Case study 2 – Short answer questions: word count and referencing stated where required
Read each question carefully and ensure you answer each part.
You have been asked to attend to the dressing of Johns wound. What would be a suitable dressing to use on Johns wound?
The dressing choice for the wound may be affected by various factors, including a patient’s age, available resources, costs, convenience, and so on. In this case, such moist dressing as Hydrocolloid should be prescribed due to its ability to absorb moisture and maintain a moist wound bed environment. Since it is absorbent, it provides moderate autolytic debridement and acts as the wound filler. For the given patient, it is especially important to change dressing every 3-5 days to eliminate excessive exudates formation. In addition, the patient’s paper thin skin requires the use of an adhesive remover.
State the goal of this treatment as per Q1a – what are you trying to achieve by maintaining a moist wound environment (max 80 words, reference)?
The creation of a moist wound environment promotes an ideal condition that has a beneficial effect on the wound healing processes. Moisture is required for the growth of cells, namely, for their growth, division, and migration at an increased rate, which provides the most favorable conditions for the formation of a new tissue (Harvey & Haigh, 2016). During this phase of the wound process, a watery medium with a certain content of nutrients and vitamins is necessary for metabolism in cells and their growth. The paramount task here is to prevent infection of the wound and stimulate an effective and stable healing process.
State whether John required a primary or secondary dressing, or both, and provide a rationale for your choice (max 70 words, reference)
Secondary dressing is more moisturising
The primary dressing is associated with the direct contact with the pressure ulcer, while the secondary treatment may be used to cover the former to provide a more moisturizing environment. Beldon (2007) states that the primary dressing may be removed if it is contaminated and changed by the antimicrobial dressing. For the given patient, it is useful to consider the secondary dressing such as foam to foster re-epithelialisation. Foam advantages, including that it is thermally insulating and impregnable, seem to be relevant to this patient’s needs.
Most infections agents are micro-organisms, these include (choose one answer):
- Bacteria, viruses, Soil, protozoa and prions
- Bacteria, Candida, fungi, protozoa and prions
- Bacteria, viruses, fungi, protozoa and prions
- Bacteria, viruses, fungi, protozoa and dust
Match the common fungal infections with their major reservoir.
Common fungal infection: Candida albicans, Aspergillus organisms.
Match the common viral infections with their major reservoir.
Common viral infection, Hepatitis A virus, Hepatitis B virus, Hepatitis C virus, Human immunodeficiency virus (HIV), Herpes simplex virus (type I).
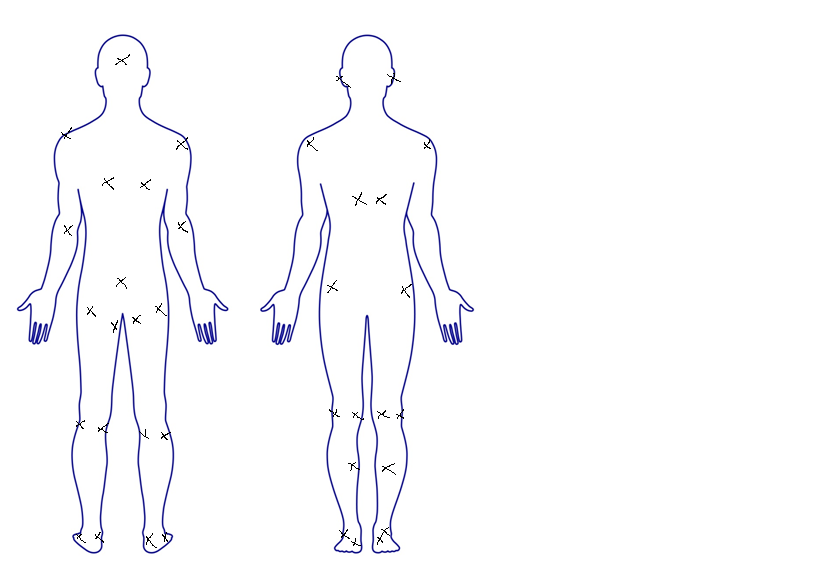
On the picture below, place an X on each of the areas that pressure sores can develop.
State 4 pressure relieving devices that may be used for John either in hospital or when he goes back to the aged care facility
Pressure relieving devices
In the treatment of pressure sores, a complex approach is always necessary to address the underlying cause – the disease that caused the bedsore as well as the factors that contribute to the development of decubitus. At each stage of development of pressure sores, it is important to prevent its progression. In order to prevent further exposure to damaging factors, it is necessary to turn the patient in bed every two hours or use special means to reduce the local pressure on the tissue. The latter may include special beds, mattresses, pillows filled with foam, water, air, gel, or a combination of these materials.
For example, special mattresses are equipped with pressure and vibration control systems, thus providing intermittent pressure. They are connected cylinders with air, which are unevenly inflated and create an alternating pressure at various points.
This patient with limited mobility requires a constant change of body position. This is a critical factor in the prevention and treatment of decubitus. In addition to a mattress, a commode cushion may be used to facilitate urine and faeces incontinence. An anti-suffocation orthopaedic pillow will also be useful to prevent accidental suffocation and increase the patient’s comfort. Since the patient is dependent on a wheelchair, a pressure relief wheelchair set with a t-shaped cushion may be recommended as it provides gentle support for the body in a sitting position.
Match the Ulcer type with their specific characteristic.
Ulcer type: Venous ulcers, Diabetic ulcers, Arterial ulcers, Pressure ulcer.
As John is quite elderly and his mobility has decreased, outline 3 risk assessments you can do, and using your research state 2 common risk assessment tools used in Australia (max 80 words, reference).
John has various risk factors that may deteriorate his current state: age, limited mobility, and the presence of chronic diseases (Frazier & Drzymkowski, 2016). The patient will need a full skin and neurological status examination to determine his response to pain and discomfort. In Australia, the Waterlow score and the Norton scale, which consider age, sex, constitution, nutrition, mobility, and other factors are used (“Medical care of older persons,” 2018). These risk assessments are likely to show that the skin loses its elasticity and the ability to quickly regenerate, the condition of the vessels worsens, and there are disturbances in the function of blood circulation.
There are four stages of pressure ulcer formation each stage has its noted characteristics.
Match the stage with the presentation.
Stage: Stage 1, stage 2, stage 3, stage 4.
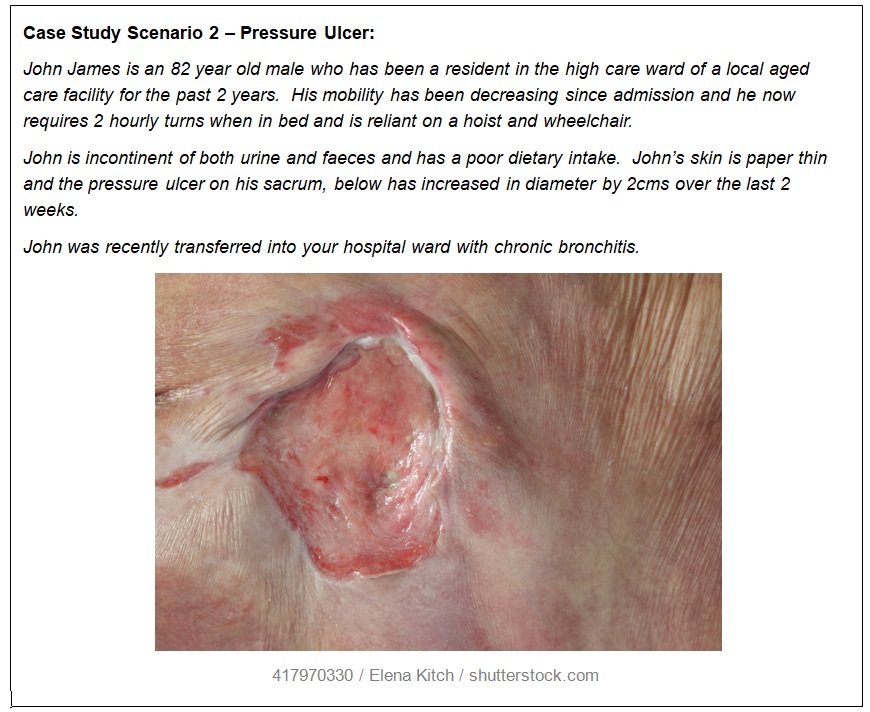
State which stage you think John’s pressure ulcer is at John has stage 2 pressure ulcer because his skin presents a shallow ulcer with pink and whitish bed formation. In addition, one may note that the dermis layer is also exposed. It is evident that the disturbance of microcirculation occurs due to the pressure of the body weight on the surface. Friction and sliding, along with the displacement of tissues, create additional mechanical damage to the skin, affecting its integrity.
When the nurse is assessing Johns wound he/she documents what it looks like using a variety of methods.
Choose from the following words and fill in the blanks with words that match them to the sentences.
Probe, marking pen, wound tracing, a ruler, written consent, Ttransparent acetate grid, clinical wound photography, wound measurement.
Transparent acetate grid provides the most accurate and objective means of assessment and evaluation of wound treatments.
Wound tracing can be used to provide an accurate measurement of the length and width of a wound.
Assessment of the depth or length of a wound can be performed using a probe Using a two-dimensional method such as by tracing the margins of the wound can be assessed using a marking pen and clinical wound photography.
It is essential that written consent is obtained from the patient/relative or carer prior to taking photographs
Johns doctor has ordered a Doppler ultrasound, what does this involve (max 60 words, reference).
Doppler ultrasonography, in this case, includes determining Brachial Pressure Index (ABPI) that is essential to measure peripheral arterial blood pressure. The use of Doppler ultrasound implies allowing the patient to lie for 10-20 minutes, measuring brachial systolic blood pressure and the ankle systolic pressure, and then calculating ABPI (Naude, 2008). In case if arterial disease is suspected, the patient should receive further examination and consultation with vascular specialists.
Identify and discuss 2 effects on wound healing in regards to complex and challenging wounds (max 100 words, reference).
Case Study Scenario 3 – Infected Surgical Wound
Ms Maggie Malone is an obese 52 year old female, who was admitted to the orthopaedic ward for a total left knee replacement. Staples were the method of wound closure.
Ms Malones’ medical history reveals that she is a heavy smoker, smoking at least 30 cigarettes / day and was diagnosed with Diabetes type 2 around 4 years ago, but has not been following a recommended diet.
Day 5 post-op: Maggie is complaining of pain in her left knee, she is febrile 38.7C and an increase in discharge from her wound on her dressings is apparent. On removal of the wound dressings, the wound appeared reddened and inflamed; staples are insitu; an open 1.3cm gap at the lower end of the wound was obvious and is oozing purulent fluid. A wound swab is taken and results show a Methicillin-resistant Staphylococcus aureus (MRSA) infection.
On reading the surgeons’ instructions: “Antibiotics to be commenced; Wound cavity to be dressed daily with Dressing as per directed by wound specialist.
Ms Malone is reviewed by the wound management nurse who documented the following:
“Nursing: Wound to heal by secondary intention. Wound cavity measures 13mm long x 10mm wide and 8mm deep, extending to the subcutaneous tissue layer. Wound bed consists of 100% granulation tissue; is malodorous and is oozing a moderate amount of haemopurulent exudate. Staples to remain insitu until day 10 post-op“

Case study 3- Short answer questions: word count and referencing stated where required
Read each question carefully and ensure you answer each part.
Q1a. Maggie’s Husband comes to visit and he has asked you to explain Maggie’s infection, how she got it and how long will she have it for, to be able to explain to Maggie’s husband you need to understand the chain of infection
Listed are the 6 elements required for a disease to be spread (start with infectious agent). Label the following chain of infection diagram with these elements in the correct order.
Beside each element state how it applies to Maggie’s wound
- Infection Agent
- Susceptible host
- Portal of exit
- Reservoir
- Mode of transmission
- Portal of entry
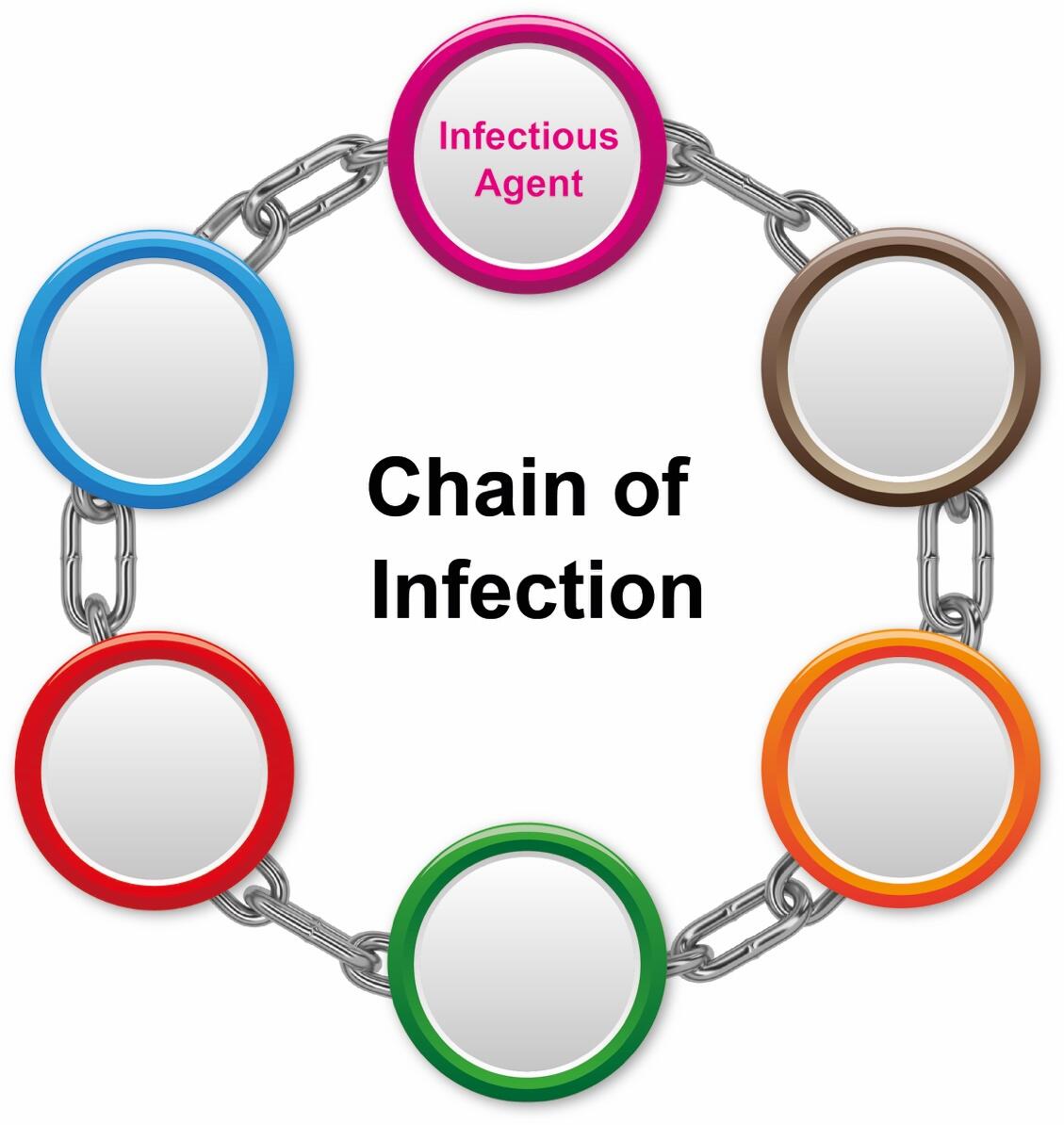
- Step 1 – Infectious agent – the presence of such an agent is the key cause of inflammation. In this case, the patient has Methicillin-resistant Staphylococcus aureus (MRSA) infection that belongs to healthcare-associated infections (HAIs).
- Step 2 – Reservoir – it is the habitat that is beneficial to the infection development. Maggie has the mentioned human reservoir that seems to be transferred through a nurse’s hands or that of her husband.
- Step 3 – Portal of exit – it is the way by means of which a pathogen leaves its host and reaches the newly infected person. MRSA may be transmitted through open sores or wounds.
- Step 4 – Modes of transmission – there are several routes of the infection transmission, incluidng direct (direct contact or droplet spread) and indirect (vehicleborne, airborne, and vectorborne) ones. In case of the given patient, it may be only either the direct contact with a person having MRSA or the contaminated surface.
- Step 5 – Portal of entry – the manner the infection enters the body of a person refers to the portal of entry. Frequently, a pathogen uses the same portals of exit and entry. In Maggie, it may be an open wound or surgical incision.
- Step 6 – Susceptible host – it depends on such factors as the patient’s age, health condition, chronic disease, and so on. The host’s susceptibility is determined by the ability to resist the infection. Since Maggie is a surgery patient, she is vulnerable to MRSA due to the weakened immune system.
Using the above model, it could be suggested that this is a hospital acquired infection (HAI).
Please provide a brief discussion on how you would explain this to Maggie’s husband. Provide this education as though you were speaking to the client’s husband. (Max 80 words)
Hi! My name is Jane, and I am the nurse managing your wife. I guess that you need to know more about her MRSA, so let me tell you about its development and treatment. I understand that you would like to know how she acquired it. MRSA is usually transmitted to patients through a nurse’s hands or the contaminated surface. Your wife is now prescribed with antibiotics that combat with the infection by preventing the growth of bacteria, and it is expected that significant healing progress will be achieved within the next week.
Tick true or false for the following in regards to the bodies defence mechanisms against wound infections
Discuss in terms that you can understand – the immune response in regards to infections. (Max 100 words, reference).
The internal environment of the body is protected by mechanisms of a specific immune response. These selective mechanisms are acquired by the body after contact with a specific foreign substance called antigen. For example, there are humoral (B-lymphocytes) and cell-mediated immunity (T-lymphocytes) (Plantinga et al., 2013). The activated T-lymphocytes enter the bloodstream, from which they migrate to the peripheral lymphoid organs. They return to the bloodstream for recycling until they meet their specific antigen. T-cells are activated when they interact with a specific antigen on the surface of antigen presenting cells (APC). In their turn, B-cells function as part of humoral immune response to a specific antigen by secreting the corresponding antibodies (Plantinga et al., 2013).
Standard and Additional precautions – Using the word bank complete the sentences in regards to precautions. (fill in the blanks).
Word bank: Mucosa, airborne, fluids, single, all, contact, suspected, infection, skin, known, droplet, co-horted.
Maggie requires both standard and additional precautions, standard precautions are infection control practices used for all patients, regardless of their known infection status.
Standard Precautions dictate that personal protective equipment (PPE) must be worn when there is a risk of contact with body skin, non-intact fluids, or mucosa.
Infection may be transmitted in various ways. The 3 transmission categories are airborne, contact, and droplet.
Maggie’s type of transmission is contact.
Transmission-Based Precautions are infection control practices used for patients with known or suspected conditions.
As Maggie has MRSA, an infectious condition she would require additional precautions and should be nursed in a single room or co-horted in a room with a patient with the same infectious condition.
As stated in the case study Maggie had a wound specimen taken. The following pictures are 16 steps of collecting a wound swab for micro-culture and sensitivity (M/C/S). Number the steps on the diagrams from 1 to 16 in the correct order.
The following is the correct order for swabbing for micro-culture and sensitivity (M/C/S):
- Examine the pathology request form and identify a specimen to be gathered
- Explain procedure, receive consent, evaluate pain, and suggest analgetic means
- Prepare equipment
- Fulfill pathology request form, including patient details and that of specimen
- Provide hand hygiene
- Apply personal protective equipment (PPE), if required
- Swab the whole wound for 30 seconds over clean granulation tissue
- Put swab to container and make sure not to contaminate swab tip
- Label specimen instantaneously to specify a patient and specimen
- Place specimen, request slip in biohazard bag, and send to laboratory
- Moisten tip of swab with sterile water
- Clean the wound to remove old drainage and normal flora
- Provide hand hygiene
- Remove gloves if worn
- Document in Progress Notes
- Await results and follow-up
Who would you discuss the results with when they are sent through to the ward?
The results of the laboratory examination are to be discussed with the the wound management nurse, the doctor, and the patient. It should be stressed that it is essential to ensure that the treatment corresponds to Maggie’s health needs and adjust it, if required. In addition, the patient should also be aware of her current health status to understand further treatment and its role in her health.
What impact will the following issues have on Ms Malones’ wound healing and her activities of daily living? Including psychological impact.
Put each of the above issues under a heading and discuss each in detail. Support each issue with research and a clear rationale (reason) for why it will affect her healing. This question is looking for your ability to problem solve and critically think. (Max 150 words, reference)
Poor Nutrition
Harper, Young, and McNaught (2014) state that malnutrition or specific nutritional events can have a profound effect on wound healing after injuries and surgeries. People with chronic diseases (for example, Maggie with diabetes and the infected wound) experience nutritional deficiencies. The energy as well as anti-inflammatory and wound-healing properties of carbohydrates, proteins, fats, vitamins, and minerals for metabolism positively affect the process of healing wounds (Harper et al., 2014).
Smoking
In those patients who smoke, the rejection and necrosis of tissues are more likely than in non-smokers. The reason for delayed wound healing is that nicotine causes vasoconstriction, which leads to oxygen starvation of tissues, while wound healing requires good blood supply (Harper et al., 2014). In addition, tobacco causes the formation of carboxyhemoglobin in the vessels.
Diabetes
Stem cells and cellular plasticity are required to provide wound healing. While diabetes impacts by affecting blood vessels and the immunity system of the body, which makes it difficult to heal wounds, there can be neuropathy (Harper et al., 2014). In this condition, long-term healing of wounds and cuts is observed, which is caused by pathological changes in the nerve endings and impaired phagocytes, as a result of which the lower extremities suffer.
Develop a nursing plan of care for Ms Malone. Your care plan must follow a nursing problem solving approach using the table below.
Give one nursing intervention for each problem stated below i.e. a total of 5 nursing interventions that you would put into place to assist Ms Malone with the following problems. (Max 300 words).
Support each intervention with a rationale/reason, evaluation and a reference.
Problems
- the location of her wound
- activities of daily living
- reduced mobility
- Pain
- Referral needs – which other health team members both within and outside the hospital environment would be involved in the care of Ms Malone.
General Questions
Identify and provide a brief description regarding the intention of the 2 standards that could relate specifically to wounds and infections (max 60 words)
The standard 3, Preventing and Controlling Healthcare Associated Infections, implies the prevention of hospital-acquired infections based on evidence-based strategies, which should be implemented by clinicians and other related staff members. The standard 8, Preventing and Managing Pressure Injuries, target the prevention of pressure ulcers as well as their management by focusing on evidence-based resources and comprehensive support of a team of care providers.
Outline the difference between an acute wound and a chronic wound (max 40 words, reference). Acute wounds are caused by surgery or trauma, while chronic wounds result from pressure or chronic diseases. If acute wounds such as gaze, cut, or surgical wound pass through the standard healing stages (hemostasis, inflammation, proliferation, and remodelling), chronic wounds require much more time to heal them (Frazier & Drzymkowski, 2016).
Review the following case studies and underline if you think it is either an Acute or chronic wound.
Jack Sparrow has a surgical wound with a Jackson Pratt drain, which of the following are correct in regards to management of jacks drain (Tick 4 correct answers.).
- Check for infection
- Maintain bulb patency as per Drs Orders
- Immediately remove if you think it is blocked
- Adhere to facility policy and procedures when caring for a Jackson Pratt Drain
- Document the amount of drainage
- No need to check the connections as this is a closed system
Provide a brief outline in regards to the historical development of contemporary wound management strategies (Max 150 words, reference).
The earliest information on the treatment of wounds was found on ancient Mesopotamian tablets about 2500 BC, as stated by Daunton, Kothari, Smith, and Steele (2012). The washing of wounds with water and milk followed by the application of dressings with honey and resin is noted.
Hippocrates put forward and substantiated the basic principle of purulent surgery: in his works, the formulation of inflammation is given, and the application of both dry bandages and wetted with wine or vegetable oil is mentioned. Hippocrates considered air to be a source of infection, so when dressing, he always used boiled water and linen dressings and also demanded that a surgeon’s hands and dressings be clean (Daunton et al., 2012).
One may state that Chinese and Egyptians used herbs to heal wounds. Advances in the field of antiseptics and asepsis as well as the successes of microbiology and the empirical experience of researchers have become the scientific foundation for the development of methods for today’s wound treating.
Research your community or online to identify educational resources, community services, and or professional organisations associated with wound management and prevention programs located in Australia. List a minimum of 2.
There are several organizations and community services that provide support and research regarding wound treatment in Australia. Australian Wound Management Association (AWMA), also known as Wounds Australia, is one of the organizations that present advocacy, research, education opportunities to clinicians, nurses, patients, and their families. According to the official website of the mentioned organization, it promotes an interdisciplinary collaboration with the aim of healing wounds (“Welcome to Wounds Australia,” 2017). It provides the educational resources and a strategic plan that details the very process of managing both acute and chronic wounds.
Wounds Australia sets the standards for caring about patients with wounds, including all the stages of wound development and follow-up. At the same time, one may note programs and conferences that target one or another related issue. For example, Wounds Australia National Conference 2018 focuses on discussing the recent advancements occurred in the given field as well as identifying further needs (“Welcome to Wounds Australia,” 2017). Considering that the modern environment is marked by the rapidly developing technology, its implementation will also be examined.
The Wound Healing Institute Australia is one more Australian organization that is a not-for-profit charitable care facility. It aims at the prevention, treatment, management, and follow-up of wounds based on the evidence-based approach. The Wound Healing Institute Australia offers the Online Wound Education Program to help health care professionals in deepening their knowledge and skills regarding wound treatment in Australian settings.
Implementing modern technology in the education process, the organization strives to provide the most relevant training sessions. The Wound Advisory Service assists clinicians and nurses in conducting research and introducing scholarly discoveries in practice. A set of consultancy services is also offered by the mentioned organization in terms of the compliance with the national standards, strategic planning, and staff training.
Today Independence Australia is another community-based organization that focuses on people with disabilities and their health needs. In particular, wound treatment is among those services that are provided to the mentioned patients. The official website presents guidelines on prevention and treatment of different wounds, which is supported by patient education services. Most importantly, Today Independence Australia targets the provision of official statistics associated with the given topic.
For example, the prevalence, morbidity, and mortality rates are demonstrated to allow the interested parties to understand the existing situation with wounds in Australia. Such an approach to promoting awareness of wound management is an important step towards decreased levels of wound formation as well as complications occurring after either acute or chronic injuries. Thus, one may note that a range of organizations provide credible and relevant information, programs, and services related to care about patients having different wounds.
References
Beldon, P. (2007). What you need to know about skin grafts and donor site wounds. Wound Essentials, 2, 149-155.
Daunton, C., Kothari, S., Smith, L., & Steele, D. (2012). A history of materials and practices for wound management. Wound Practice & Research: Journal of the Australian Wound Management Association, 20(4), 174-186.
Frazier, M. S., & Drzymkowski, J. (2016). Essentials of human diseases and conditions (6th ed.). St. Louis, MO: Elsevier Health Sciences.
Guo, S. A., & DiPietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219-229.
Harper, D., Young, A., & McNaught, C. E. (2014). The physiology of wound healing. Surgery, 32(9), 445-450.
Harvey, K. E., & Haigh, D. A. (2016). Wound dressings: Moist dressings. Dermatological Nursing, 15(3), 10-16.
Medical care of older persons in residential aged care facilities. (2018). Web.
Naude, L. (2008). Chronic wound management diabetic, venous and arterial ulcers-a summary: Wound care. Professional Nursing Today, 12(2), 18-24.
Plantinga, M., Guilliams, M., Vanheerswynghels, M., Deswarte, K., Branco-Madeira, F., Toussaint, W.,… Hammad, H. (2013). Conventional and monocyte-derived CD11b+ dendritic cells initiate and maintain T helper 2 cell-mediated immunity to house dust mite allergen. Immunity, 38(2), 322-335.
Tan, M., Law, L. S. C., & Gan, T. J. (2015). Optimizing pain management to facilitate enhanced recovery after surgery pathways. Canadian Journal of Anesthesia, 62(2), 203-218.
Tricco, A. C., Antony, J., Vafaei, A., Khan, P. A., Harrington, A., Cogo, E.,… Straus, S. E. (2015). Seeking effective interventions to treat complex wounds: An overview of systematic reviews. BMC Medicine, 13(1), 89-112.
Welcome to Wounds Australia. (2017). Web.