Introduction
This project will involve the use electronic health records (EHRs) among certain community physicians. Electronic health records are vital in the health care industry because they provide cost savings, improve efficiency and reduce the chances of performing life altering mistakes. Physicians achieve these benefits through error-reduction in prescriptions, tests, preventive care and procedures. This project can boost healthcare quality in the selected community, and thus heighten patient outcomes.
Needs analysis
This phase involves two principle segments: stakeholder identification and stakeholder need determination. The stakeholders to be involved in this project are as follows: physicians in the selected community, electronic health record vendors, health care providers and consumer groups.
The physicians will emanate from hospitals in the selected community, clinics, medial centers, community hospitals and physician associations. Consumer groups will involve public interest groups such as consumer foundations, universities and coalition groups. It will also involve health care providers like insurance providers (Ohseroff et al., 2007).
Their needs can be divided into three categories: improvement of preventive care through physician vigilance, identification of allergic drug prescriptions or harmful identifications, and management of chronic conditions among the patients. One can subdivide all these needs into smaller ones that start with the elimination of paper medical records.
Physicians waste a lot of time and resources in pulling charts. EHRs will reduce the number of employees needed to pull the charts and the amount of time spent in writing notes. Another need is avoidance of duplicated diagnostic tests. This will create cost savings for health service providers who must pay for inappropriate tests when no monitoring system exists. HIT implementation through EHRs will send alerts to physicians when lab tests are redundant.
This project will also deal with another need, which is to prevent the unnecessary use of radiological services. The EHR will provide a decision support system to physicians who would then minimize the use of unnecessary radiological services. This project will address the need to use cost-effective prescription drugs.
The physicians involved will get clinical decision support through the use of EHR. This information can assist them through the use of generic prompts as alternatives to branded drugs. Furthermore, the systems can provide them with alternatives on cost effective drug management or inexpensive therapies; this initiative with target outpatient settings particularly. Most health care insurers will benefit, and so will pharmaceutical companies.
Physicians will not benefit financially from that component. Physicians and nurses need to improve their productivity. They can achieve this through reduction of the time that they allocate to paper documentation. Lastly, the stakeholders need to reduce the length of stays in hospital.
This project will assist in achievement of that objective by avoidance of costly errors, reduction of the time it takes to administer drugs, and increment of the physician’s ability to perform clinical functions (Wang et al., 2003). This aspect may not benefit physicians directly but will benefit patients and healthcare service providers.
Project design
This project will start by identification of the participating community. It will probably involve a district that has enormous healthcare expenditures and inefficient healthcare services. The right community should be one that has a high number of participants getting their services from that respective enterprise.
It should also be highly committed to health care improvement through the use of electronic health records. Thereafter, the project manager and other team members will instate technical standards and choose the right vendors. Technical standard identification will involve specification of safety initiatives and quality initiatives. Systematized Nomenclature of Medicine (SNOMED) will be the standard system used to represent data.
A working group will carry out vendor selection, and they will also carry out evaluation of the system; features such as functionality, usability, security, reliability ad support capability will be the main points of focus for system assessment. The working group will carry out vendor selection through analysis of the company’s background. They will look at the vendor’s track record and whether it is financially viable.
The group will consider the product portfolio of the company in order to compare it with the project needs. The project team will check vendor software requirements for compatibility with current IT systems.
Client device support, implementation requirements and adherence to standards will be crucial in order to ascertain that the vendor remains compatible with the data extraction costs and the budgetary allocation (Bates et al., 2003). Finally, the working group will consider the vendor’s pricing in order to select the most cost effective terms.
The funding will follow the analysis of vendors and standard setting. Participants will receive funds for the project from government affiliated institutions as well as insurance service providers. It is unlikely that small hospitals and clinics will finance their own EHRs. This is because they may not realize the benefits of investments as much as insurance companies will. It is also likely that this process will require $ 50 million for successful completion.
Legal fees will take up five percent of this budget while twenty five percent will meet staff and direct overhead costs. The rest will finance the actual implementation of the EHRs. The project will involve collaborative meetings with key stakeholders in the community so as to include their inputs on the necessary standards and practices. Furthermore, the stakeholders will sign onto the project by committing to the full conversion of their paper records to electronic health records.
They will also promise to share data in the community and maintain data security standards. The working group will provide the participants with funding after signing the draft. After completion of this aspect, the project team will start recruiting physicians and provide patients with the options of including themselves in the project.
The project vendors will instate IT infrastructure in all the participating health institutions. After approximately four months, the system will ‘go live’. The project members will carry out an evaluation of the missing components as they proceed with EHRs.
Team leadership
A board of directors will head this project; they will work hand in hand with a consumer advisory committee as well as a physician advisory committee. The second level of the project will consist of a CEO. This individual will provide leadership and overall direction to the team members. He will ensure that other leaders will carry out their activities within project limits of time and financial resources.
Underneath the CEO are the: a working group, a financial team, an office of operations, an external communications team, and a legal team. The working group team leader will manage a group of people that will take care of clinical requirements and privacy, data standards and quality measurement, legal contracting and reimbursement, pilot selection/ evaluation, and vendor selection.
The operations team leader will deal with planning, vendor management, evaluation and budgets. Members of the team will carry out each of these functions independently. The team leader is the operations officer, and he will work with senior operations executives. The team members who carry out smaller functions will report to him (Heeks, 2006).
Scope
The key deliverables for this project include the improvement of treatment methods and protocols, improvement of better patient outcomes, reduction of healthcare costs in the selected community, detection of public health diseases and increment of the surveillance of pharmaceuticals.
The selected community will limit this project; it will not be implemented in other geographical areas. Furthermore, electronic health records are the only source of health information technology in the project. Other methods such as computerized provider order entry (CPOE) will not be a prime concern in this work.
All the stakeholders involved will participate willingly; there will be no mandatory requirements for participation. The project will not end at the ‘go live’ phase. Project team members will focus on evaluation, as well. Lastly, project success highly depends on the planning and implementation accuracies. Physicians that resist these efforts after committing to the project will adversely affect its outcomes.
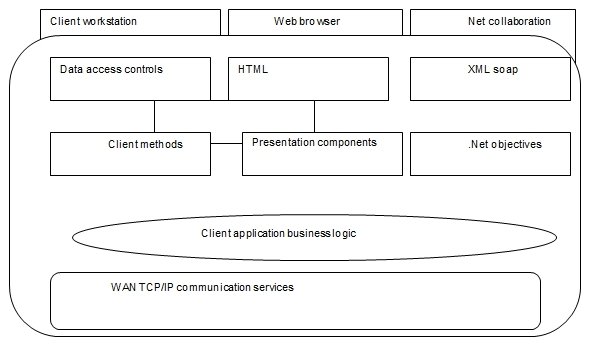
Architecture
Shown is a summary of the project architecture needed for successful implementation of electronic health records.
Conclusion
This project intends on reducing waste, improving physician efficiency and heath outcomes among the participating physicians. It will achieve this through a well-planned project and careful selection of the respective IT vendors. Stakeholders also realize that financial resources often limit physician commitment. It will solve this problem by working hand in hand with sponsoring groups.
References
Angeles, R. (2001). Creating a digital marketplace presence: lessons in extranet implementation. Internet research, 11(2), 167-184.
Bates, D., Gotlieb, E., Zapp, J., Mullins, H. & Ebell, M. (2003). A proposal for electronic medical records in primary care. American Medical Information Association Journal, 10, 1-10.
Heeks, R. (2006). Health information systems: failure, success and improvisation. International journal of Medical informatics, 75, 125-127.
Ohseroff, J., Teich, J., Steen, E., Middleton, B., Detmer, D. & Wright, A. (2007). A roadmap for national action on clinical decision support. American Medical Information Association Journal, 14, 141-145.
Wang, S., Prosser, L., Middleton, B. (2003). A cost-benefit analysis of electronic medical records in primary care. American Med. J., 114, 397-403.