Abstract
Sonodynamic therapy (SDT) for cancer treatment highly depends on the intake of sonosensitizing drugs present in tumor tissues and how ultrasound activates such drugs. Ultrasound is capable of piercing through the inner cells up until it touches the part with tumor in order to trigger sonosensitizer. This makes SDT to be accurate compared to additional cancer treatment methods. According to the research conducted recently by the medical fraternities, when photochemical porphyrins encounter ultrasound during SDT, they display significant antitumor effects. Therefore, for SDT to work efficiently there should be sonoluminescent light and singlet oxygen, which acts as a sensitizer.
Introduction
Cancer is a multifaceted illness influenced by the phenotype of the host meaning that it needs sophisticated and multi-factorial solutions. Several cancer treatment methods are evident in dissimilar hospitals; however, they lacked enough information on finding an appropriate tumor-inhabitation treatment method leaving the side effects1. Finally, invention of ultrasound/ Sonodynamic method is appropriate in cancer treatment because it has a penetrating tissue, which enables it to reach profound cancer infected tissues. Sonodynamic therapy (SDT) also known as ultrasound therapy is a hopeful innovative cancer treatment method that focuses on synergistic effect on tumor cell killing of a photosensitizer and ultrasound. SDT is similar to Photodynamic therapy (PDT), except that SDT is a local therapy and depends on sound for activation. Concurrently, the activation of PDT depends on light. Both SDT and PDT are important during cancer treatment because they work in a superior manner when combined. The two methods mainly strategize in treating areas infected with cancer.
It is approximately 40 years since the introduction of sonodynamic therapy. The tenacity of introducing this method was to defeat the imperfect tissues that pierce the light ability in PDT. SDT concentrates on synergistic communication among ultrasound and sensitizers. Some ultrasounds contain high frequencies that enable them to pierce deep tissues; thus, focusing in few regions where activation of sonosensitizer is possible. Various hospitals using this method with slight or no toxicity, experience positive results within a short period of application. SDT is proficient of producing remarkable results in a patient with late phase cancer. During SDT, drugs like “photofrin II, zinc, HP and chloroaluminum phthalocyanines” can perform the role of photosensitizers and sonosensitizers.
Review
While conducting SDT, ultrasound performances on biological material occur in two different ways, which involve the thermal and the non-thermal processes. During the thermal process, the captivation of ultrasound energy turns into heat. Therefore, this process largely relies on captivation and indulgence of ultrasound energy. The non-thermal process is a shear stress and cavitation, which involves pressure, force and fluid generated by the ultrasound waves running above the cellular membrane. Breakdown of cavitation bubbles can result to development of radicals.
SDT also involves acoustic cavitation, which is the more important compared to other non-thermal ultrasound mechanisms because it yields effect on biological tissues. Cavitation refers to the growth, oscillation and failure of minor gas bubbles present in a fluid medium. In ultrasound, cavitation bubbles grow by rectified diffusion process whereby the total gas diffusion into the bubbles during expansion is more than gas that gets out of the bubbles during contraction. This process has two divisions, the constant and transient cavitation. In stable cavitation, bubbles persist for a large numbers of aural cycles while in transient; cavitation enlarges faster than their original size, which makes them oscillate before disappearing. According to different researches, stable cavitation actions can lead to destruction of biological tissue. However, inertial cavitation is the accepted mechanism that can form structural changes in intact cancer cells.
Diagrams
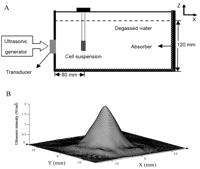
- Sonodynamic Set up
- Intensity allocation of pulsed ultrasound

“The effects of ALA solution of different concentrations on SAS cells growth after different incubation periods (n=3)”. “B: Survival rates of SAS cells after sonication alone for 1, 2, 3, 4 and 5 min (n=6)”. “C: Survival rates of SAS cells after 2 min sonication plus ALA at 0, 1, 10 and 50 μg/ml (n=6)”.
In order for sonodynamic to work well, there should be a sensitizer, energy and oxygen. Sensitizer is necessary because the cancer cells absorb it from the healthy cells. Energy is also vital during this process because it activates sensitizer resulting to oxygen reacting with activated sensitizer to create complimentary radicals in the cancer cells. The therapy occurs in the outpatient basis without any pain, injection or anesthetics. If the cancer patient is in late stage, he/she experience exhaustion, adequate pains in the tumor and nausea. This therapy lacks a long-term negative effect.
During synodynamic therapy, it is not necessary for a doctor to know the tumor that the cancer patient has and its preciseposition. The therapy is not capable of transmitting any other diseases therefore, the process can reoccur for several times. The sensitizer has little or no harmfulness before it is exposure to sound but afterward, it becomes toxic to the cancer cells only. When SDT combines with other cancer therapies in treatment, it works to perfection because of different cellular distribution.
In sonodynamic therapy, the attracted and dispatched light in the surrounding tissues limits light initiation. An alternative to this process is the application of lengthier wavelengths of light on sensitive agent. Due to SDT’s capacity to penetrate into deeper tissue unlike other therapies, it boosts PDT ability to stimulate deeply seated sensitizer plus the metastatic tumors. Ultrasound deeply pierces in the inner organs and low-intensity organs during medical diagnostics and physiotherapy thus treating deeply infected organs. Conducted research displays that disclosure to ultrasound has little synergistic consequences of 0.51W/cm2 at 1.0 MHz for a period of 10 minutes. It also shows that combination of both SDT and PDT largely contributes to the inhabitation of tumor growth compared to application of a single treatment. In addition, the total period of survival from irradiation to death between both PDT and SDT treating mice is longer (120days) than a single treatment, which is shorter (77-95 days?)
When PDT and SDT combine in cancer treatment, they work better because the two supplements each other as follows. First PDT is more effective in dealing with breast and skin cancer because it is easy for the sun to reach and activate xychloro directed by the doctor. Secondly, PDT can act as treatment to the whole body after consulting the doctor, though whole body therapy is not advisable because it has several side effects. The PDT always applies ultrasound when handling deep cancer tumors since the PDT light process is incapable of reaching those areas. The ultrasound/SDT is safe and more effective in the same manner of a process applied while viewing fetus in the womb. According to the observed changes in cancer patients, combination of therapies prompts tumor necrosis 2 to 3 times deeper than the single therapy. PDT and SDT combination becomes more successful when treating nonsuperficial or nodular tumors. Therefore, more studies in the field are important in order to exploit the cancerous cells.
In SDT process, there are different energy sources that are useful in cancer treatment. First, “light treatment bed occupied with spectrum light that illuminate the whole body”. Secondly, “laser device with a frequency and intensity applied directly over the affected areas”. Thirdly, “ultra sound instrument that generates little intensity ultrasound energy” exists.
Ultrasound exposures activate anti-tumor negotiators leading to Sonodynamic therapy. The name “Sonodynamic therapy” originated from “Photodynamic therapy” that was previously developed method in cancer treatment via light as an activation source. The first experiment on sonodynamic therapy applied photosensitizer and showed exposing the agent leads to development of synergic problems thus affecting growth inhibition in targeted tumors. The SDT effect on anti-tumor largely depends on ultrasound appliance of acoustic cavitation. Activation of SDT by ultrasound is likely to produce radicals, which are capable of inducting chain peroxidation of lipids in cellular membranes. SDT is more preferable in cancer treatment compared to PDT because it infiltrates profoundly into the body thus the deeply infected body parts may be treated. Attributable to little dispersion of light in the body tissues, PDT is only proficient of treating small tumors that occur on or beneath the skin and those on the outer layer of the inner organs.
In treating a cancer patient using SDT, firstly, the patient goes thorough assessment by the required doctor. Afterwards, the patient gets the dose basing on his/her weight and the stage of his/her tumor. The patient takes the given dose orally every morning making Ausclorin disappear from the skin and accumulate in the tumor sites. Later, the patient gets exposure to enough light depending on the present tumors. Light exposure to a cancer patient with fewer tumors varies from 30 to 60 minutes while for a patient with more tumors gets light exposure for few minutes. During the normal clinical treatment, the patient undergoes lesser bed exposure, gets enough treatment and extra three-month treatment while at home
The sonodynamic cancer treatment equally occurs through exposing the patient to a light bed with 48 panel of LED’s emanating visible and infrared light at the rate of 660nm and 940nm (+/-30nm). The patient light exposure time ranges from shorter original contact interval according to physical status and diagnosis of the patient. Then, application of ultrasound follows using hand held maniple at 1W/cm2 with frequency of 1MHz to definite sites discovered to have malignant diseases. Application of light and ultrasound process goes on for three consecutive days and the same procedure reprise using Sonnelux-1 in order to finish the required SDT treatment phase. In case of patients with numerous tumors, the management involves application of dexamethasone 2mg two times a day from the first day of treatment and continues for four consecutive sessions.
After following the essential SDT steps, there has been fruitful handling of breast and prostate cancer. Patients with dissimilar types of brain tumor for example, glioblastoma and multiforme have showed encouraging results after SDT. According to research conducted by medical practitioners, there is one case of glioblastoma multiforma complications, which showed total disappearance of tumor after conducting SDT. The same researches indicated that a fluorescent camera is capable of showing tumors that develop adjacent to the body surface. For perfect achievement of tumor selectivity, photosensitizers must combine with antibodies to fight against the tumor associated antigens. From different experiments conducted worldwide, it emerged that though sonodynamic therapy is still infancy, it is the most effective cancer treatment method. For photosensitive drug reaction within the treatment, the lesser light ultrasound is preferred. During SDT, photochemical hematoporphyrin and photofrin II that contains cell-killing tissues are activated releasing sonosensitizers that are capable of treating tumor when combined with ultrasound. Photofrin II, which is a homogeneous complex of hematoporphyrin remains in the tumor tissues for a long time compared to other body tissues thus acting as cancer photosensitizer. In addition, the exact SDT mechanisms that relates to cytotoxicity lead to cancer cells dying. However, Acoustic cavitation activates photosensitive drugs combined with malignant cell membrane leading to disruption of the cell surface.
Most photosensitizers originate from a natural forming compound s called porphorins. They are by products of recycled hemoglobin, very light intensive, accumulates in tumors, and with time, they lead to formation of cancer cells. The main photosensitizer used in cancer treatment was photofrin from hemoglobin.
In the recent experiment to test how SDT works, there was preparation of photoimmunoconjugate (PIC) among ATX-70, gallium-porphyrin photo-sensitizer and F11-39, which is a very high affinity monoclonal antibody against carcinoembryonic antigen. The conjugate resulted to F39/ATX-70 and maintained immunoreactivity besides purified CEA and this makes the cell to appear as formed by enzyme-connected immunosorbent. When vitro is united with ultrasound irradiation, the cells expressing human gastric turned out expressing G39/ATX-70 against CEA, which is more greater than ATX-70. In vivo, there was enormous growth witnessed in tumor. After one hour of administering PAD-S31, ultrasound energy conveyed transdermally to sonodynamic therapy. After a month, the experiment results indicated that intimal and medial cross-sectional region was slighter in sonodynamic therapy. This experiment concluded that sonodynamic therapy is likely to be a possible treatment method for noninvasively impeding neointimal hyperplasia.
For one to confirm that SDT is operative in killing the cancerous cells, he/she should use “dark field microscopy, sonography and fluoroscopy”. The administration of these three procedures to a patient comes before, in and after treatment. On conducting these procedures, the practitioner will tell whether xychloro is effective to the metastases. Observation of tumor obliteration process goes on during therapy while the surface tumors are visible by photodynamic diagnosis. At the start of SDT, a patient can have various tumors through fluoroscopy but as the therapy continues, the tumors disappear. SDT is capable of detecting cancerous cells years before the appearance of mammogram.
For SDT to successfully work the patient should be in good health and the cancer cells should not have seriously interfered with the delicate body structures and tissues. Therefore, it is not advisable for a cancer patient to wait for a long period before seeking SDT. This therapy is highly recognized for its gentler tumor homicide effects and works efficiently with low level of cancer present in the body. The process can also be successful in the present of many small tumors rather than few large tumors. SDT works poorly with big and thick tumors since blood cannot efficiently flow through the tumors making it hard to detect sensitizers that reside within the profound cancerous cells. In case of larger tumors, SDT is not advisable instead, debulked surgery is important. When a patient has more cancer tumors, SDT is preferable because it treats cancer on the body surface and it perfectly observes the improvement of therapy through microscopy, sonography and fluoroscopy. The most treated cancers by SDT are the breast, prostate and skin cancer and it is due to microscopy, sonography and fluoroscopy managing monitors them.
Sometimes, SDT fails to work because some patients have a mindset that only conventional therapies work successfully in cancers. Secondly, the treatment fails due to poor health conditions of a patient besides their cancer complications. Thirdly, it can be due to the patient deserting the therapy in advance. Fourthly, the treatment can fail because of a cancer patient starting SDT treatment too late after many body organs are infected. Finally, the treatment can fail if the cancer patient has medical problems that discourage application of SDT method. People conclude that there is no cancer cure, but SDT ensures that a cancer patient ends up without cancer symptoms Application of SDT in cancer treatment has more advantages compared to cancer surgeries and radiotherapies because SDT is not invasive, doctors accurately target it, and administration of the doses can be repeatedly without limitations that exist in radiotherapy. After undergoing through SDT, the healing procedure does not have scars as it is in radiotherapy. Finally, SDT is always on an outpatient or day casing setting without any long-term side effects.
Apart from treating cancer, Sonodynamic therapy also treats leukemia. The Sonodynamic irradiation is more powerful and it focuses on body tissues affected by cancer posing less effect to the normal body tissues. SDT waves lead to chemical actions if cavitation occurs, for example, water irradiation can lead to formation of hydrogen peroxide. Researches show that exposure of some drugs to SDT wave’s leads to formation of active oxygen that effectively terminate cancer tissues. The SDT waves lacks anti-tumor activity and are little in toxicity unveiling the anti-tumor activity in the body by chemical reaction from ultrasonic irradiation. Therefore, in SDT less risk is involved in causing body organs disorder. During the SDT, the chemical reaction induced in the process of violet micro bubble collapse is very important because it alters different compounds killing the cells. Recently conducted research y medical fraternities on leukemia cell showed that, the cell died on exposure to low intensity of ultrasound in the existence of porfimer sodium several pre-clinical researches have indicated that local SDT treatment of cancerous tumor promotes the immune response of a system and it acts as a warning sign to enhance the response of anti-tumor immune. SDT generates photo-oxidative cytotoxic lesions, which leads to quick death of cancerous cells thus alerting the immune system. Administering local SDT treatment can lead to dissimilar side effects such as systematic neutrophilia, initiation of acute phase proteins, high circulation level of protein and inflammatory cytokines.
The availability of tumor sensitive lymphocytes in tumor mass and lymph node creates favorable condition for the cancer. With this knowledge, it will be better to encourage modification of immune-tumor microenvironment to reduce cancer development. Conventional treatment eradicates tumor cells, which releases tumor antigen host that primes the antitumor immune reaction. However, radiotherapy and chemotherapy have an antagonizing effect on the human immune system via lymphocyte division and death. In addition, the tumor cell apoptosis that occurs due to treatment is immunogenic.
SDT also involves anti-angiogenesis therapy, which is an approach of treating different body cancers because it is crucial for tumor growth. However, the ultrasound energy used in anti-angiogenesis therapy improves the anti-tumor consequence of a chemotherapeutic cause in vivo and vitro. Among the famous uterine malignances, uterine sarcoma is the widely malignant neoplasm having a weak reaction to both chemotherapy and radiotherapy.
Though SDT is recommendable in cancer treatment, it also has synergistic effects. First, the therapy involves production of sensitizer-derived free radicals that affect chain constitution of the membrane lipids. Secondly, SDT has sonosensitizer that leads to physical weakening of human body cell membrane making the cell weak. This leads to its inability to clip forces and ultrasounds involved in transporting drugs through the cell membrane. These mediated effects caused by SDT needs more research for better understanding because doctors assume that they might be from ultrasound secreting sonochemical reaction together with sensitizer. Alternatively, they assume that it might be attributable to indirect sonoluminescence that produces light due to the tissue exposure on excess light.
Conducting sonodynamic therapy has various limitations that deter its applications in many hospitals. Firstly, the therapy is not widely used in western countries because they prefer chemotherapy, hormone therapy and radiation therapy to SDT; furthermore, the western medical fraternities are slow in adopting new therapies. Secondly, the early sensitizers in SDT had negative effects, which discouraged medical fraternities from applying the method. Thirdly, SDT did not produce enough radicals; therefore, the total rate of cell killing was low. Finally, activations of some SDT sensitizers are by blue light; therefore, in the absence of transparent body, it becomes impossible to conduct treatment.
There are noticeable developments in sonodynamic therapy since in the past two years new clinics have started applying the method in treating cancer patients. The combination of SDT and other cancer therapy methods have shown efficacy in different types of cancer such as breast cancer, liver cancer, small cell lung cancer and ovarian cancer among others.
Conclusion
In conclusion, SDT is a treatment method where the activated chemicals of sound energy form a cataract of endogenous cyto-toxic agents. SDT works in similar manner as PDT except that it avoids light from probing the inner tissue of tumors. SDT has more advantages compared to PDT since it can penetrate deep into the sensitizer composites; therefore, destroying the deeply formed cancerous tumors. However, the PDT can overcome its limitations when the composites go through activation from inner piercing sono-energy. Because SDT is a non-invasive and sound accepted treatment, the sector needs additional studies to solve the rising cancer cases. Further studies in the sector will enhance the capability of the treatment process; thus, controlling incidences of tumor progression through inducement of inflammatory necrosis in deeper tumors that are inflammatory. Finally, more studies in sonodynamic therapy are vital because SDT will be a treasured tool in targeting the inflammatory tumors.
Bibliography
American Chemical Society, Chemical abstracts, volume 139, American Chemical Society, Washington DC, 2003
Braham, M, Complementary, Natural & Alternative bladder cancer treatment-it is your life live it, Cancer Group Institute, Rochester, 2009
Castro, D, & P Capote, Analytical application of ultrasound, Amsterdam, Elsevier, 2007
Cho, W, Materia Medica for Various Cancers, Springer, New York, 2011
Gustafsson, W, New Gene Therapy and Cancer Research, Nova Publishers, New York, 2008
Haar, G, & C Coussios, Sixth International Symposium on Therapeutic Ultrasound, American Institute of Physics, New York, 2007
Hamblin, M, & P Mroz, Advances in photodynamic therapy: basic, translational and clinical, Artech House, Belmont, 2008
Hill, C, J Bamber & G Haar, Physical principles of medical ultrasonic, John Wiley and Sons, Hoboken, 2004
Lemoigne, Y, A Caner & G Rahal, Physics for Medical Imaging Application, Springer, New York, 2007
Luo, Q, Advances in biomedical photonics and imaging: proceedings of the sixth international conference on photonics and imaging in biology and Medicine, World Scientific, Singapore, 2008
Maalouf, J, Mechanism of the sonodynamic effect. Chicago, University of Chicago, 2008
Optical Society of America, Optics letters, volume 28, University of Chicago, Chicago, 2009
Osawa, E, Perspective of fullerene nanotechnology, Springer, New York, 2002
Patrice, T, Photodynamic therapy, London, Royal Society of Chemistry, 2003
Quaia, E, & T Bartolotta, Contrast media in ultrasonography: basic principles and clinical applications, Springer, New York, 2005
Shen, X, & R Wijk, Biophotonics: optical science and engineering for the 21st century, Springer, New York, 2005
Sykes, A, Advances in Inorganic Chemistry, Academic Press, New York, 2009
Song, W, Apoptosis of SAS Cells Induced by Sonodynamic Therapy Using 5-Aminolevulinic Acid Sonosensitizer, anticancer Research, January vol. 31, no. 1, 2011, pp 39-42
Torres, L, Cancer drug resistance research perspective, Nova Publishers, New York, 2007
Vaezy, S, & V Zderic, Image-guided therapy systems, Artech House, Belmont, 2009
Wu, J, &W Nyberg, Emerging therapeutic ultrasound, World Scientific, Singapore, 2006