Introduction
Tuberculosis is an extremely widespread infectious disease that has caused pain, suffering, and deaths to thousands of people around the world. The health sector has already accorded Tuberculosis a high priority status because it remains a major public health concern. The strain of bacteria that causes tuberculosis is known as Mycobacterium tuberculosis.
Although the bacteria mainly attack the lungs, nonetheless, it can also attack other body parts including the spine, brain, and kidney. Over the years, the bacteria strain that causes tuberculosis (Mycobacterium tuberculosis) has developed a lot of resistance mainly as a result of a lack of compliance to treatment on the part of the patient.
This is because the treatment regiment usually lasts for a very long time and some patients find it hard to cope (World Health Organization 2009). Also, poorly managed treatment programs are also to blame for the increased prevalence of the disease. This resistance presents a new challenge to public health care.
The mode of transmission of tuberculosis is via the air, when an individual with TB of the throat or lungs sneezes, talks, or coughs. It is always advisable for people who have been exposed to persons suffering from TB to see their doctor for tests. Individuals with a weak immune system are at a greater risk of contracting TB.
The facts
For persons suffering from TB of the lungs, general symptoms include persistent coughing, often lasting for more than three weeks, coughing up mucus or blood, weight loss, fatigue or weakness, chills and fever, and night sweats. Without proper treatment, TB may be fatal.
According to the World Health Organization report, about a third of the global population could be infected with the bacterial strain that causes tuberculosis- Mycobacterium tuberculosis (World Health Organization, 2009). Also, the World Health Organization Report also notes that approximately one new infection of tuberculosis happens every second (World Health Organization, 2010).
The proportion of individuals that get sick every year as a result of tuberculosis appears to be falling or stabilizing globally, but since the population is increasing steadily, new cases of tuberculosis appear to be on the increase (Who Health Organization, 2010). In 2007, the World Health Organization reported an estimated 13.7 active cases of chronic tuberculosis globally (World Health Organization, 2009).
At the same time, some 1.8 million deaths as a result of tuberculosis complications were reported worldwide, and many of them were in the developing countries (World Health Organization, 2009). Furthermore, a higher number of individuals in the developed countries contract tuberculosis since their immune systems tend to be already compromised as a result of higher exposure to the AIDS virus or immunosuppressive substance abuse.
Tuberculosis lacks a uniform distribution across the world, with nearly 80 percent of the cases being reported in African and Asian countries. TB infection involves the interplay between the host, the environment, and the agent, according to the diagram below.
(Source: Horwitch, 2004)
All those people who are exposed to the disease do not get infected. Also, all infected individuals may not get active diseases. Mycobacterium tuberculosis, the bacteria strain that causes tuberculosis, is a small non-motile, aerobic bacillus.
Majority of the unique clinical characteristics associated with this particular strain of bacteria are due to its high lipid content (Jasmer, Nahid & Hopewell, 2002, p. 1861). Besides the Mycobacterium tuberculosis is a complex strain made up of four other strains that can also cause TB. They include M. africanum, M. bovis, M. microti, and M. Zanetti.
M. africanum strain is not as widespread as the other three, but it still accounts for a large proportion of the tuberculosis cases reported in Africa (Madison, 2001). Before the introduction of pasteurized milk, M. bovis used to be a common cause of tuberculosis, but this is no longer the case. M. Zanetti is also rare, but a few cases have been reported in Africa.
On the other hand, M. microti is mainly seen in immunodeficient individuals, but there is the likelihood that scientists and researchers may have underestimated its prevalence (Niemann et al., 2000). If untreated or undiagnosed, TB may be potentially devastating, and could even cause death.
For many years, tuberculosis has remained a major killer in many of the less developing nations. Because tuberculosis spreads through blood, other vital parts of the human body are at risk including the brain, lymphatic system, intestines, circulatory system, joints, skin, and bones.
Infants below the age of 1 year are at a greater risk of tuberculosis meningitis since their immunity is still weak and as such, they cannot fight the bacterial strain that causes this disease. Tuberculosis also poses a danger to pregnant women is infected. It is important therefore to treat them on an immediate and emergency basis to avoid the transmission of the diseases to the unborn child as well.
Impact on the world
Individuals from developing countries are the main victims of tuberculosis. TB has even been labeled as a disease of poverty because it affects marginalized populations and poor countries. Ninety-eight percent of the deaths related to TB is thought to emanate from developing countries, while 95 percent of all the reported cases of TB are also from the developing countries (World Health Organization, 2010).
Also, most of the deaths occur in Asia and sub-Saharan Africa. TB is a leading cause of death among young women and children across the globe. Individuals living with HIV/AIDS are at a greater risk of contracting TB more than any other individuals (World Health Organization, 2001). Also, the HIV/AIDS pandemic is also responsible for the majority of the new cases of TB reported globally.
The indirect and direct costs associated with TB are not only devastating to individuals but also the families as well. Globally, related deaths and illnesses lead to the loss of millions of productive and potentially healthy years of life across the globe, even as people have access to affordable, cost-effective, and available cure. A lot of factors add to an individual’s vulnerability to TB.
Being of a minority group, poor, a child, a refugee or migrant, a prisoner, having a weak immune system as a result of substance abuse or HIV, can all predispose one to contract TB (Dhuria, Sharma & Ingle, 2008). TB has for long been associated with being poor. As such, crowding, malnutrition, poor sanitation, and poor air circulation are all linked to poverty and by extension, to TB.
TB is characterized by an acute socioeconomic burden because its greatest impact is on adults when they are most productive economically. Consequently, this reduces the productivity of the global workforce.
Impact in the UAE
The incidence of TB for every 100 000 people in the UAE seems to be on the decline. In 2004 for example, 17 people in every 100 000 individuals were reported to have contracted TB. By 2008, the figure had declined 6 (The World Bank, 2011).
However, experts are warning that despite the stable state of TB infections in the UAE, there is a high potential for the disease to spread (National Tuberculosis Control Program, 2010). This is due to a steady migration of people from high prone TB areas such as China, India, and sub-Saharan Africa into the UAE (Khalaf, 2009).
A lot of attention should be given to the health care workers because they are the most vulnerable group to contract TB. Although the UAE still has the lowest rate of spread of TB in the Gulf Region, nonetheless, there is also another fear in the form of latent TB patients who have still not been diagnosed with the disease.
Comparison with the UK
For the past 20 years, the UK has witnessed a gradual increase in the number of reported cases of tuberculosis. In 2009, the number of reported cases increased by 4.2 % compared with the reported cases in 2008. As a result, the overall number of tuberculosis cases for every 100,000 members of the population rose to 15.
In 2009, the UK reported some 9,040 cases of tuberculosis. A lot of these reported cases were in urban areas. Thirty-eight percent of all the reported cases of tuberculosis in the UK’s urban areas are in London. This represents 44.4 cases of tuberculosis for every 100,000 individuals.
Most of the migrant to the UK are from sub-Saharan Africa and the Indian subcontinents where tuberculosis has high prevalence rates. This may perhaps explain the apparent increase in the rates of tuberculosis.
Fig 2: A figure of the reported cases of tuberculosis per 100,000 in the UK between 2000 and 2009 (Source: Anderson et al., 2010).
On the other hand, the UAE has lower rates of tuberculosis infection (see table 1 below) compared with the UK. Although the number of immigrants from sub-Saharan Africa and Asian where tuberculosis is a real menace also migrate to the UAE, nonetheless, the AUE appears to have instituted better control mechanisms to curb the spread of tuberculosis, compared to the UK.
On the other hand, it could be argued that the UK has also documented the patent cases of tuberculosis and the UAE has not and hence the difference.
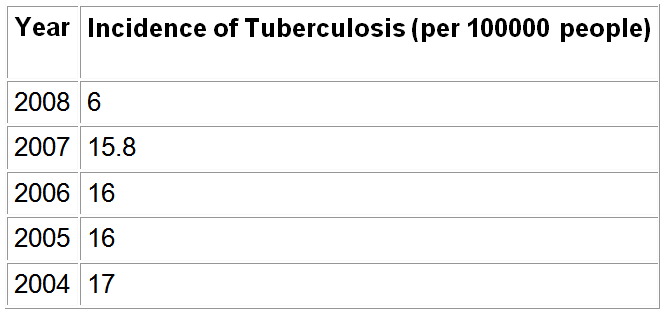
A comparative assessment of the incidence of tuberculosis between countries is important because it is indicative of the policies put in place by countries to curb the spread of the disease. Also, countries with a higher incidence of TB can implement similar policies to those implemented by countries that have managed to reduce their rates of TB.Table 1: Incidence of Tuberculosis in the UAE (per 100000 people) (Source: The World Bank, 2011).
Conclusion
Tuberculosis is a global pandemic with a lot of challenges to global health care. Tuberculosis mainly affects individuals in sub-Saharan Africa and Asia. A strong link between the agent, the environment, and the host increases the chances of infection with the TB causing bacteria.
For a long time now, research has demonstrated a strong association between poverty and TB, and because it mainly affects individuals when they are most productive, TB is important because it affects the overall productivity of the global workforce, and this may result in increased poverty.
There is a need for government to provide access to an affordable cure for TB. Also, individuals should be educated on how to reduce the incidences of contracting TB.
Reference List
Anderson, L., Moore, J., & Kruijshaar, M., et al. (2010). Tuberculosis in the UK: Annual report on tuberculosis surveillance in the UK 2010. London: Health Protection Agency Centre for Infection.
Dhuria, M., Sharma, N., & Ingle, G. K. (2008). Impact of tuberculosis on the quality of life. Indian journal of community medicine, 33(1), 58-59
Horwitch, C. (2004). Tuberculosis: Global Impact and Drug Resistance.
Jasmer, R. M. Nahid, P.,& Hopewell, P. C. (2002). Clinical practice. Latent tuberculosis infection. N Engl. J. Med, 347(23), 1860-6
Khalaf, H. (2009). Experts say tuberculosis is still a threat. Web.
Madison, B. (2001). Application of stains in clinical microbiology. Biotech Histochem, 76(3), 119-25
National Tuberculosis Control Program. (2010). Manual of tuberculosis control. Web.
Niemann, S., Richter, E., Dalugge-Tamm, H., Schlesinger, H., Graupner, D., Konigstein, B., Gurath, G., Greinert, U., & Rusch-Gerdes, S. (2000). Two cases of Mycobacterium microti derived tuberculosis in HIV-negative immunocompetent patients. Emerg Infect Dis, 6(5), 539-42
The World Bank. (2011). Incidence of tuberculosis (per 100,000 people). Web.
World Health Organization. (2001). Guidelines for social mobilization: a human rights approach to tuberculosis. Web.
World Health Organization. (2009). Epidemiology. Global tuberculosis control: epidemiology, strategy, financing. Web.
World Health Organization. (2010). Tuberculosis Fact sheet N°104″. Web.