Introduction
Cervical cancer continues to be a significant health problem in the United States. According to the latest statistics by the Centers for Disease Control and Prevention (2022), the US has approximately 13,000 new cases of this cancer annually, and about 4,000 of the diagnosed women die from cervical cancer. Although new screening methods were introduced in the last decades, and women were provided with additional tests, screening rates remain low (Bedell et al., 2020). Therefore, the question of how Advance Practice Nurses can aid patients in undergoing screening arises. Nurses should introduce such initiatives as self-completed test kits that can be used at home for human papillomavirus screening and patient navigation to create a supportive environment for cervical cancer screening.
Describing Quantitative Research
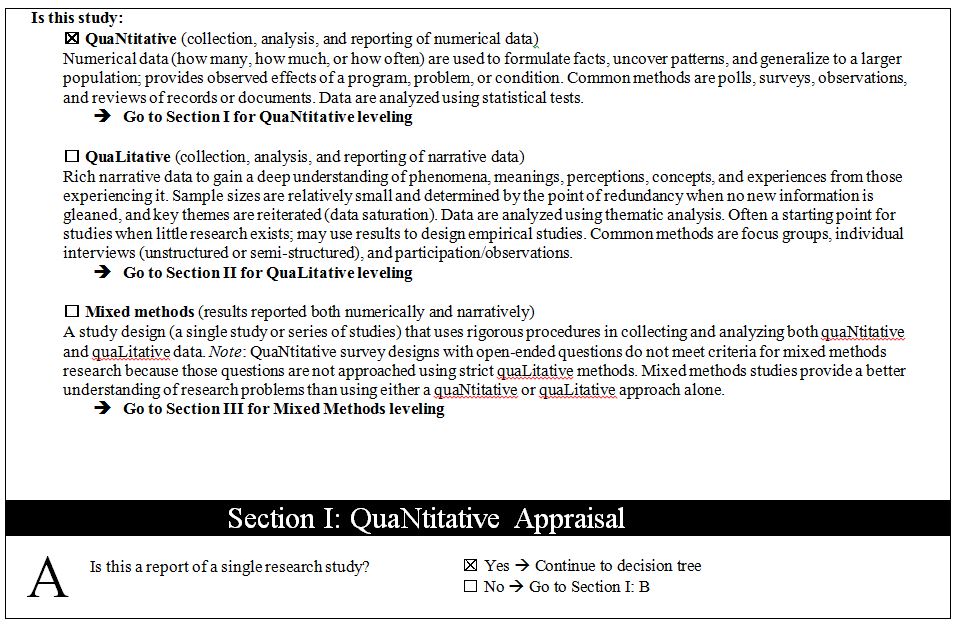
Quantitative research includes studies that approach scientific inquiries with quantifiable measures. In such studies, data is collected for calculations that help answer the research question. For example, one may find a correlation between an independent and dependent variable to see how two or more elements are interconnected (Sürücü & Maslakçi, 2020). Furthermore, quantitative research may help compare group behavior depending on the intervention to which they are exposed (Vu, 2021). Regression and change are also possible investigation goals in this branch of scientific research. Some types of quantitative studies include descriptive, correlational, quasi-experimental, experimental, and more.
To explore the issue of cervical cancer screening, one may look at different types of qualitative research. The problem reviewed is the need to increase cancer screening rates with the help of nurse intervention. Therefore, one needs to look at studies that compare the effectiveness of nursing interventions and usual care regarding screening programs. An experimental study that divides the participants into two or more groups is a type of quantitative research that can support the thesis and provide more information on effective intervention types. Moreover, meta-analyses and systematic reviews of nursing interventions can provide a solid base for further research.
Appraisal Tools, Studies, and Matrix
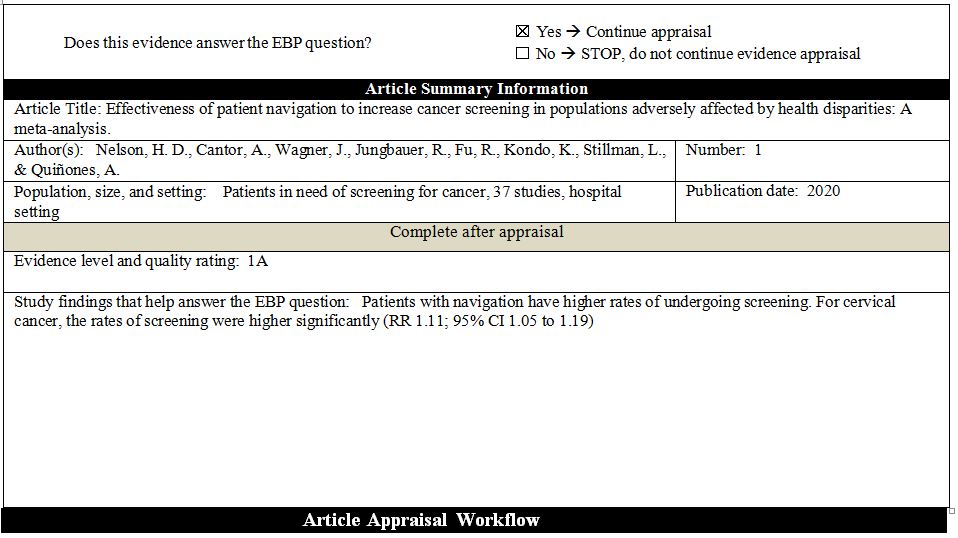
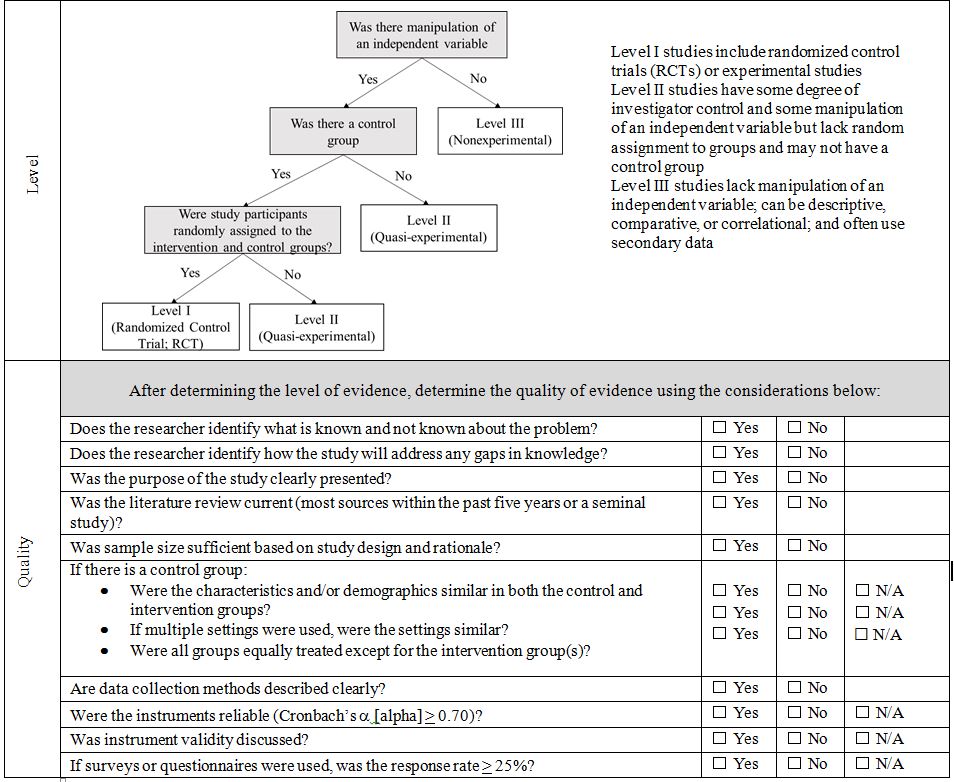
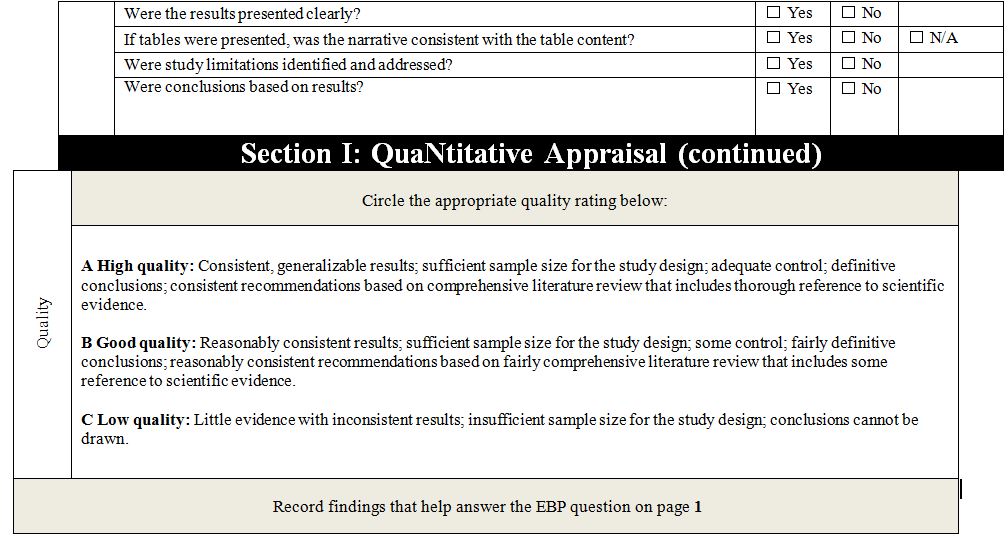
Two studies were chosen for the appraisal and analysis to support the topic of cervical cancer screening. The first one is a meta-analysis performed by Nelson et al. (2020) – the researchers aim to investigate the impact of patient navigation on cancer screening rates among underserved populations. As seen in Appendices A and B, the study shows a high level of quality, producing consistent results. This review was selected as it contains studies on cervical cancer, and its focus on screening rate improvement aligns with the topic of interest.
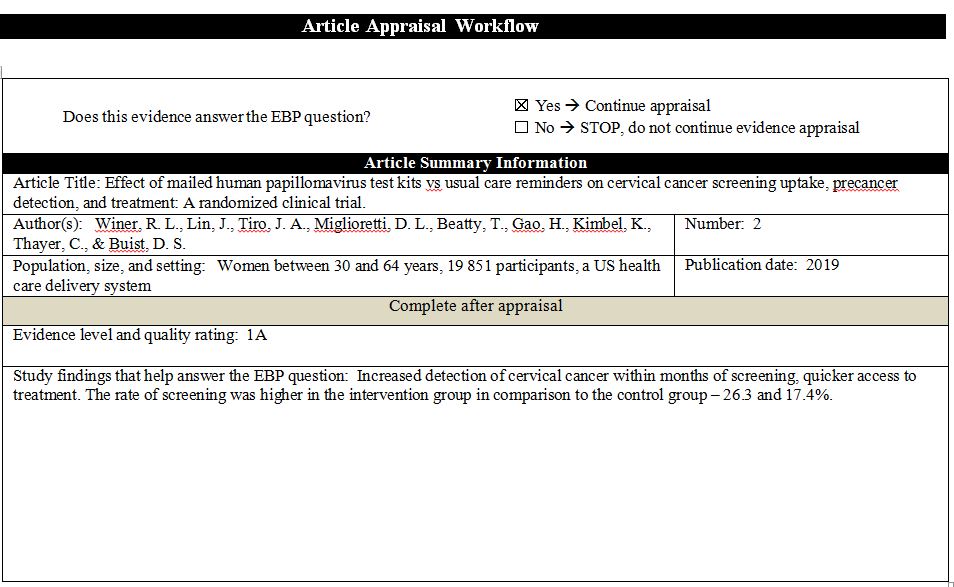
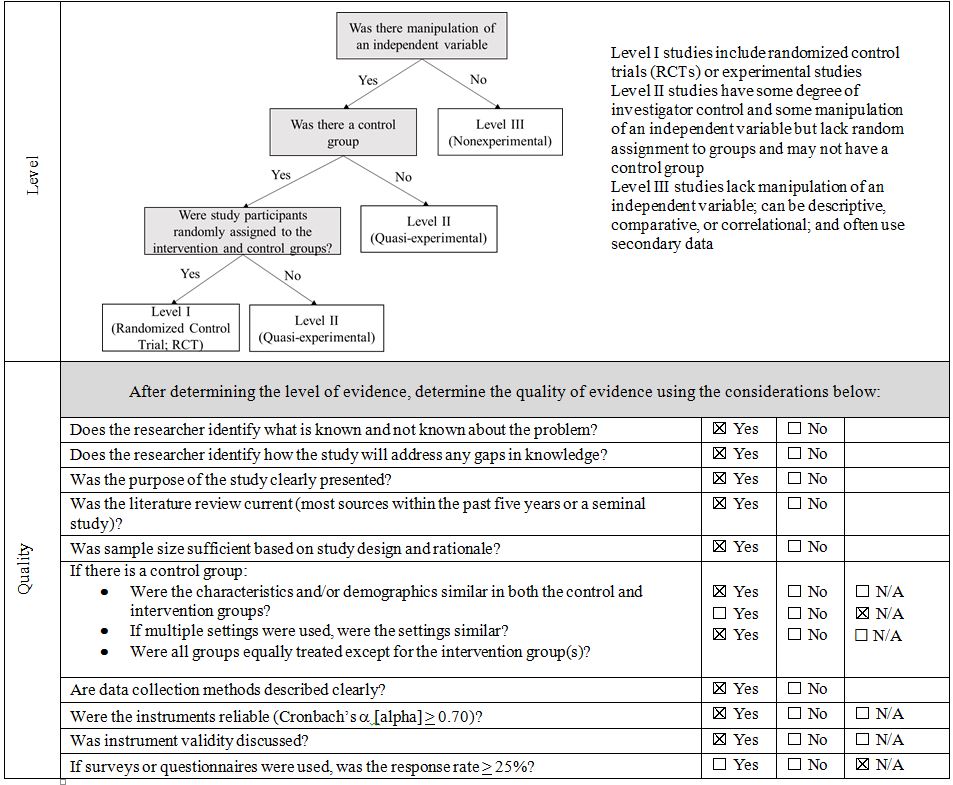
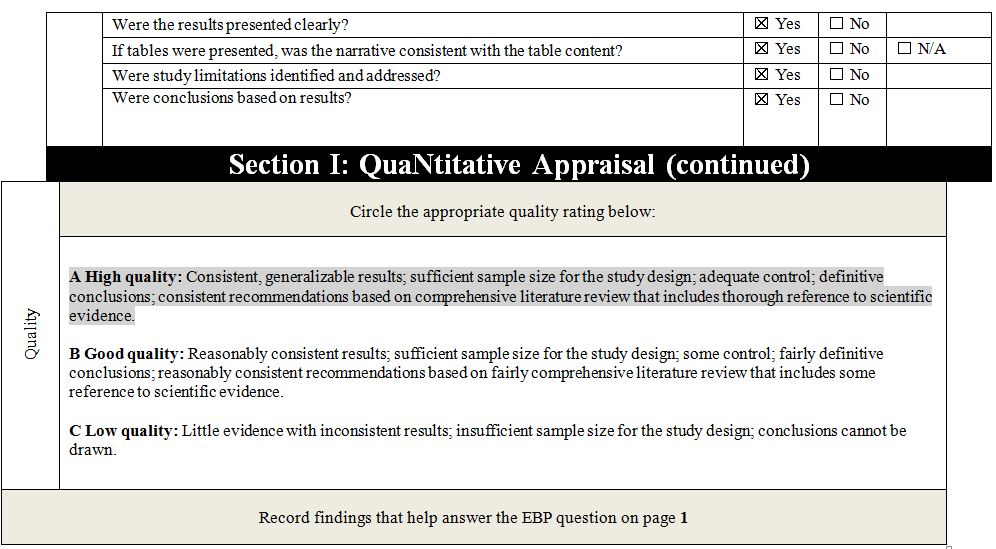
The second article under examination is a randomized controlled study. In the clinical research by Winer et al. (2019), the authors test whether mailing a test kit to patients is more effective than simple reminders to get screened for cervical cancer. Similar to the previous study, Appendices A and B demonstrate the high quality of available evidence. The research was chosen for this review due to its interest in additional measures for improving screening rates and a choice of nursing intervention.
Article Discussion
To understand the selection of sources and appraise their quality, one has to discuss them in more detail. First, in the meta-analysis, Nelson et al. (2020) aim to analyze the outcomes of patient navigation on the participants’ cancer screening rates. Breast, colorectal, and cervical cancer are considered in the study, and patient navigation is defined as “services that improve engagement in healthcare by providing personal guidance through the healthcare system” (Nelson et al., 2020, p. 3028). The research design is a meta-analysis that considers quantitative studies. The investigators introduce a new way of appraising the results by adapting them into one measurement. As a result, the article’s methodology synthesizes evidence and calculates the risk ratio.
The data collection process is described in the article in detail. It is noted that the authors gathered sources from such databases as Ovid® MEDLINE®, PsycINFO®, and SocINDEX (Nelson et al. (2020). The inclusion criteria included randomized controlled trials and observational studies with control and intervention groups. Furthermore, the reviewed sources had to consider vulnerable populations, be relevant to US health and practice, and present clear results of screening rates (Nelson et al. (2020). As a result, the data was collected from 37 articles, including 29 randomized controlled trials and eight observational studies. The validity of the data in the papers and their analysis was checked by comparing the selected studies’ results (Vu, 2021). Articles show consistently high significance, but additional research is necessary due to the variance in rates (Nelson et al. (2020). The instrument’s reliability is based on its transparency and consistency, which is supported by the author’s detailed discussion of its operation.
The results of the meta-analysis show that the screening rates for all types of cancer were positively influenced by patient navigation. While studies analyzing cervical cancer were limited in number, the consistency of the results for the available sources and the outcomes for other types of cancer demonstrate the overall effectiveness of this approach (Vu, 2021). These findings have significant implications for practice as they support the idea of additional measures for engaging patients in cancer screening. The study emphasizes the value of individual approaches to patients and communication’s role in improving patients’ preparedness for regular screening. Based on the factors above, the study’s evidence quality level and the findings’ ratings are high, and the meta-analysis can be marked as IA.
The second source presents similarly high-quality results while testing another method of screening rates’ improvement. In a randomized controlled trial, Winer et al. (2019) analyze whether patients are more likely to undergo hospital cervical cancer screening if they receive home test kits for human papillomavirus (HPV). To complete the study, the researchers identified eligible participants using electronic health records and separated them into control and intervention groups. The inclusion criteria are women between 30 and 64 years old who did not have a hysterectomy and had a clinician within the selected system. The control group receives usual care, including yearly reminders to undergo screening and frequent messages from the clinic. For the treatment group, these activities are supplemented by mailing patients a self-sampling kit that tests for HPV (Winer et al., 2019). Then, the screening rate is compared in the next six months after the initiative.
The data collection process in the second study relied on electronic health records. Two major outcomes were considered: diagnosed and treated precancerous conditions, and other measures included increased test uptake and abnormal results (Winer et al., 2019). As a result of investigating health records, it was determined that the difference between control and intervention groups was significant, with the self-testing kits raising the screening uptake by almost 10% (Winer et al., 2019). These results have high validity due to standardized statistical calculations and electronic records use (Vu, 2021). The implication of this study is the effectiveness of reaching out to patients with opportunities for self-testing instead of calling. The quality of data and the transparent explanations of each step allow one to grade this study as IA on the quality scale.
Applicability to Practice and Future Research
The discussed studies can significantly impact practice and positively influence its quality. Based on the six domains presented by the AHRQ (2022), the findings can enhance safety, effectiveness, and focus on patient-centered care. First, the articles demonstrate ways to improve screening rates and better diagnosing for patients to prevent and treat cancer – a severe condition that endangers the lives of many people. Thus, the conclusions and recommendations support the aim of patient safety. Second, the effectiveness of care is improved by engaging patients in screening and providing timely care. The higher rate of timely diagnoses is a result of both studies, showing the positive impact of the considered interventions. Finally, as the research finds ways to solve a problem in patient outreach, especially among underserved populations, it is consistent with the patient-centered approach to care. The recommendations to communicate with patients and provide them with easy methods of pretesting should be implemented in practice to deliver better care.
Conclusion
Cervical cancer is a significant problem that poses risks to population health. Timely screening remains an issue, especially among women with health disparities. The selected studies offer several options for reaching out to patients to provide them with testing recommendations or tests to engage them in cancer detection and treatment. The articles present reliable evidence of the approaches’ effectiveness and demonstrate that patient-centered and effective care is possible with nursing interventions.
References
Agency for Healthcare Research and Quality [AHRQ]. (2022). Six domains of healthcare quality. Web.
Bedell, S. L., Goldstein, L. S., Goldstein, A. R., & Goldstein, A. T. (2020). Cervical cancer screening: Past, present, and future. Sexual Medicine Reviews, 8(1), 28-37. Web.
Centers for Disease Control and Prevention. (2022). Cervical cancer: Statistics. Web.
Nelson, H. D., Cantor, A., Wagner, J., Jungbauer, R., Fu, R., Kondo, K., Stillman, L., & Quiñones, A. (2020). Effectiveness of patient navigation to increase cancer screening in populations adversely affected by health disparities: A meta-analysis. Journal of General Internal Medicine, 35, 3026-3035. Web.
Sürücü, L., & Maslakçi, A. (2020). Validity and reliability in quantitative research. Business & Management Studies: An International Journal, 8(3), 2694-2726. Web.
Vu, T. T. N. (2021). Understanding validity and reliability from qualitative and quantitative research traditions. VNU Journal of Foreign Studies, 37(3). Web.
Winer, R. L., Lin, J., Tiro, J. A., Miglioretti, D. L., Beatty, T., Gao, H., Kimbel, K., Thayer, C., & Buist, D. S. (2019). Effect of mailed human papillomavirus test kits vs usual care reminders on cervical cancer screening uptake, precancer detection, and treatment: A randomized clinical trial. JAMA Network Open, 2(11), e1914729-e1914729. Web.
Appendix A: Individual Evidence Summary Tool
EBP Question: In women, will additional screening advice from the Advanced Practice Nurse increase the rate of screening for cervical cancer in comparison to usual care?
Appendix B
Research Evidence Appraisal Tool – Source 1
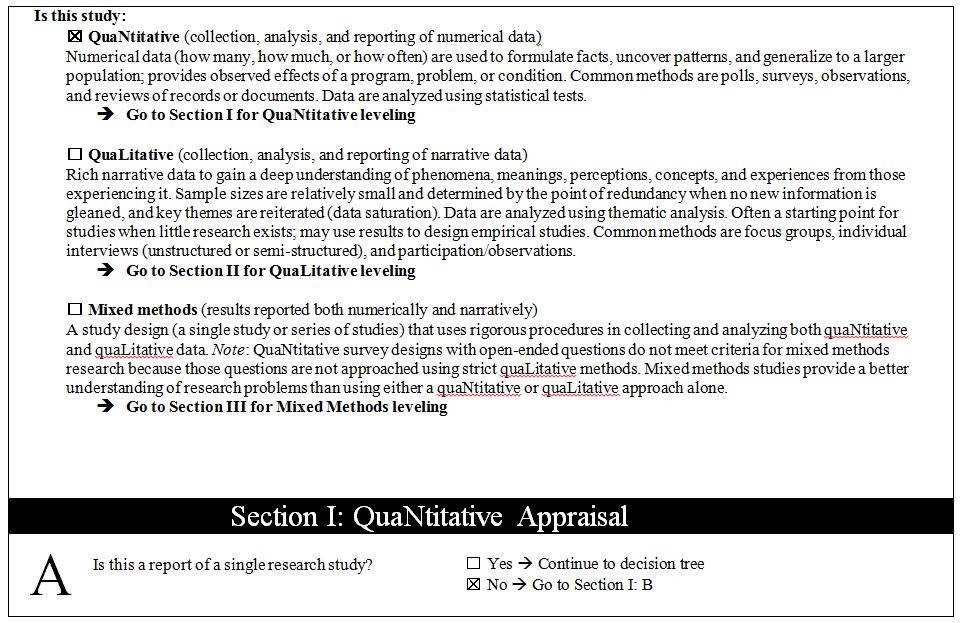
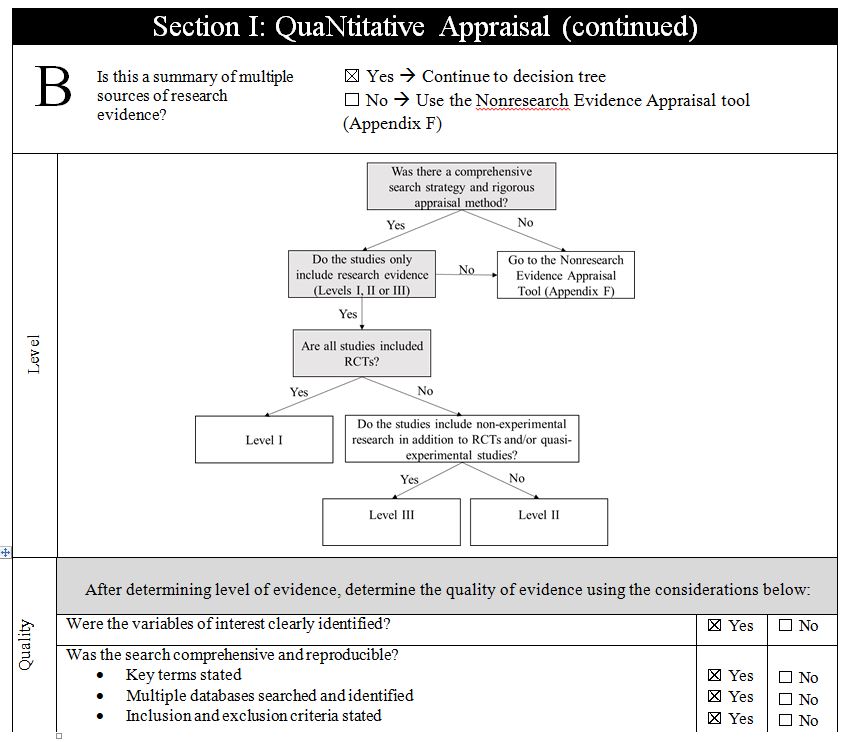
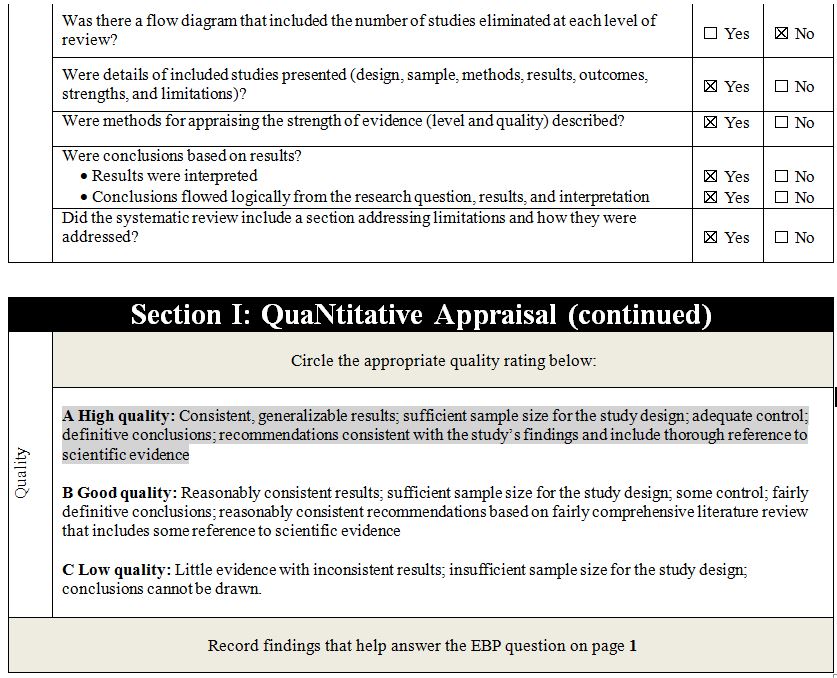
Research Evidence Appraisal Tool – Source 2