Introduction
This presentation explores the following issues:
- eMedicine;
- Telehealth;
- Available telehealth models;
- Available technologies in telehealth;
- How to improve data tracking through telehealth.
In this short presentation, I explain the benefits of telehealth by defining the concept and its value addition advantages. I also emphasize how it improves medical outcomes, and explain the best way to adopt it. The purpose of this presentation is to encourage the use of the technological platform in the medical field. However, before we delve deeper into this subject, it is important to understand how telehealth falls within a wider umbrella of emedicine.
What is emedicine
- eMedicine is the cost-effective and secure use of information to improve the quality of health care service delivery to patients;
- eMedicine also refers to the use of technology to provide health care services;
- eMedicine involves sharing medical information among different health practitioners to improve the delivery of care;
- eMedicine is applicable in different fields of medicine, including health surveillance, health education, health research and health literature (Fernandez-Marcelo, 2015).
The correct definition of eMedicine rests in understanding how health practitioners could use computers to support information processing functions to improve health outcomes. Researchers have described how it is important in improving decision-making and records keeping functions. However, its level of adoption is dependent on the quest by health practitioners, especially doctors, to use it in their daily functions.
- It is a new way of doing things.
As highlighted in the above diagram, eMedicine simply refers to a new way of doing things in health care service delivery.
Functional Areas of emedicine
- Telemedicine/telehealth;
- mHealth (mobile technologies);
- Electronic Medical/Health Records;
- eSurveillance and Tracking;
- eLearning for Health (Olasina & Popoola, 2014).
There are different applications of eMedicine. They include mHealth, electronic medical records, eSurveillance, eLearning, and telemedicine. In this presentation, I focus on telemedicine as a key functional area of eMedicine.
What is Telehealth?
Telehealth involves the use of technology to bridge the distance in communication when delivering health services.
It facilitates the practice of medicine when patients and health care service providers are not in the same location.
Available technologies include:
- Live video;
- Remote-patient monitoring;
- Mobile Health;
- Store-and-forward.
Telehealth is not a specific service; instead, it includes a variety of technologies for delivering medical and health services. Its purpose is to enhance the delivery of health care and education because using the technological innovations associated with telehealth helps health practitioners to provide care in different areas of medicine, including dentistry, counseling, physical and occupational therapy, home health, and disaster management (among others).
What benefits have health care facilities enjoyed from Tele-health?
- Improved decision-making skills, which manifest through improved health care quality;
- Facilitates early and accurate diagnoses;
- Improves the efficiency and coordination in administrative functions;
- Reduces medical costs through reduced transfer rates and timely treatment;
- Saves lives through remote consultations (SETRC, 2015).
Organizations that adopt telehealth enjoy enhanced organizational outputs because they thrive on the backdrop of improved decision-making skills, improved organizational efficiency and an enhanced coordination of administrative functions. However, these benefits are not only limited to health facilities because patients could equally realize improved health outcomes through early diagnoses, accurate diagnoses, and reduced medical costs. All these benefits help to save lives.
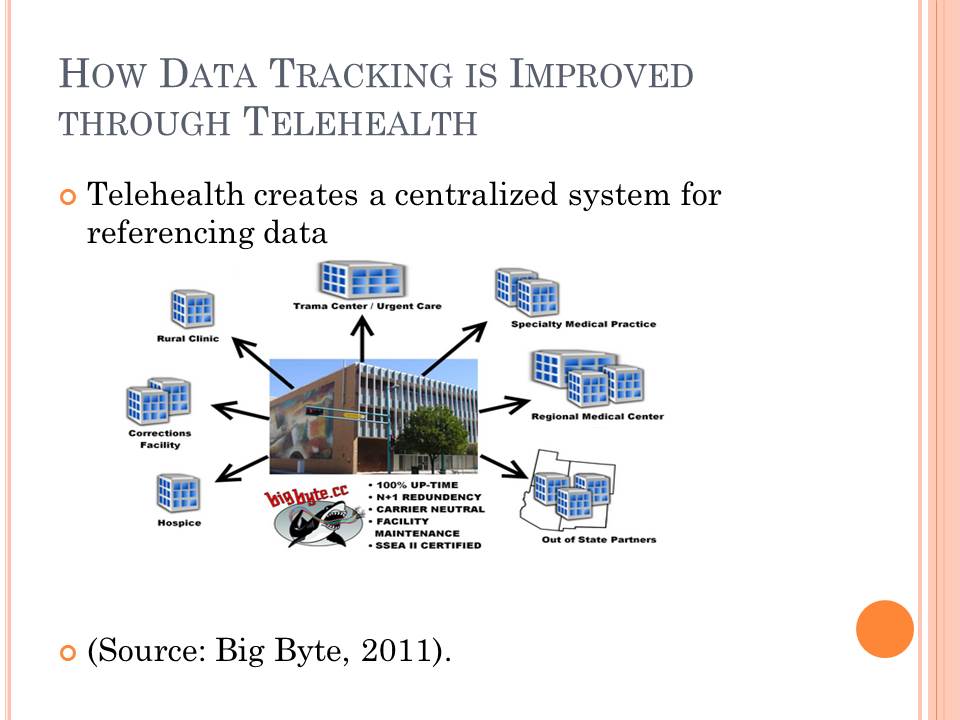
How Data Tracking is Improved through Telehealth
- Telehealth creates a centralized system for referencing data.
Data tracking is arguably one of the most important functions of health care service delivery. Telehealth helps to improve this function through increased coordination among different health centers, as outlined in the diagram. The diagram shows that the telehealth center acts as a hub for tracking data from different centers, such as the trauma center, regional medical center, hospice, out-of-state partners, rural clinics, and correctional facilities. This way, health practitioners can provide holistic care to their patients.
What types of Telehealth Models are there?
- Real-time (synchronous);
- Store-and-forward models (asynchronous);
- Centralized model;
- Decentralized model (Joseph, 2008).
According to the factor of time model, telemedicine has two main types of models – real time model and the store-and-forward model. Synchronous telemedicine is diverse, as it can be as simple as a telephone call, or as complex as robotic surgeries. In other words, the model requires both parties to be physically present, at the same time, and communicate through one platform. The store-and-forward model involves sending medical information (as pictures, biosignals and the likes) for medical assessment. It differs from the real-time model because it does not require the physical presence of both parties. A centralized model involves the interconnectedness of different regional telemedicine centers to a secondary health care service provider. Here, the regional centers cannot communicate with each other. Comparatively, in a decentralized model, the regional telemedicine centers could communicate among themselves. These models outline the functioning of different telehealth models.
Recommendations to move to Telehealth
- Understand federal and state laws governing the use of telehealth;
- Identify a service model that addresses your health problem;
- Make telehealth as inclusive as possible;
- Encourage demand-led solutions;
- Telehealth equipment needs to reflect modern technology;
- A change of attitude is needed (Rheuban, 2016).
There are different challenges associated with the adoption of telehealth. To overcome them, health administrators should understand the legal ramifications of adopting telehealth and encourage demand-led solutions in its adoption. To achieve the best results, they also need to identify a service model that addresses their unique health problems and promote inclusivity to create a positive attitude for its adoption in the organization.
Conclusion
- Telehealth improves health outcomes;
- Telehealth reduces health care costs;
- Provides more educational opportunities for health care service providers;
- Improves efficiency in the provision of health care services;
- Improves data management services.
Generally, health administrators should adopt telehealth because it improves health outcomes. However, its advantages cut across the board, in the sense that health care practitioners, patients, and family members would benefit from its adoption.
References
Big Byte. (2011). Telehealth and Colocation. Web.
Fernandez-Marcelo, P. (2015). Telehealth and emedicine. Web.
Joseph, T. (2008). Healthcare Information Systems and Informatics: Research and Practices. New York, NY: IGI Global.
Olasina G., & Popoola, T. (2014). Predictors of the Use of E- Medicine by Medical Doctors. J Health Med Informat, 5(4), 166-172.
Rheuban, K. (2016). Adopting telemedicine in practice. Web.
SETRC. (2015). Benefits of Telehealth. Web.