Introduction
Marijuana has been used for several thousand years in various directions. In the West, for the first time, medical use became known thanks to the work of Professor O’Shaughnessy, who personally observed the process of her treatment in India (Cerdá et al. 167). After a series of experiments, he began to use it for patients with rabies, epilepsy and tetanus. Over the following years, the opinion of experts has constantly been changing, and discussions about the ratio of benefits and harms are still ongoing. Evidence of medical use of marijuana varies from proven clinical cases to speculative claims. Despite its long history and positive feedback from patients in various fields, one must not forget that cannabis has psychoactive properties, so its turnover should be limited. The legal status and availability of the remedy are ambiguous for many countries.
Forms of Medical Cannabis
The Cannabis sativa plant contains more than 100 compounds, including terpenes, flavonoids and – most importantly for medical purposes – cannabinoids (Ali 25). The most common cannabinoid is delta-9-tetrahydrocannabinol (THC), which has psychotropic properties and is capable of causing euphoria (Grassa et al. 1678). The next most common cannabinoid is cannabidiol (CBD), which is not psychotropic. THC and CBD are the most studied cannabinoids. Evidence suggests that other cannabinoids and terpenoids may also have potential medical applications and that different cannabis compounds may work synergistically, enhancing each other’s effect.
Opinions on the Legalization of Medical Cannabis
Opponents
Among psychiatrists, there are opponents of the use of marijuana. They warn that legal cannabis, even with limited use in medicine and veterinary medicine, will easily get out of control and will contribute to the additional spread of drug addiction among the population (Nosarieme 293). Opinions are given about the risk of mental disorders, a decrease in long-term memory. The danger is the statement about the harmlessness of marijuana. There is concern that the burden on law enforcement agencies will sharply increase, which will have to deal with the purpose of using cannabis in detainees.
Studies have shown that adolescents who use marijuana have noticed anxiety and deterioration in the educational process (Larkin and Madras 590). Colorado was the first to legalize marijuana in 2012 (Page et al. 145). Scientists at the University of Colorado stated that since legalization, the number of patients admitted to hospitals in a serious conditions caused by cannabis has tripled (Cerdá et al. 169). Opponents of legalization are also confident that legalization will lead to the emergence of a black market for marijuana. It is economically more profitable for producers to trade illegally than to pay taxes to the state and be under its control.
Supporters
Supporters of changing the law emphasize the need to use medical cannabis as an adjunct to pain relief for different illnesses. In addition, they refer to the results of the experience of other countries where there is no ban on marijuana, which has allowed to reduce in drug trafficking on the black market (Ali 25). A number of studies have shown that the crime rate began to drop markedly in the US states where marijuana was legalized (Grassa et al. 1677). For example, in the states bordering Mexico, the number of crimes decreased by 13% (Nosarieme 294).
Results of Cannabis Legalization
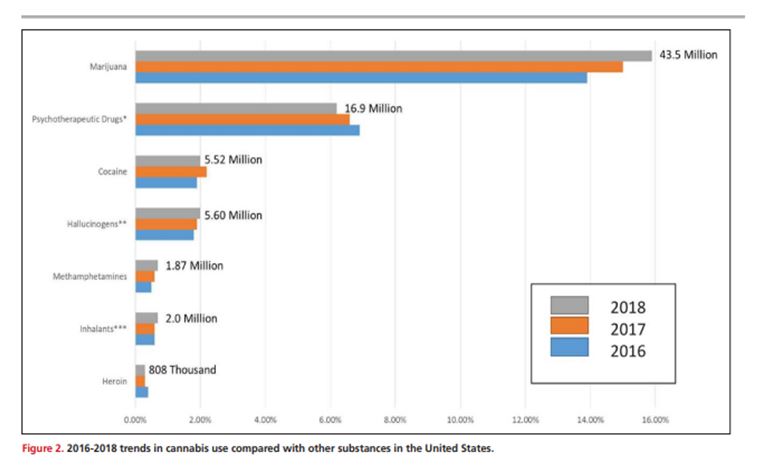
The process was initiated by Uruguay and Canada, which allowed the use of marijuana in 2001 (Larkin and Madras 579). Smoking is not prohibited for persons over the age of 18 in special places (Page et al. 138). The position of the official authorities is neutral. In some countries, the law allows to have marijuana for one’s own use and to breed from 5 to 15 bushes at home for personal needs (Nosarieme 292). In Colorado, Georgia and Washington in the USA, two years after the legalization of marijuana in 2013, there were fewer patients going to drug treatment centers (Ali 21). The suicide rate has hardly changed. According to police statistics, employees have received more opportunities to investigate serious crimes and preventative law enforcement activities. Consumption of other narcotic drugs has not increased (as shown in the graph) and alcohol consumption has decreased.
However, it is also possible to highlight the negative consequences of the legalization of marijuana. The Canadian Association of Psychiatrists demands that the sale of cannabis be restricted to 25 years (Grassa et al. 1669). Doctors say that the passion of young people affects the development of thinking abilities, memory, attention, and learning ability and destroys intelligence. In addition, marijuana becomes a catalyst for people at risk for mental illness. These include people with stressful work, stress and dysfunctional heredity.
The Use of Cannabis in Medicine
Chemotherapy
Chemotherapeutic drugs are administered to cancer patients in courses for several weeks. They are effective but highly toxic; treatment is accompanied by severe side effects that worsen the quality of life of patients. One of the unpleasant consequences is severe nausea and vomiting, which are almost impossible to control. Patients try to eat less, and can not stand the sight and smell of food, which leads to exhaustion and depression. Sometimes they interrupt therapy, despite the deadly risk.
Antiemetic drugs relieve the condition, but they are not always effective, and their prolonged use causes complications. Marijuana has been proposed as a less harmful alternative. Since 1985, oncologists have been allowed to use synthetic tetrahydrocannabinol in capsules, but Alfred Chang’s research has shown that bioavailability when smoking is much higher (Larkin and Madras 578). Cannabis treats nausea by increasing appetite (which prokinetics do not do), and also has an analgesic effect, which potentially allows to give up narcotic analgesics.
Multiple Sclerosis and Epilepsy
Clinical manifestations of multiple sclerosis are diverse and depend on the localization of foci of myelin destruction. Etiotropic therapy is absent; the disease is irreversible, so combinations of expensive symptomatic drugs are used. Marijuana relieves tremors and partial loss of coordination. There have been documented cases when cannabis effectively coped with focal seizures in epilepsy (Cerdá et al. 171). Even under the condition of illegal purchase, it was cheaper than traditional treatment. Anticonvulsive properties also helped with tremors of various origins (infections, organic pathology of the central nervous system, and dystonia).
Anorexia in the Treatment of HIV/AIDS
Taking antiretroviral drugs can depress digestion and cause nausea, which increases the risk of exhaustion for patients who are already losing weight due to the disease. Cannabis not only excites hunger but enhances the taste and pleasure of food. After the 1971 studies, Dronabinol was allowed to be used in the USA since it turned out to be safer and more effective in comparison with Megestrol (Page et al. 149). Cannabis treatment of anorexia with HIV infection Marinol is possible only in some foreign countries by prescription. Many patients resort to ordinary smoking marijuana. They indicate that it relieved symptoms more effectively than a synthetic analog.
Chronic Pain
Traditionally, chronic pain was treated with opiates and synthetic analgesics. This led to dangerous complications in the form of gastrointestinal bleeding, ulcers and renal-hepatic insufficiency. The combination of sedative and analgesic action allows the use of cannabis for pathologies such as osteoarthritis and phantom pain after limb amputation. Although marijuana is inferior to opiates in the power of pain relief, smoking on demand is accompanied by fewer side effects and rarely causes addiction. Cannabis is becoming a means of choice for people suffering from migraines, as many of them simply do not help analgesics.
Rare Cases of Medical Use
Cannabis helps only a small part of patients, so it is rather an exception to the rule. This is due to the use of pharmaceutical drugs in the treatment of fairly rare symptoms and side effects. There is reason to believe that marijuana is likely to benefit in the treatment of diseases, the list of which is presented below.
Glaucoma
In an experiment at the University of California, the properties of cannabis were found to reduce intraocular pressure and lacrimation. The effect after smoking persisted for 4-5 hours, while the pupils reacted normally to light and the quality of vision did not change (Nosarieme 295).
Atopic Dermatitis
Marijuana helps to suppress itching and irritability associated with the disease when the effectiveness of antihistamines and corticosteroids is limited or there are contraindications to them.
Labor Pains
Pregnant and lactating women should generally avoid the use of medications, as there is a risk of poisoning the child. However, in India and African countries, marijuana is used to relieve labor pains due to the banal lack of normal medications.
Depression, Psychosis and Other Disorders of The Emotional Sphere
The use of cannabis, in this case, is ambiguous. On the one hand, it has been used for years past to treat melancholy. On the other hand, chronic use can cause and exacerbate mental disorders.
Asthma
Cannabinoids in the experiment showed a weak bronchiolitis effect in the absence of side effects characteristic of beta-agonists and steroids. However, smoking is contraindicated because of its irritating properties; only oral administration is suitable.
Insomnia
This is one of the most ancient indications for taking cannabis in various pathologies. Such pathologies can be multiple sclerosis, bipolar disorder, and withdrawal syndrome.
Scleroderma
Due to the pathology of connective tissue, patients suffer from heartburn, difficulty swallowing and nausea, which leads to a decrease in appetite and exhaustion.
Conclusion
People in the last stages of fatal diseases often turn to weak narcotic substances. Cannabis helps to suppress pain, nausea, depression and feelings of fear without causing severe withdrawal or addiction. Therefore, it is pointless to deny its palliative capabilities. Globally, evidence of the use of cannabis in medicine is not systematic. Due to problems with the legality of turnover, doctors are forced to provide unofficial statistics. However, cases of the palliative use of cannabis are massive.
Marijuana is not harmless, so the question of safety should be decided by a doctor. If a patient finds a suitable specialist, they will help choose the right dose and weigh the risks in the long term. The toxic effects of cannabis can be acute and chronic, leading to undesirable consequences. However, no fatal cases of intoxication have been confirmed. The effectiveness of cannabis is individual in each case. It depends on the severity of the causal disease, the characteristics of the patient and the dose. Unfortunately, accurate data is not available, as the illegality of the tool limits research.
Works Cited
Ali, Ola. Association of Cannabis Use with Depressive Symptoms and Cardiovascular Diseases: A Cross-Sectional Analysis. Doctoral dissertation, Ohio State University, 2015.
Cerdá, Magdalena, et al. “Association Between Recreational Marijuana Legalization in the United States and Changes in Marijuana Use and Cannabis Use Disorder From 2008 to 2016.” JAMA Psychiatry, vol. 77, no. 2, 2020, pp. 165-171.
Grassa, Christopher, et al. “A New Cannabis Genome Assembly Associates Elevated Cannabidiol (CBD) With Hemp Introgressed into Marijuana.” New Phytologist, vol. 230, no. 112, 2021, pp. 1665-1679.
Larkin, Paul, and Bertha Madras.“Opioids, Overdoses, and Cannabis: Is Marijuana an Effective Therapeutic Response to the Opioid Abuse Epidemic?” The Georgetown Journal of Law & Public Policy, vol. 17, no. 555, 2019, pp. 555-597.
Nosarieme, Abey. “Cannabis Sativa (Marijuana) Alters Blood Chemistry and the Cytoarchitecture of Some Organs in Sprague Dawley Rat Models.” Food and Chemical Toxicology, vol. 116, no. 15, 2018, pp. 292-297.
Page, Robert, et al. “Medical Marijuana, Recreational Cannabis, and Cardiovascular Health: A Scientific Statement from the American Heart Association.” Circulation, vol. 8, no. 142, 2020, pp. 131-152.