Subgroup Presentation
The African-American subgroup represents a cohort of patients that have to cope with healthcare disparities rather often. It happens because many of them do not have adequate insurance coverage and underutilize healthcare services overall (Greene-Moton & Minkler, 2020). Thus, cultural sensitivity can be crucial for African-American patients, as it might have a positive effect on patient experiences and health outcomes. Even though African-American patients do not engage in their own healthcare too often, a culturally-sensitive approach might change that in the future.
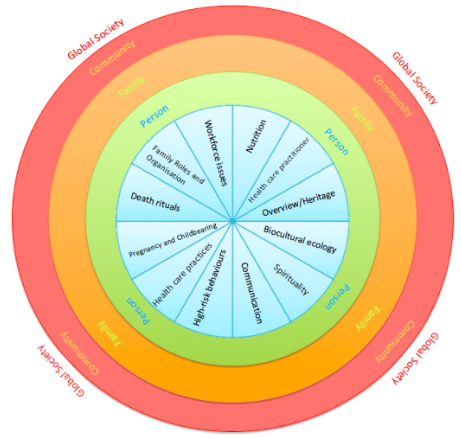
Purnell’s Model Constructs
- Overview (heritage) – a patient’s origin
- Communication – a patient’s ability to interact with others and convey health-related ideas
- Family roles and organization – in-family hierarchy and interactions
- Workforce issues – issues related to the workplace, such as a language barrier that can affect patients on many levels
- Biocultural ecology – differences between racial and cultural groups that could help patients and care providers find common grounds
- High-risk behaviors – consumption of illicit substances and other life-threatening activities
- Nutrition – food intake preferences that are specific for different cultures
- Pregnancy and childbearing – cultural beliefs that impact traditions and various practices
- Death rituals – recognition of customs and beliefs related to burial ceremonies and death
- Spirituality – prayer-related habits and cultural practices associated with religion
- Healthcare practices – provision of culturally-competent services to all patients with attention being paid to all possible cultural considerations
- Healthcare practitioner – cultural differences between providers and patients are mediated to achieve positive health outcomes.
Subgroup Issues: Local And Global
The primary local issue that has to be considered is the existence of socioeconomic disparities that might cause certain diseases to spread and create a negative health environment. According to McRoy et al. (2018), religious peculiarities and restrictions might become another cornerstone of problematic care provision. African-Americans can be expected to utilize their past experiences and religious knowledge to engage in care processes that might not necessarily be in line with the official treatment agenda. Thus, the primary global issue that African-Americans have to deal with is the lack of trust in care providers (McRoy et al., 2018). Without proper insurance coverage, African-Americans tend to live in fear and rarely address the doctors when experiencing health issues. Seeking treatment from official providers is replaced with spiritual practices and family advice, which causes even more health issues on a long-term scale. Thus, heritage, communication, and spirituality represent the biggest contributors to health outcomes in African-American patients.
Recommendations For Culturally Competent Care for the Subgroup
The primary recommendation that can be made after connecting Purnell’s model to the African-American community is to empower the latter to participate in clinical trials more often. This would improve the quality of communication and healthcare practices while also bridging the gap between patients and care providers.
The secondary recommendation is to investigate resource allocation across the most problematic African-American communities and motivate patients to contribute to the effectiveness and safety of care by providing relevant feedback. On a long-term scale, it will help care providers reduce healthcare-related anxiety and carry out more clinical research projects aimed at African-Americans.
References
Greene-Moton, E., & Minkler, M. (2020). Cultural competence or cultural humility? Moving beyond the debate. Health Promotion Practice, 21(1), 142-145.
McRoy, R. G., Oglesby, Z., & Grape, H. (2018). Achieving same-race adoptive placements for African American children: Culturally sensitive practice approaches. In Serving African American Children (pp. 85-104). Routledge.
Purnell, L. (2019). Update: The Purnell theory and model for culturally competent health care. Journal of Transcultural Nursing, 30(2), 98-105.