatric dermatology, 2 nd edn, Blackwell Publishing, Turin.
Jenniskens, G, Oosterhof, A, Brandwijk, R, Veerkamp, J. & Kuppevelt, 2000, Heparan ‘Sulfate heterogeneity in skeletal muscle basal lamina: Demonstration by phage display-derived antibodies,’ The Journal of Neuroscience, vol. 20, no 11, pp 4099-4111.
Pooler, C, 2009, Porth Pathophysiology: Concepts of Altered Health States, Lippincott Williams & Wilkins, New York.