Introduction
Lesbian, homosexual, bisexual, transgender, and gender-diverse individuals continue to be marginalized and excluded from health care due to discriminatory legislation and social practices. As such, this climate of exclusion fosters hatred and violence (Veldhuis, 2022). Isolation often results in an unequal allocation of healthcare resources. The voicing of concerns by stakeholders on the marginalization of LGBTI individuals and their susceptibility to poor health, particularly HIV infection, have not yet provided sustainable measures. Therefore, the healthcare system has an onus to ensure all and sundry receive ultimate healthcare.
LGBTQ Community Challenges to Accessing Sufficient Healthcare
Everyone needs access to better health care, including individuals who identify as lesbian, gay, bisexual, transgender, or queer (LGBTQ). Since sexual and reproductive health care and LGBTQ medical issues entail people’s liberty in some of their most personal choices, they are intimately intertwined. Due to significant gaps in lower health results than the general public, the LGBTQ minority has traditionally and mostly been neglected by the health care system. These disparities are caused by several obstacles in the healthcare system, such as the dispersion of medical services, prejudice on the part of healthcare professionals, and insurance-related problems.
Challenges Facing LGBTQ In Healthcare
Fragmented Health Care System
The health care system has consistently and continues to fail LGBTQ persons, with LGBTQ individuals enduring medical inequalities throughout their lifespan due to diverse and often compounding hurdles to getting proper treatment. For example, the absence of connectivity in healthcare and services for LGBTQ individuals is often isolated from sexual and reproductive health care owing to structural and financing barriers and damaging heteronormative attitudes. Such is the assumption that lesbians do not need contraception. As a reason, LGBTQ individuals often do not get complete health services.
Discrimination and Lack of Cultural Competency
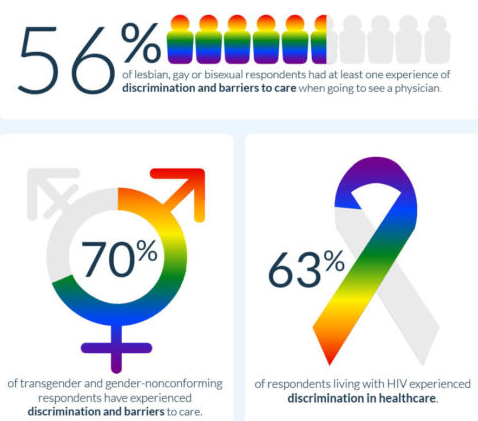
Most gay and transgender people allege anti-LGBTQ prejudice in health care. Nearly a quarter of transgender individuals have avoided obtaining health care for fear of mistreatment. This is due to health care problems with cultural competence. Thus, the system is attempting to improve providing treatment to patients with various values, perspectives, and habits. However, many health care professionals have excellent intent but possess inadequate cultural competence and education to appropriately meet LGBTQ patients’ concerns and help them experience comfort. LGBTQ people often report negative sexual and reproductive health care encounters. Moreover, contraceptive counseling is typically based on beliefs about a patient’s sexual activity, and the non-contraceptive advantages of hormonal contraception may not be considered.
Importance of Care Coordination
Care coordination entails arranging patient-care operations and sharing data across all parties involved in a client’s care in order to provide healthier, more effective care. Consequently, coordination will stress the Patient-Centered Medical Home (PCMH) paradigm of treatment. This will help the LQBTQ community transform the fractured healthcare system into a comprehensive one. Specifically, primary care settings have been essential to health care reform initiatives to improve the effectiveness of health care treatments for all LGBTQ patients, especially those with co-occurring health social issues (Nelson et al., 2017). In addition, it lowers healthcare segmentation by emphasizing team-based treatment and coordination, resulting in improved care for LGBTQ individuals.
The purpose of coordination in medical care practice is to create safer and more effective treatment by consciously arranging patient care activities and exchanging information across all the professionals connected with a patient’s care. In this manner, it guarantees that accountability is established and that an agreement is reached on duty. Primarily, the hospital shall be held accountable for damages if a member of the LGBTQ community experiences discrimination while attempting to obtain universal health care. In addition, the professionals working in the hospital will be blamed in case of discrimination.
Care Coordination in Meeting Demands
As a result of their work, their education, and the reputation they have gained, medics are well to promote and lead transformational reforms in healthcare. To play a significant role in creating these changes, nurses must comprehend the factors that motivate the change, the requirements for practice change, and the competencies in expertise, abilities, and mindsets necessary for personal and system-wide success (Salmond & Echevarria, 2017). As patient-oriented professionals, nurses are thus perfectly suited for this function. For example, medical practitioners have begun to adopt a treatment strategy that is integrative. This model enables health caregivers to assume liability for all patients.
The coordination paradigm eliminates care that is provided in a disconnected manner in medical entities. Disjointed systems are possible even within a single healthcare organization for LGBTQ members. It is uncommon for procedures to change, often drastically, from one part of an organization to another. Thus, this is particularly true when comparing primary care facilities to specialist care facilities. The coordination of care has the potential to minimize these distinctions and create the impression of a more continuous journey. This implies that the patient’s requirements and preferences are understood and conveyed at the proper time.
Inclusivity in Improving Health Standards
Since patient populations are varied, medical treatment must consider each patient’s unique history and life experiences. Nevertheless, diversity in healthcare improves staff morale by ensuring, for example, that caregivers are more sympathetic. Therefore, prejudice, stereotyping, and judgment of others may be eradicated, improving health standards. Thus, acknowledging the life choices of others may help people be more empathic and inclusive. Empiric healthcare providers deliver superior treatment by establishing a rapport with their patients, ensuring their comfort, and alleviating their anxieties and anxiety. Healthcare worker, caring for others is an enormous source of inspiration. It is crucial to minimize healthcare inequalities, particularly regarding access to treatment based on sexual orientation; this will equal a proper health standard.
Conclusion
To summarize, gender-affirming and family-centered treatment should be programmed to fuel the inclusivity of LGBTQ people. Therefore, nurses may implement initiatives such as workshops on equitable sexual and gender diversity prevention. In addition, this presentation underlined the need for LGBT cultural competency training for health professionals to ensure human rights are preserved. Thus, lesbian, gay, bisexual, and transgender (LGBT) individuals face health inequities and a lack of medication availability. In turn, the influence of these elements will increase the quality of medications.
References
Bradley, E. H. (2020). Diversity, inclusive leadership, and health outcomes. International Journal of Health Policy and Management.
Medina-Martínez, J., Saus-Ortega, C., Sánchez-Lorente, M. M., Sosa-Palanca, E. M., García-Martínez, P., & Mármol-López, M. I. (2021). Health inequities in LGBT people and nursing interventions to reduce them: A stematic review. International Journal of Environmental Research and Public Health, 18(22), 11801.
Nelson, K., Sylling, P. W., Taylor, L., Rose, D., Mori, A., & Fihn, S. D. (2017). Clinical quality and the patient-centered medical home. JAMA Internal Medicine, 177(7), 1042.
Salmond, S. W., & Echevarria, M. (2017). Healthcare transformation and changing roles for nursing. Orthopaedic Nursing, 36(1), 12–25.
Veldhuis, C. B. (2022). Doubly marginalized: Addressing the minority stressors experienced by LGBTQ+ researchers who do LGBTQ+ research.Health Education & Behavior, 10901981221116795. Web.