- Introduction
- Data and Methods
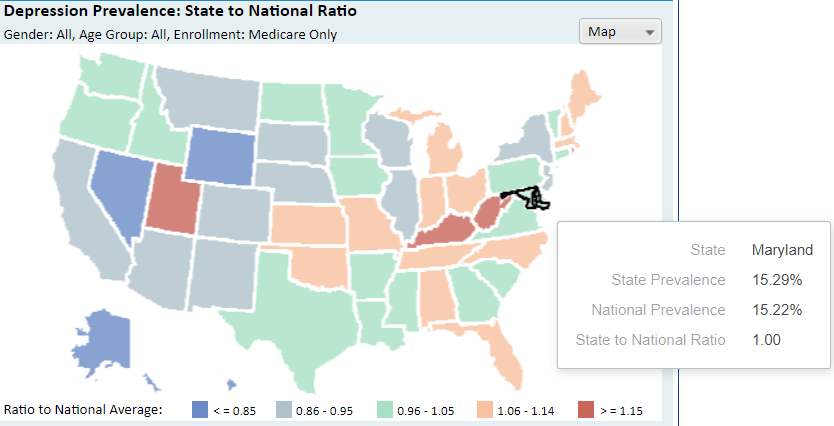
- Prevalence of Depression Within the Medicare Population in Maryland
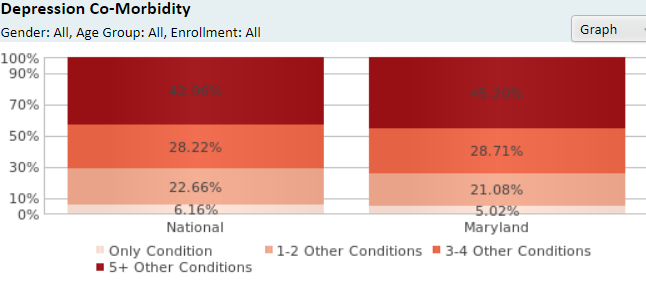
- Comorbidity rate for Medicare Beneficiaries with Depression
- The Difference in Prevalence Rate among Subpopulations in Maryland
- Predisposing, Reinforcing, and Enabling Conditions
- Conclusion and Recommendations
- References
Introduction
Depression is a relatively common mental disorder that appears in different population segments. The condition is rather severe and complex because it has many additional contributing factors to its appearance, and the number of cases increases over time (PGCHealthZone, n.d.). The risk of getting a disease varies depending on the social group and its characteristics. Women tend to suffer from depression more often than men, teenagers’ depressive episodes appear more often than adults and the segment with low income and education levels is exposed more significantly to the condition than those with high-paid jobs (Remington et al., 2016, p. 869). Additionally, sexual and ethnic minorities are subjected to the disorder’s progression due to discrimination and systematic oppression. Depression is a risk factor for developing addictive behaviors and substance use (McKenna, 2021). On the contrary physical illnesses such as heart problems, diabetes or cancer can serve as stimuli for the occurrence of the condition.
Data and Methods
For the research used secondary sources such as scholarly analyses, articles, and data from the government website. The information includes the numbers of people from different risk groups who are affected by depression. The statistics about the prevalence and comorbidity rates of depression are provided from the Medicare Chronic Conditions Dashboard (CMS, 2021) and are portrayed in the table included in the paper. Upon entering the portal, on the land hand-side, the states are listed, it is necessary to select the ‘national’ checkbox and the state for which one wants to see the data comparison, in this case Maryland was selected. Then, there is a graph with various conditions, and it is necessary to select depression. At this point, the graphs and map present the comparison between Maryland and the US national average. At the top of the page, there are options to modify the data. One can select gender as either male or female, age group as either below or above 65 years old, and enrollment as either all, Medicare and Medicaid, or Medicare only. The data and tables shown in this paper are taken using variations of these settings, primarily all under the Medicare only enrollment, other than the age and gender prevalence. Several other CMS data platforms were used for supporting data. CMS data remains as one of the most reliable stemming from a federal agency with reporting data nationally and from every US jurisdiction.
Prevalence of Depression Within the Medicare Population in Maryland
Depression is not an uncommon phenomenon and occurs all over the world among different population groups. The general prevalence of the disease in Maryland among the Medicare population is 15.29% which is virtually similar to the national average of 15.22% (CMS, 2021). Depression has many various aspects that influence its appearance and cause major problems in people’s mental state. There are many causes of depression, starting from the biological to psychological, and often it combines with other illnesses. Sometimes one disease can cause depression, and otherwise, the depression might lead to other health problems. Especially the situation worsened during the Coronavirus pandemic and caused massive mental issues among the population. Medicare beneficiaries faced economic difficulties and complications with accessing healthcare and ensuring certain basic needs (Balasuriya et al., 2021). Notably, according to CMS, the prevalence of the general rate in Maryland is 18.02%, a 3% increase from the ‘Medicare only’ indicator. Remington et al. (2016) links depression with low socioeconomic achievement and social barriers such as ethnic discrimination that may lead to it. People suffering with mental health issues, including depression, are typically poorer, lack stability (unable to keep a job, relationships), and have negative responses to stressors. While that position may qualify them for Medicare or Medicaid, the rate of healthcare utilization or adherence is likely much lower, worsening prevalence of the chronic conditions and comorbidities.
Comorbidity rate for Medicare Beneficiaries with Depression
The comorbidity rate aims to identify how many conditions occur along with the selected illness. According to the data retrieved from CMS, 45,2% of beneficiaries from Medicare struggle simultaneously with five or more conditions besides the depression itself. Approximately 28.71% have 3-4 diagnoses, 21.09% have 1-2 diseases, and only 5.02% have solely depression (CMS, 2021). There is a certain reason why the comorbidity rate demonstrates the highest percentage of Medicare beneficiaries with more than five additional conditions and the least of those who only have depression. For the most part that matches the national average, with Maryland percentages slightly lower at lesser co-morbidities.
Considering the initial disease itself, the main organ that is affected is the brain. Inevitably it influences the physical state and leads to changes in the physiological processes in the human body (Gardner, 2018). Some of the most widespread symptoms include the constant feeling of tiredness and exhaustion, low libido, problems with sleep, and lack of appetite. Although those symptoms that cause bodily reactions are significant, there is a more severe factor that can stimulate the appearance of other illnesses. The lack of serotonin usually induces multiple mental struggles, and people might lose interest in their regular activities, job, and relationship and even start experiencing suicidal thoughts and intentions.
Along with the frustration, the difficulty or inability to find a way from the condition might push an individual towards self-destructive behaviors and new disorders. Due to the fact that people with depression experience physical symptoms and emotional struggles, they try to find a way to avoid it or at least minimize it as much as possible (McKenna, 2021). Consequently, a decent number of individuals become victims of addictions. Most of the time, it implies substance and alcohol use, but it may include smoking. However, it may work otherwise when people initially struggling with addiction eventually start dealing with depression. Other conditions such as diabetes, cancer, high blood pressure, chronic pain, or heart disease can lead to the development of the disorder (Gardner, 2018). It is as ell connected with the inability to cope with the mental exhaustion, draining, and physical pain.
The Difference in Prevalence Rate among Subpopulations in Maryland
Figure 3: Conditional prevalence among age groups and genders
Expectedly the prevalence rate differs between the subpopulations such as gender and age groups, race-ethnicity, income, and geographical position. For instance, the prevalence rate among women is 20%, and among men is 11%. (Data.CMS.gov., n.d.). It is seen that number of women with depression is almost twice higher than men, and there are certain reasons for this. Older women, for instance, experience mental disorders connected with menopause, which is supplemented with the gain of weight, sleeping problems, and stress. However, many of those factors are associated with pregnancy and motherhood. Severe biological and hormonal changes in women’s bodies cause mood swings and even deep frustration. Furthermore, such occurrences as miscarriages, infertility, and complications during the pregnancy may individually or cumulatively lead to depression. Motherhood as well appears to be a stressful period for women, especially in the beginning after they give birth. Change in the lifestyle, overload with parental responsibilities, and troubles in the relationships serve as primary reasons for developing the condition.
In addition, younger people and the middle-aged population group suffer from depression noticeably more often than older ones. Individuals before age 65 have a 33.45% prevalence rate, while older adults aged 65+ only have 16% (CMS, 2021.). Adolescents are at the group risk of regrading the mental disorder and suffer from it more often than adults. Puberty is a turbulent period of life for each individual, and regular mood swings can transform into depression. Although the influence of hormones on the mental state and the overall wellbeing might be troubling, it is not enough to induce the disease. Social factors are an important driving force in the appearance of the psychological issue in teenagers. Regular adolescents often experience a crisis of identity and confusion about their role in life and the future of adulthood (Mayo Clinic Staff, 2019). Additionally, family conflicts and issues in school and with peers deeply affect the already unstable position of the child and synergetically can lead to depression (Mayo Clinic Staff, 2019). Furthermore, in that case, girls are at higher risk of developing the disorder than boys since they reach the period of puberty at an earlier age.
The prevalence rate among the different races and ethnicity varies and shows other numbers in the statistics of Medicare beneficiaries. White people struggling with depression make 19%, while the black population – 14%, Hispanic – 13%, and Asian/pacific islanders – 9%. In general, ethnic minorities are at risk factor of struggling with mental illnesses and depression in particular (Data.CMS.gov., n.d.). Due to social inequality and discrimination, they are exposed to financial struggles, poor education, and fewer opportunities for quality healthcare (Remington et al., 2016, p. 20). Still, the central problem is that racial minorities regularly have to deal with untreated depression. Although the white population more often struggles with major depressive disorder, African Americans, for instance, are exposed to chronic depression (Bailey et al., 2019). Usually, specialists fail to notice the signs of the condition, and eventually, it remains untreated (Bailey et al., 2019). Overall, this is a result of the structural inequality and inability to prioritize psychological struggles due to other difficulties such as unemployment, low salary, and adaptation to the surrounding environment.
Although ethnical minorities are a risk group, they are not the only ones who are affected by the factors mentioned above. Those who do not have an education or job and live in poverty far more often suffer from depression (Remington et al., 2016, p. 869). Individuals who live in dysfunctional areas are more likely to be exposed to severe psychological illnesses than those who live in safe and flourishing neighborhoods (Remington et al., 2016, p. 871). Thus, the geographical position is a significant indicator, and it relates to the urban and rural areas. However, the prevalence rate among Medicare beneficiaries in the urban and rural areas is the same and consists of 17% each per territory (CMS Chronic Conditions Public Use Data. n.d.). Nonetheless, mental disorders appear more often in urban areas rather than in rural (Remington et al., 2016, p. 869). The reason for this might be the higher pace of living and overload of activities, and daily stressful occasions.
Predisposing, Reinforcing, and Enabling Conditions
Since depression is a relatively common psychological disorder and often appears among the population, it requires serious attention. People with different characteristics and backgrounds can be exposed to the disease and should have the ability to receive an early diagnosis and intervention. Considering the particular determinants such as age, ethnicity, geographical position, and gender, some representers are a risk group. Women, adolescents, racial minorities, and urban citizens are the ones whose needs have to be most represented. Due to the barriers induced by Covid-19, the number of self-reported cases of depression increased. Covid-19 reportedly triggered a 25% increase in depression due to the pressure of multiple stress factors (World Health Organization, 2022). People felt significantly more stressed and less secure financially and emotionally due to the limitations of social connection and working possibilities. Older adults become the most vulnerable in this situation and face depression because of not accessing and maintaining their basic needs. Meanwhile, young people and women were significantly affected as well, being disproportionally at risk of suicide and self-harming behaviors or having pre-existing conditions that are linked to depression.
The depressive disorder should be examined, considering the possibility of supplementing illnesses. Some diseases such as diabetes, cancer, or substance abuse may be the factors that contribute to the appearance of the condition. Many chronic diseases act in synergy, so depression can have a compounding risk on health outcomes. In a national survey, disability was found in 51% with diabetes, but 78% with both diabetes and depression (Remington et al., 2016). The relationship between depression, as with many mental illnesses can be bidirectional, as many physiological and chronic conditions impact mental health, so does mental health impact the physiology. Depression can be seen in 40-60% of patients who have had a heart attack, while 1 in 4 people with cancer suffer from depression (Remington et al., 2016). In order to reinforce the factors that impact the appearance of the condition, it is crucial to detect specific details and set priorities. Firstly, it is necessary to consider the gender, age, and race of the person. Secondly, as supplementing factors should be viewed the income level and geographical position. Alongside it, there is a need to identify whether there are other diseases and, if so, which cause depression or vice versa.
The public health intervention program should focus on the risk groups mentioned above and consider their specifics. Since the majority are women and teenagers, it has to be safe for the female participants to share their problems and get support. In the case of working with children, the specialist has to be experienced in work, particularly with adolescents, because their condition is rather unstable due to puberty. The approach should demonstrate inclusivity and understanding of the specifics of people with different cultural backgrounds and consider it during the intervention. Moreover, the governmental policies should focus on the training of the professionals and bringing awareness to the public through educational institutions and the workplace. Finally, the program necessity has to be accessible because a decent number of depressive cases are caused by poverty and low income, so those people could be allowed easily to get help.
Conclusion and Recommendations
Overall, depression is a rather severe disorder that requires specific attention intervention. Women, adolescents, social minorities, and people with lower income are the risk groups whose needs have to be addressed in the first place. Depression may be a supplementing disease to other conditions or vice versa, it can cause different disorders. Thus, the medical specialists have to get additional training and education on detecting the symptoms of depression, among other occasions, and precisely identify what serves as the initial cause of the health problems. Such practice will ensure effective treatment and will allow the patients to recover in a shorter period of time.
However, based on the findings, the majority of the causing factors have roots in the social aspects of the population, such as poverty, pandemic, and discrimination. In order to eliminate the causes, the healthcare and social system specifically requires major changes on the macro level, and it might take a long time until the risk factors are reduced. Nevertheless, there are certain preventive methods that can be implemented to minimize the cases of depression. The government should focus on education about the issue and removing the stigma from having a conversation and turning to specialists for help. It might include special programs in schools, universities, and workplaces about the symptoms of depression and the reasons that lead to it.
References
Bailey, R. K., Mokonogho, J., & Kumar, A. (2019). Racial and ethnic differences in depression: current perspectives.Neuropsychiatric disease and treatment, 15, 603. Web.
Balasuriya, L., Quinton, J. K., Canavan, M. E., Holland, M. L., Edelman, E. J., Druss, B. G., & Ross, J. S. (2021). The association between history of depression and access to care among Medicare beneficiaries during the COVID-19 pandemic.Journal of General Internal Medicine, 36(12), 3778-3785. Web.
CMS Chronic Conditions Public Use Data. Chronic conditions prevalence, state/county 2018 [Infographic]. Web.
CMS. (2021). Medicare chronic conditions dashboard: State level [Infographic]. Web.
Data.CMS.gov. (n.d.). Mapping Medicare Disparities by Population [Infographic]. Web.
Gardner, A. (2018). 10 Medical Conditions That Are Linked to Depression. Health. Web.
Mayo Clinic Staff. (2019). Depression in women: Understanding the gender gap. Mayo Clinic. Web.
McKenna, J. (2021). How Are Depression and Substance Abuse Related? WebMD. Web.
PGCHealthZone. Depression: Medicare Population [Infographic]. Web.
Remington, P., L., Brownson, R., C., and Wegner, M., V. (2016). Chronic Disease, Epidemiology, Prevention, and Control (4th ed.). American Public Health Association.
World Health Organization. (2022). COVID-19 pandemic triggers 25% increase in prevalence of anxiety and depression worldwide. Web.