Aging affects both females and males in today’s society hence the interest in factors that influence longevity. Data indicates that ordinary American men are likely to live until they reach seventy-six years, whereas the average American women live until they are eighty-one years (Murphy et al., 2018). Interestingly, if men do not face a significant injury or disease during their lifespan, they are likely to live sixty-seven healthy years. In contrast, American women are likely to enjoy healthy seventy years. All countries report that female life expectancy is slightly higher than that of men. Differences between female and male mortality rates underwent considerable changes in the 20th century (Crimmins et al., 2019). Women are highly likely to live longer than men because of behavioral and biological factors.
Behavioral Factors
Men have a high chance of abusing their bodies more than women as they are more inclined to partake in harmful habits. Both U.S. women and men have a higher life expectancy than Indian men and women. Although both behavioral and biological factors influence varying life expectancy in females and males in both nations, health outcomes in India are poorer than in the U.S. The access to medical care is lower in India than in the U.S.; therefore, people in the U.S. are likely to live longer than Indians. Men’s tendency to engage in several behaviors that risk their health can explain age differences between men and women (Reitsma et al., 2021).
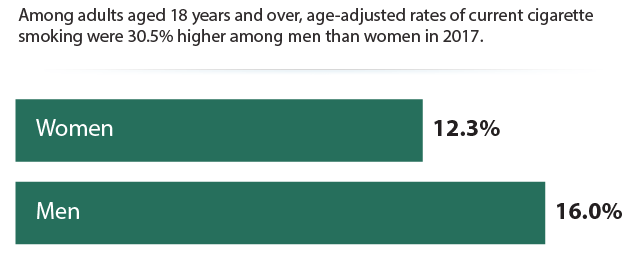
Firstly, smoking has been a critical factor in influencing men to live lesser than women (Zarulli et al., 2018). 16% of men aged eighteen and over smoke compared to 12.3% of women within the same age bracket (Healthy People, n.d.). It is generally popular among men, and the sex differences in mortality indicate that men started smoking more than women decades ago.
Smoking cigarettes elevates the risk of death by three times for smokers when compared to nonsmokers. The excess mortality among smokers is caused by smoking-related diseases, such as respiratory and vascular diseases and cancer. Smokeless tobacco increases the risk for immediate and sudden death from ventricular arrhythmias. Male smokers aggravate dying risk from emphysema and bronchitis by seventeen times and from cancer by twenty-three times. In contrast, females who smoke increase their mortality rate by twelve times from cancer, emphysema, coronary heart disease, as well as bronchitis.
Approximately 278,544 men die from cigarette smoking annually compared to 201,733 women in the U.S. (Centers for Disease Control and Prevention, n.d.). In contrast, smoking prevalence is 12.6% in men compared to 1.98% of women in India (Reitsma et al., 2021). Since more men than women smoke, it is unsurprising that smoking is responsible for the sex differences in men’s and women’s mortality rates.
Secondly, men have a higher tendency than women to eat high-fat diets that may lead to visceral fat accumulation. Such foods result from animal products and have life-threatening consequences. For example, cardiovascular disease is responsible for approximately seventy percent of the excess difference in men’s and women’s mortality. Heart diseases caused about 357,761 deaths in U.S. men in 2019 compared to 299,578 U.S. women deaths in 2017 (CDC, 2020, 2021). In addition to causing obesity, meals with high amounts of butter make men more vulnerable than women to heart diseases.
As a result of biological functions, men accumulate visceral or belly fat in their abdomen when they become overweight. Men tend to have more extensive chylomicrons, which contribute to the elevated accumulation of visceral fat in the abdomen. In contrast, fat from dietary uptakes is stored as subcutaneous fat around the buttocks, thighs, and hips in women (Covassin et al., 2018). Since visceral fat amplifies cardiovascular disease risk, more men generally develop the ailment and die early than women.
Differing Effects of Estrogen and Testosterone
The two hormones, estrogen and testosterone, affect the body and explain mortality differences between females and males. According to a recent study by Watts et al. (2021), men with elevated levels of free testosterone and the insulin-like growth factor-I hormone amplify prostate cancer danger. The research results showed that men increased prostate cancer risk by nine percent for every five nanomoles of insulin-like growth factor-I hormone in a liter of blood. In addition, each increase of fifty picomoles of free testosterone in a liter of blood led to a corresponding ten percent elevated risk of developing prostate cancer, as shown in figure 1 (Watts et al., 2021). Therefore, it is evident that the insulin-like growth factor-I hormone and testosterone jointly aggravate the risk of developing prostate cancer.

Furthermore, testosterone is an essential factor in reproduction, but it can be a double-edged sword. For instance, it helps regulate heart function and is vital in sperm production, energy levels, muscle mass, and concentration (Schooling & Zhao, 2021). As men age, testosterone is associated with reducing their lifespan. Nevertheless, testosterone is linked to adverse health outcomes as it can increase coronary plaque coagulation and volume and impair endothelial function. In addition, testosterone has been known to suppress immunity in men, which increases susceptibility to cardiovascular disease and cancers (Ruth et al., 2020). Thus, testosterone is more likely to cause an immune deficiency or dysfunction that may increase the number of men who die prematurely in older age.
While testosterone in men suppresses immune responses to diseases, estrogen has the opposite effect on female bodies. Estrogen may offer women some additional lifespan advantages. It appears to have a protective role since it acts as an antioxidant to help conserve skin collagen among women as they age. Furthermore, estrogen can prevent damage to deoxyribonucleic acid (DNA), avoiding a body that is weak and easily susceptible to various diseases. The protective effect of estrogen enables premenopausal women to have lower chances of developing coronary heart disease than women and men who have reached menopause (Iorga et al., 2017). Ultimately, estrogen helps keep the female body in a healthy and normal cell functioning.
Presence of An Extra X Chromosome in Women
Women are more robust than men since their birth due to the extra X chromosome. Men live shorter than women worldwide, whether during sickness, healthy times, wars, famine, or epidemics. In addition, researchers have determined that females outlive men in many animal species. Generally, female species have two X chromosomes, whereas male animal species have an X and Y chromosome. Researchers utilized the known fact that men living with Alzheimer’s disease die younger than women with the same illness (Davis et al., 2020). The study does not preclude the effect of environmental, social, and biological factors, but it suggests an important role that the second X chromosome in female mammals plays.
The X chromosome is associated with multiple genes related to the brain and influences survival on various levels. Without the presence of at least a single X chromosome, mammals cannot live. On the other hand, male animals and people have the Y chromosome, absent in females. The Y chromosome contains extremely few genes, except those producing secondary characteristics like facial hair and male genitals, which are not required for survival (Davis et al., 2020). The researchers used experimental mice and gave them four distinct combinations of gonads and chromosomes.
The combinations included two XX and XY chromosomal pairing found in nature and others made in the laboratory. The mice were identical in genetics, excluding their sex chromosomes. In addition, the environment was manipulated by researchers to ensure that it was the same. The final results showed that mice with two X had longer survival rates than those with one X chromosome. When the two X chromosomes were used in the ovaries, the mice’s life expectancy was longer than those with X and Y chromosomes, as shown in figure 2 (Davis et al., 2020). As a result, the existence of the second X chromosome in females improves resilience when fighting diseases. Thus, females are naturally resilient in fighting diseases, and newborn boys have a higher chance of dying than female babies.

Conclusion
In conclusion, behavioral and biological factors account for the differences in men’s and women’s life expectancies. Men are known to live shorter than women across all ages and places. Researchers have attempted to explain the sex differences in men’s and female’s mortality rates. Several reasons have emerged from researchers that explore life expectancy and sex differences in humans. Firstly, men are generally abusive of their bodies as they eat high-fat diets and smoke more than women. Secondly, estrogen, which enhances immunity in women, and testosterone, which suppresses immune responses, can explain why women live longer than men. Finally, the second X chromosome in women promotes survival and resilience. Different factors influence life expectancy, but social factors and biology have a major impact on mortality differences in women and men.
References
Centers for Disease Control and Prevention. (2020). Women and heart disease. Web.
Centers for Disease Control and Prevention. (2021). Men and heart disease. Web.
Centers for Disease Control and Prevention. (n.d.). Tobacco-related mortality. Web.
Covassin, N., Sert-Kuniyoshi, F.H., Singh, P., Romero-Corral, A., Davison, D.E., Lopez-Jimenez, F., Jensen, M.D. and Somers, V.K. (2018). Experimental weight gain increases ambulatory blood pressure in healthy subjects: Implications of visceral fat accumulation. Mayo Clinic Proceedings. 93(5), 618-626. Web.
Crimmins, E. M., Shim, H., Zhang, Y. S., & Kim, J. K. (2019). Differences between men and women in mortality and the health dimensions of the morbidity process. Clinical Chemistry, 65(1), 135-145. Web.
Davis, E.J., Broestl, L., Abdulai-Saiku, S., Worden, K., Bonham, L.W., Miñones-Moyano, E., Moreno, A.J., Wang, D., Chang, K., Williams, G. & Garay, B.I. (2020). A second X chromosome contributes to resilience in a mouse model of Alzheimer’s disease. Science Translational Medicine, 12(558), eaaz5677. Web.
Healthy People. (n.d.). Tobacco. Web.
Iorga, A., Cunningham, C. M., Moazeni, S., Ruffenach, G., Umar, S., & Eghbali, M. (2017). The protective role of estrogen and estrogen receptors in cardiovascular disease and the controversial use of estrogen therapy. Biology of Sex Differences, 8(1), 1-16. Web.
Murphy, S. L., Xu, J., Kochanek, K. D., & Arias, E. (2018). Mortality in the United States, 2017. Centers for Disease Control and Prevention. Web.
Reitsma, M. B., Flor, L. S., Mullany, E. C., Gupta, V., Hay, S. I., & Gakidou, E. (2021). Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and initiation among young people in 204 countries and territories, 1990–2019. The Lancet Public Health. 6(7), E472-E481. Web.
Ruth, K. S., Day, F. R., Tyrrell, J., Thompson, D. J., Wood, A. R., Mahajan, A., Beaumont, R.N., Wittemans, L., Martin, S., Busch, A.S. & Perry, J. R. (2020). Using human genetics to understand the disease impacts of testosterone in men and women. Nature Medicine, 26(2), 252-258. Web.
Schooling, C. M., & Zhao, J. V. (2021). Investigating the association of testosterone with survival in men and women using a Mendelian randomization study in the UK Biobank. Scientific Reports, 11(1), 1-6. Web.
Watts, E. L., Fensom, G. K., Smith Byrne, K., Perez‐Cornago, A., Allen, N. E., Knuppel, A., Gunter, M.J., Holmes, M.V., Martin, R.M., Murphy, N., & Travis, R. C. (2021). Circulating insulin‐like growth factor‐I, total and free testosterone concentrations and prostate cancer risk in 200 000 men in UK Biobank. International Journal of Cancer, 148(9), 2274-2288. Web.
Zarulli, V., Jones, J. A. B., Oksuzyan, A., Lindahl-Jacobsen, R., Christensen, K., & Vaupel, J. W. (2018). Women live longer than men even during severe famines and epidemics. Proceedings of the National Academy of Sciences, 115(4), E832-E840. Web.