Abstract
Psychological disorders are the most widespread causes of the suicides among the military personnel who return from the war. Surveys and psychological questionnaires after the military personnel returned from the war can be very helpful in determining the type of disorder. Usually, military people suffer from post-traumatic stress disorder (PTSD), depression, anxiety, and bipolar disorder. The paper is aimed at testing the following hypothesis: to prove that intervention methods help lower suicide rates in the military.
Cognitive Behavior Therapy (CBT), psychotherapy counseling, Eye Movement and Desensitization and Reprocessing (EMDR), and Selective Serotonin Reuptake Inhibitors (SSRI) can be used to treat the disorders. Families should participate in the intervention programs to understand the approaches to the existing problems their family members have. The results showed a positive response to the treatments.
Introduction
In the United States, military men and women have a high rate of suicide. In the Army alone, the rate is 7.3 per 100,000 (Bagley, Munjas, & Shekelle, 2010). It is very important for all citizens to offer support, especially for those in the healthcare arena. The sacrifices made by these men and women are great, for this reason, creating a plan of care focused on the prevention of suicide is so important to the military personnel and his/her families. Gone are the days when military men and women were not welcomed home, ostracized, or worse. The awareness of what these individuals have gone through increased over the years and with that, great respect and gratitude. Therefore, our hypothesis is to prove that intervention methods will help lower suicide rates in the military.
Critical Literature Review
Throughout the years, there have been studies on the rate of suicide in the military caused by posttraumatic stress disorder (PTSD), depression, anxiety, and bipolar disorder. Studies performed such as survey and psychological questionnaire after the military personnel returned from the war have been helpful to distinguish the type of disorder (Gordana & Milivoje, 2007; Crawford et al., 2015; Blow et al., 2012).
The article I reviewed showed there were insufficient studies of United States Veterans to reach a conclusion (Bagley, Munjas, & Shekelle, 2010). The author reviewed seven different studies from previous authors to help delegate the intervention performed and results from the intervention. Some useful information that I can use from this article for my future research is the types of intervention used, such as suicide awareness training videos required during annual training, weekly counseling meeting, and mental health services (Alexander, Reger, Smolenski, & Fullerton, 2014).
I do believe the author did lack some health intervention points, such as Selective Serotonin Reuptake Inhibitors (SSRI), that can benefit the military personnel. SSRI raises the level of serotonin in your brain, which helps you feel better. This treatment involves FDA approved treatment for PTSD called Zoloft and Paxil (U.S. Department of Veterans Affairs, 2014). The available literature showed that military personnel and their families should be educated regarding the potential threats a mental disorder might pose after the return.
Materials and Methods
Study Participants
The sample of the study consisted of 300 participants: 183 men and 117 women. The age of the participants varied from 25 to 40 years of age. The participants had different ranks and experience. No exclusions were made. The condition of the participants had been evaluated during the deployment and after it. The evaluation showed that 150 men and women showed signs and symptoms of mental disorders. Only 100 participants returning from the deployment decided to enter healthcare programs designed to help the military personnel with their mental disorders.
Different Mental Disorders and Suicide in the Military
Posttraumatic stress disorder (PTSD)
It is a mental health condition caused by experiencing or seeing severe trauma. It is known as shell shock or combat stress.
Depression
It is one of the world’s top public health problems, also a cause of suicide in the military. Depression includes chronic illness, decreased function, history of neglect or abuse, family history of depression, and other psychiatric problems.
Bipolar Disorders Types I and II
Type I disorder involved periods of severe mood episodes from mania to depression. Type II is a milder form of mood elevation involving milder episodes of hypomania that alternate with periods of severe depression.
Screening and Treatment
Cognitive Behavior Therapy (CBT). The concept of this treatment method is the help of the therapist to realize the causes of the trauma and learn to control the thoughts about what may provoke stressful condition and worsen the current situation (U.S. Department of Veterans Affairs, 2014). CBT can help the military people to avoid blaming themselves in situations, for example, when their actions caused the death of their friends, and nothing could have been done about it.
Psychotherapy counseling
During the counselling treatment, participants expose their inner thoughts and negative memories to learn to control the influence of these thoughts and memories on the present state of mind (U.S. Department of Veterans Affairs, 2014). It can be helpful in the cases of soldiers having combat experiences.
Eye Movement and Desensitization and Reprocessing (EMDR)
This concept of treatment involves combined activities of CBT and tracking the movements (eyes, hands, or sounds), preliminary negotiated with the therapist who performs them (U.S. Department of Veterans Affairs, 2014; Shapiro, 2014). There is an ongoing argument about the positive influence of this treatment on the patients’ condition, but there is no evidence that it does not help.
The medication called Selective Serotonin Reuptake Inhibitors (SSRI)
Finally, this concept involved the use of specialized medications (Kauffman, 2009). It is close to the idea of antidepressant medicine. “SSRIs include citalopram (Celexa), fluoxetine (such as Prozac), paroxetine (Paxil), and sertraline (Zoloft)” (U.S. Department of Veterans Affairs, 2014). These chemicals can help a patient to relax and feel less anxious and stressed, not to mention the relief of the depression state.
Intervention Programs Designed for the Military
The intervention programs applied during deployment worked as follows. If the military personnel showed any signs or symptoms of mild bipolar or depression disorder, he/she would start psychotherapy counseling. A healthcare facility used for this military personnel to dealing with a mental disorder during deployment. Disconnecting from the combat field will help them cope and begin the treatment for their mental disorder before it becomes chronic. Intervention programs designed for the families of the military and their colleagues who need help with understanding the different mental disorders and coping with living with someone who is diagnosed with PTSD, depression, or bipolar disorder.
Results
After reviewing the 100 participants who had entered the healthcare rehabilitation facilities to help cope with their mental disorder, the rate of those who had thoughts of suicide decreased.
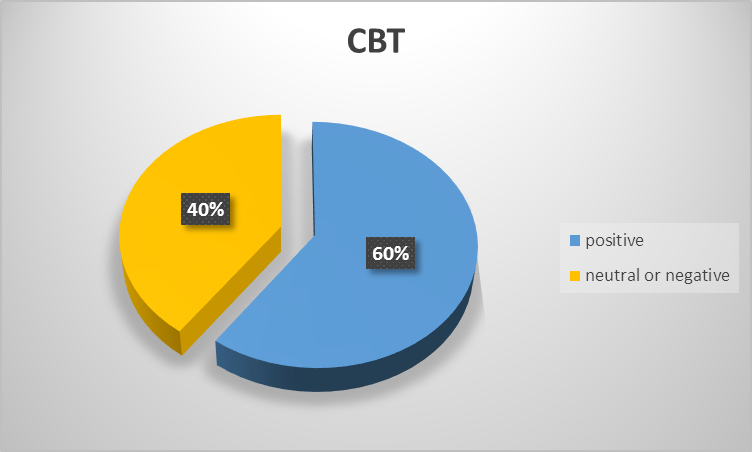
Cognitive Behavior Therapy (CBT)
The group of our 100 participants went through the CBT procedure. The results showed that about 60% of the participants responded positively to the treatment. It is peculiar that men reacted to the treatment more positively than women did (65% versus 35%). It could have been caused by the level of stress experienced by both genders and the ability to respond to it during the therapy.
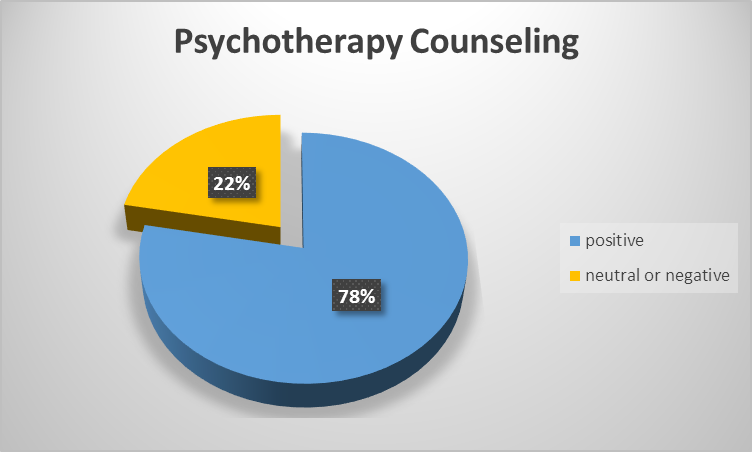
Psychotherapy Counseling
In this case, the situation appeared to be even better than in the case of CBT treatment. The results showed that almost 80% of the participants felt better after the counseling sessions. Women dominated in terms of the positive response to such type of treatment (70% versus 30%). It can be related to the less traumatic approach to the process of memory revoking since the counsellor helped the participants to get back to the traumatic events following the series of the preliminary conversations about them.
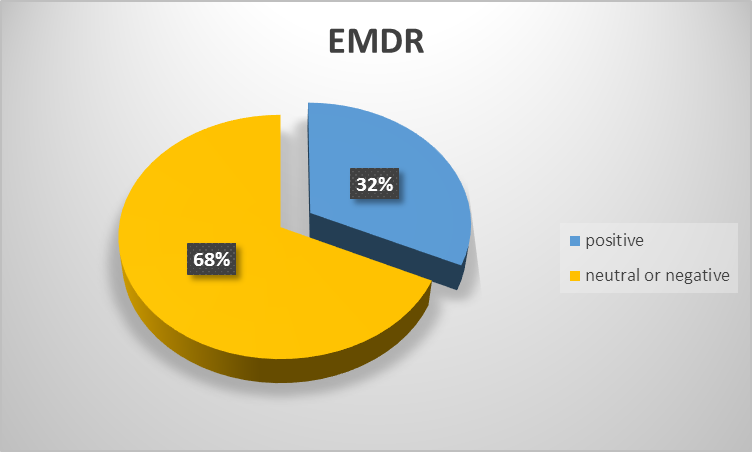
Eye Movement and Desensitization and Reprocessing (EMDR)
This type of treatment appeared to be less effective than others. In fact, only about 30% of the participants responded positively regarding their condition after the treatment course. Additionally, there was parity between men and women in this case (50% versus 50%). Such results can be conditioned by the lack of attention of the participants to the difference this treatment had as compared to CBT. It is also possible that the participants were less responsive to the therapy after the series of the previous treatments, and they did not want to revive the stressful events over and over again.
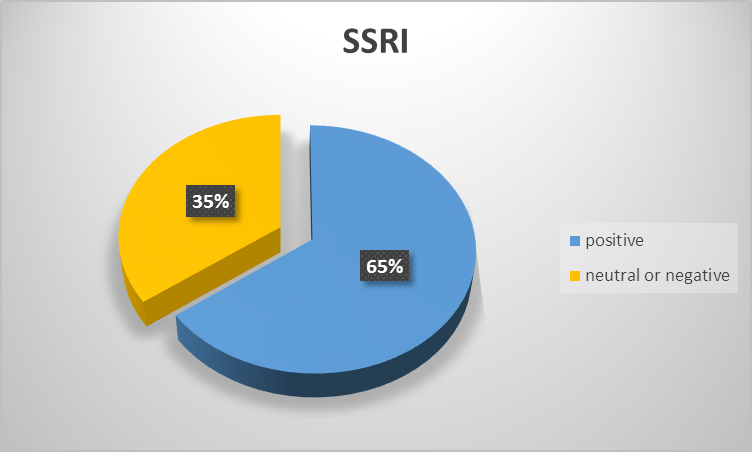
Medication Called Selective Serotonin Reuptake Inhibitors (SSRI)
Finally, the group of our 100 participants went through the SSRI treatment to finalize the experiments. The results showed that about 65% of the participants felt less depressed and anxious after the medication treatment. Men and women responded similarly (51% versus 49%).
Conclusion
After reviewing the 100 participants who entered the healthcare rehabilitation facility to help them with their mental disorder, the rate of suicidal thoughts after treatment decreased. With the intervention program designated for those in the military that showed signs and symptoms of PTSD, depression, or bipolar disorder during deployment, the turnout after treatment has been a great success. Not only does this healthcare facility help military personnel with psychotherapy counseling but it also aids their families with counseling and improves their knowledge about PTSD, depression, and bipolar disorder.
References
Alexander, C.L., Reger, M.A., Smolenski, D.J., & Fullerton, N.R. (2014). Comparing U.S. Army suicide cases to a control sample: Initial data and methodological lessons. Military Medicine, 179(10), 1062-1066. Web.
Bagley, S.C., Munjas, B., & Shekelle, P. (2010). A systematic review of suicide prevention programs for military or veterans. Suicide & Life-Threatening Behavior, 40(3), 257-265.
Blow, F.C., Bohnert, A.B., Ilgen, M.A., Ignacio, R., McCarthy, J.F., Valenstein, M.M., & Knox, K.L. (2012). Suicide mortality among patients treated by the veterans health administration from 2000 to 2007. American Journal of Public Health, 102(S1), S98-S104. Web.
Crawford, E.F., Elbogen, E.B., Wagner, H.R., Kudler, H., Calhoun, P. S., Brancu, M., & Straits-Troster, K.A. (2015). Surveying treatment preferences in U.S. Iraq-Afghanistan veterans with PTSD symptoms: A step toward veteran-centered care. Journal of Traumatic Stress, 28(2), 118-126. Web.
Gordana, D.J., & Milivoje, P. (2007). Suicide prevention program in the Army of Serbia and Montenegro. Military Medicine, 172(5), 551-555.
Kauffman, J.M. (2009). Selective serotonin reuptake inhibitor (SSRI) drugs: More risks than benefits?Journal of American Physicians and Surgeons, 14(1), 7-11. Web.
Shapiro, F. (2014). The role of Eye Movement Desensitization and Reprocessing (EMDR) therapy in medicine: Addressing the psychological and physical symptoms stemming from adverse life experiences. The Permanente Journal, 18(1), 71-77. Web.
U.S. Department of Veterans Affairs (2014). PTSD: National center for PTSD. Web.