Introduction
Background Information
Most patients suffering from non- small cell lung cancer (herein referred to as NSCLC) are advised to undergo surgery, especially if the ailment is in the early stages. Analysis of failure patterns in the past has indicated that when resected patients suffer systemic failure, they usually become incurable. Many studies have been carried out in the field of local regional recurrence. These studies reveal that this recurrence ranges from 3 to 9 percent in stage I, and between 29 and 38 percent in Stage IIIA, depending on whether the patients were taken through adjuvant treatment. After administering curative resection, 5 year survival can range from 10 to 21 percent among persons suffering from stage III adenocarcinoma, or between 54 and 84 percent for stage I of squamous cell carcinoma (herein referred to as SCC).
There are more cases of documented distant treatment failures after surgery than intrathoracic ones. Persons who suffer from intrathoracic recurrence are mainly treated with endobronchial irradiation, completion pneumonectomy, and such other aggressive approaches. Photodynamic therapy has also been shown to be quite ineffective among NSCLC patients suffering from inoperable recurrent non- small cell lung cancer at stump site. According to a study that was conducted by Lam, 75 percent of patients who had suffered from NSCLC recurrence at stump site re-recurred after going through photodynamic therapy, in spite of initial positive response.
However, other studies conducted in this field have more than contradicted this position. There are various studies which have shown that radiation therapy can be effective in treating lung cancer stump recurrence, even when it is not used in conjunction with other therapies. All these studies were carried out over a long period of time and involved recurrence at various sites, including at bronchial stump, chest wall, and lymph node. These studies used diverse samples of patients that were treated using different doses and fractionation patterns. Additionally, radiotherapy was at times used in combination with brachytherapy or chemotherapy. In this regard, the studies did not portray a comprehensive picture on the effectiveness of radiotherapy in disease treatment. This is regardless of the fact that some of them acknowledged the fact that External Beam Radiation Therapy (herein referred to as EBRT) was as effective as surgery.
In NSCLC, pneumonectomy is required in the removal of lesions, which involves the bronchi. In the case of lung cancer, pneumonectomy is correlated to significant mortality and morbidity rates, including lung edema, postpneumonectomy syndrome, and bronchopleural fistula. However, in most cases, this cannot be avoided due to technical and anatomical considerations. In addition to changing pulmonary hemodynamics, pneumonectomy results in the migration of large vessels, as well as the heart, in the pneumonectomic cavity. This process takes place over a period of many years after one undergoes resection. After a patient undergoes right pneumonectomy, the heart will shift laterally. However, it is noted that in the case of left-sided pneumonectomy, the heart rotates in the cavity.
There are various benefits associated with radiation therapy. For example, radiation therapy improves both overall survival and local control in stump recurrence after pneumonectomy is carried out. However, the survival merits that result from secondary metastases prevention and better local control can be offset by radiation induced heart disease. There are various explanations for this. One of them is the lateral shift of the heart after the patient suffering from lung cancer has undergone right pneumonectomy. There are other ailments that a person may suffer from later in life as a consequence of cardiac irradiation. These include valvular disease, cardiomyopathy, and pericardial disease. Lung cancer patients who are also afflicted by different heart ailments have an increased risk of myocardial infarction or even death as compared to those patients without additional heart conditions. There are many contributing factors in this case. However, the main ones are cardiac volume and radiation dose.
In this study, it is supposed that cancer- heart geometry that is caused by the lateral shift of the heart serves an important role. It helps in predicting cardiac morbidity among patients with cardiac anatomy that is unfavorable for three dimension techniques. Tomotherapy has been found to significantly reduce the radiation dose delivered to the cardiac region and other uninvolved tissues among patients with left sided breast cancer. The main objective in such a case is to ascertain the effectiveness of tomotherapy in increasing the tumor dose, while at the same time reducing irradiation of the heart, the left lung and other tissues. This is among patients who suffer from inoperable recurrent non- small cell lung cancer at stump site after right pneumonectomy.
In this study, the researcher sought to analyze the preliminary results of tomotherapy for the treatment of inoperable recurrent non- small cell lung cancer at stump site. The analysis was carried out at stump site after right pneumonectomy. The treatment was carried out by escalating radiation dose and reducing radiation exposure to the right- shifted heart and to the only one remnant left normal lung caused by right pneumonectomy.
Problem Statement
Lung cancer is considered to be the leading cause of cancer related deaths in the world today. The discussion about NSCLC recurrence after pneumonectomy has been rather peripheral. The literature on the effectiveness of using radiation therapy alone in treating recurrent lung cancer among patients who have undergone right pneumonectomy is even scarcer. The scarcity is the reason why a uniform policy has not been put in place to tackle these issues in the world today. Many of the reports include studies that were carried out over periods of many years and involve multiple therapeutic and diagnostic approaches. Moreover, it is to be noted that most of the studies do not have information on treatment and expected outcomes among patients who have stump recurrences.
One of the main reasons why the survival rate among recurrence patients is low, even after subsequent radiation therapy, is that post- operative irradiation is delayed. In most cases, it is delayed until such a time when recurrence has already occurred. Various studies have pointed out that post- operative irradiation is effective, especially if it is directed and confined to stump site. In spite of the fact that this clinical investigation only involved 23 patients, it was carried out over a relatively shorter period of time. It was carried out for one year and endeavored to ascertain the effectiveness of tomotherapy as a sole treatment.
Objectives of the Study
The current study had two major objectives, which acted as guides in conducting the research. They were related to the research questions, and they represented the goals that the researcher wished to attain in conducting the study. The objectives are listed below:
Objective 1
To determine the effectiveness of tomotherapy in radiation dose escalation for the treatment of inoperable recurrent non-small cell lung cancer at stump site after right pneumonectomy
Objective 2
To determine the effectiveness of tomotherapy in reducing radiation exposure to the right- shifted heart and to the only one remnant left normal lung for the treatment of inoperable recurrent non- small cell lung cancer at stump site after right pneumonectomy
Research Questions
As already indicated, the research objectives were related to the research questions. By answering the research questions, the researcher effectively addressed the objectives of the study. Just like in the case of the research objectives, there were two research questions for this study. The questions were linked to each of the research objectives. They are listed below:
Research Question 1
How effective is tomotherapy in radiation dose escalation for the treatment of inoperable recurrent non- small cell lung cancer at stump site after right pneumonectomy?
Research Question 2
How effective is tomotherapy in reducing radiation exposure to the right- shifted heart and to the only one remnant left normal lung for the treatment of inoperable recurrent non- small cell lung cancer at stump site after right pneumonectomy?
Significance of the Study
The current study had both professional (including academic) significance and personal significance. Professional significance touches on the applicability and relevance of the current study to the researcher’s professional life, including their field of study and future, as well as current, career path. Personal significance implies the applicability and significance of the current study to the researcher’s personal life, including their background.
Scholars have noted that pneumonectomy can cure NSCLC because it is a relatively safe procedure. However, when compared to sublobar or lobar resection, it has high mortality and morbidity rates. Various scholars are of the opinion that the operation scale, as opposed to neoadjuvant therapy, is the main contributor to postoperative mortality and morbidity rates. Additionally, most patients suffering from lung cancer develop recurrence after successful resection. The recurrence can either be distant metastasis or locoregional recurrence. Between 10 and 35 percent of NSCLC patients develop isolated recurrence, while more than 50 percent of such patients develop both distant metastasis and locoregional recurrence.
As already mentioned earlier in this paper, there are quite a number of studies that have documented findings in this regard. The findings from the current study will be seminal in informing policy with regard to effective treatment of inoperable recurrent NSCLC among patients who have undergone surgery. The effective treatment is both in tumor dose escalation, as well as cardiac and pulmonary dose reduction. Penagaricano and colleagues note that tomotherapy is a radiation therapy technique that allows for conformal distribution of the dose to the volume that is targeted while at the same time reducing irradiation of normal tissues. In this regard, it is a technique that can reduce the toxicity of normal tissue and allow the escalation of the dose to the targeted volume, thus culminating in higher local control rates. The findings of the current study will go a long way in complementing such studies in the field.
Presently, there are no conclusive guidelines on the optimal dose for the treatment of inoperable NSCLC. Lack of such conclusive guidelines is especially notable in cases of bronchogenic carcinoma. It has also been observed that local control improves with an increase in the dose of radiation. Nevertheless, the optimal dose has been traditionally set from 60 to 70 Gy mainly because of the nearness of other structures to tumors. Moreover, the risk of developing radiation pneumonitis increases with the increase in the dose of radiation. The paper describes the outcomes and characteristics of 23 patients with bronchial stump recurrence after curative right pneumonectomy who received subsequent tomotherapy treatment.
This researcher is a practicing radiation oncologist from South Korea. As such, radiation and oncology is their area of specialization. The current study addresses these professional aspects of the researcher given that it is conducted within their area of specialization. The 23 patients whose data was used in the study represent a sample of the patients that the researcher comes across in their daily professional endeavors.
Assumptions Made in the Study
It should be noted that it is not possible for the researcher in a given study to control all the variables involved. The limitation can be attributed to the fact that resources may be limited, and controlling all the variables becomes hard. Efforts to control all the variables may also water down the findings of the study by negatively affecting the focus of the researcher. As a result of this, the researcher assumes that some of the factors, which they are unable to control in the study, will remain constant throughout the study. If the factors change, the researcher will assume that such changes are minimal and insignificant, and as such unlikely to affect the findings of the current study. The current study was no exception. The researcher made several assumptions, which are listed below:
- The researcher assumed that inoperable recurrent non-small cell lung cancer at stump site after right pneumonectomy is an important cause of morbidity and mortality
- The researcher assumed that tomotherapy is a technique that can be effectively used to increase tumor dose while reducing the irradiation of other normal tissues and structures
- It was assumed that the findings of this study could be applied to a universal population, beyond the 23 patients who were studied. In other words, the researcher assumed that the 23 patients shared the same experiences with others suffering from a similar condition in other parts of the world
- It was assumed that although right pneumonectomy is curable, radiation therapy is essential for the treatment of locoregional recurrence.
- It was assumed that tomotherapy is more effective than other radiation therapy methods that are commonly used in treating recurrent NSCLC.
Limitations and Scope of the Study
It is not possible to address all issues surround a given topic in a single study. The inability is due to various factors that constrict the nature of the study. As such, the researcher finds it important to leave out some issues that may be related to the study. Such a step is important in order to help the researcher focus their attention to a specific field. The boundary within which the study is to be conducted is referred to as the scope of the study. The ‘limitations’ is an acknowledgement of the issues that the research, for one reason or the other, will be unable to tackle. The scope and limitations of the current study are outlined below:
- The study limits itself to the use of tomotherapy in spite of the fact that there are other methods used in treating inoperable recurrent non- small cell lung cancer at stump site after right pneumonectomy
- In the process of collecting data for the current study, the patients received a low dose of 2.3Gy in 30 fractions in spite of the fact that clinical trials have found that higher doses lead to higher survival rates among NSCLC patients. In other words, the study was limited to the use of low doses of 2.3Gy in 30 fractions.
- The study was conducted over a period of two years. It fails to capture the long- term (five years and beyond) overall survival rate of patients. The study is thus limited to the developments among patients within these two years.
- The study involved only 23 patients and as such, trends of statistical significance may not be very clear.
- The study was carried out within the Department of Radiation Oncology, Soonchunhyang University Bucheon Hospital, South Korea. What this means is that the findings may not be representative of the whole universe.
- Although tomotherapy minimized the irradiation of the left normal lung and the heart, it was not possible to completely eliminate exposure. This was another limitation for the current study.
Chapter Summary
In chapter 1, the researcher sought to introduce the reader into the study that was conducted and reported in this article. The aim of this was to give the reader an idea of what the study was all about. Several issues concerning the study were highlighted. The researcher started by providing background information on the study, which sought to provide the reader with an idea on the field within which the study was conducted. A statement of the problem was provided. The statement sought to justify the need for the current study within the field. Objectives or aims of the study were provided. Two objectives which will guide the study were identified.
The research questions were related to the two objectives. There were two research questions corresponding to each of the two research objectives. Key words that will appear conspicuously in the paper were highlighted, followed by the significance of the current study. The researcher provided both personal and professional significance of the current study. Assumptions made in the study were also analyzed. They included an analysis of the variables that were assumed to remain constant in the current study. Finally, the researcher provided the reader with an analysis of the scope and limitations of the study.
In chapter two, a critical review of literature in this field will be provided. The aim here is to provide the reader with the status of the knowledge in the field within which the study was conducted. To this end, the researcher analyzed the findings of various studies conducted in the field. The agreements and disagreements among the various scholars in the field were identified during the critical review of relevant literature.
Literature Review
Introduction
In chapter 1, the researcher introduced the reader to the current study. Several issues concerning the study were highlighted to provide the reader with an idea of what the study is all about. Issues such as the objectives of the study, the research questions, limitations and scope, as well as the significance of the study, were all highlighted. At this juncture, the reader has an idea on what to expect from the rest of the study.
In chapter 2, a critical review of the literature that exists in this field will be provided. It is noted that the findings of studies conducted in a given field are recorded and archived, forming the literature and knowledge base of the field. It is important for the researcher in a given field to familiarize themselves with the literature or knowledge stored or available in their field of interest. By doing this, the researcher can identify gaps and inconsistencies that need to be addressed in that particular field. They can use the current study to address such inconsistencies and gaps. Literature review is also important as it helps the researcher to locate the current study within the larger field within which it is being conducted.
They are able to relate the knowledge existing in the field with the aims and objectives of their current study. A critical literature review also helps in identifying what other scholars have done in the past within that particular field. It is by doing this that the researcher can avoid duplicating what other scholars have done in the past. If it is necessary to duplicate past studies, literature review can help in arming the researcher with information regarding the findings of the previous scholars, their methodologies and limitations among other such issues.
It is also through a critical literature review that the researcher can identify the agreements and disagreements between the various scholars. The researcher can then analyze these disagreements and agreements critically and come down in favor of one or the other. These are some of the issues that motivated the researcher to conduct a literature review for the current study.
Medically Inoperable NSCLC
Overview
Surgery is the choice treatment for persons who are suffering from the early stages (I & II) of NSCLC. Nonetheless, there are many other conditions that can lead to complications or death when a patient suffering from NSCLC is operated on. To this end, it is noted that Tomotherapy has become one of the most successful surgical alternatives for treatment of inoperable NSCLC in the society today. After lung resection, health patients have a 2.5 to 5.0% complication incidence. Such incidences are not uniform or consistent to all patients. The incidence is greater among patients who have a history of suffering from lung disease. Most lung cancer patients are more likely to be smokers who engaged in the behavior at some point in their life. They are also likely to have suffered from heart disease or emphysema. After a patient is diagnosed with resectable curable NSCLC, pulmonary function tests are carried out to determine whether the person can tolerate surgery with minimal risks of complication or not. Patients afflicted by impaired pulmonary functions are likely to suffer from complications, which range from heart and respiratory failure to death.
Pulmonary function tests are crucial in such cases. They analyze the functionality of the lungs. The aim here is to determine whether these organs are capable of supplying enough oxygen to the body and rid the body of carbon dioxide. In addition, the tests determine the extent of complications likely to be suffered is the patient happens to undergone surgery. They are used to approve or disapprove treatment through surgery and to determine the patients who need further evaluation.
The findings and the results vary from one patient to the other. Steps that are taken as far as treating the patient are determined by the findings made from the tests. For example, it is important to carry out further radioactive evaluation on patients who have borderline test results. The aim here is to map out the parts of the lungs with poor ventilation capacity. It is noted that such regions of the lung have a very little impact on pulmonary function when they are resected together with the tumor.
Treatment Options
There are various treatment options available for persons suffering from medically inoperable NSCLC discussed above. Such alternatives include, among others, cryotherapy, radiofrequency ablation, and targeted therapy. Others are chemotherapy and radiation therapy. The options will be discussed in detail below:
Cryotherapy
It is one of the options available to patients afflicted with this condition. It is noted that the treatment option involves the use of liquid nitrogen. The compound is used to freeze cancerous cells. Steel probes are used in this procedure. They are inserted into the cancerous tumor and surrounding areas. The strategy is effective in delivering liquid nitrogen to the targeted areas. For persons suffering from lung cancer, the technique is used to treat the disease within the airways. The findings of one particular clinical trial conducted in Paris are significant to this form of therapy. The study found that cancerous cells were successfully eliminated among 90 percent of the patients after a year of continued treatment. Another trial conducted in Hong Kong gave similar results. The Hong Kong trial found that the rate of survival among patients treated using cryotherapy for 18 months was 86 percent. The rate is significant by any standards.
Radiation Therapy
Traditionally, 3D techniques are used to treat patients suffering from inoperable NSCLC. The 3D techniques are especially used among patients in the first two pathological stages of the condition. Scholars note that the techniques make it possible for radiation oncologists to visualize both the tumor and normal tissue in 3D. Such visualizations help the professional to calculate the dose of radiation that should be delivered to the tumor while at the same time minimizing damage to other normal tissues and organs. To this end, a dose of about 2Gy is applied to the tumor on a daily basis for a period of 30 to 35 days. At the end of the therapy, the patient is exposed to a total dose of 60 to 70 Gy. Various reviews documented the fact that the survival rate among patients treated using such an approach is 32 percent and 55 percent at 5 and 3 years respectively. Various radiation oncologists have recorded improved outcomes with the use of higher doses of between 70 and 90 Gy on the patients.
However, the benefit of delivering the increased doses must be balanced with the associated risks. A balance should be struck between the benefits and such risks as exposing other tissues, such as the spinal cord, normal lung, esophagus, and heart, to radiation. The side effects associated with the radiation depend on several factors. The factors include, among others, the dose delivered during each treatment session, total dose delivered after the entire treatment period, and the volume of tissue irradiated. Various studies have documented this fact. One such study carried out in the United States of America found that 14 percent of NSCLC patients treated with a 70 to 90 Gy dose suffered lung injury. The study found that there are various side effects associated with this form of therapy. The two most common pulmonary side effects of radiation therapy are pneumonitis, which is also referred to as lung inflammation, and fibrosis, also referred to as lung scarring.
Stereotactic Body Radiation Therapy
Stereotactic body radiation therapy (herein referred to as SBRT) is another form of treatment used on NSCLC patients. It is a radiation therapy technique that involves targeting the tumor volume with multiple radiation beams. The radiation beams are sourced from diverse directions. Each of the beams delivers low- dose radiation. A combination of all the beams gives rise to a high dose of radiation targeted at the tumor. This technique is used to deliver adequate amounts of radiation to a small tumor. At the same time, the technique minimizes the chances of irradiating normal tissues. SBRT is highly successful in treating tumors in the brain. The technique is used on lung cancer patients with medically inoperable peripheral tumors. It is also used on patients who do not want to undergo surgical procedures.
SBRT is delivered in doses of between 7 and 22 Gy. The treatment is carried out over a period of 1 to 2 weeks. The higher doses have a theoretical merit given the fact that they may damage the tumor more than the traditional 2 Gy. The technique has several advantages over other forms of treatment. It is regarded as more convenient to both the doctor and the patient given the fact that the patient is exposed to radiation for a period of 2 weeks as opposed to 7 weeks needed in other modes of treatment. However, the technique has several weaknesses. One of the biggest challenges for the oncologist using this technique is coming up with the appropriate treatment and quality control measures to optimally target the tumor and limit the irradiation of normal organs and tissues in the body.
Tomotherapy, IMRT, and 3D Techniques
In addition to NSCLC, tomotherapy, Intensity Modulated Radiation Therapy (herein referred to as IMRT), and 3D techniques, conformal radiation therapy techniques are used in treating other forms of carcinoma. As a result of the heart’s proximity to regions that are irradiated with higher doses, women who undergo whole breast radiotherapy for left- sided breast cancers are more prone to cardiac morbidity than those receiving treatment for right- sided cancers. Some studies have gone a step further to show that such patients have a high risk of mortality. Risk to myocardial infarction after radiotherapy for breast cancers is one of the complications associated with the technique. The complication is likely to occur on the left breast. It is observed to be at least three times higher than that of right sided cancers.
In spite of the fact that the accelerated partial breast irradiation (herein referred to as APBI) technique is very effective in reducing cardiac irradiation, it has several shortcomings. For example, its long term effectiveness is not well known. In addition, the technique is not suitable for women with unfavorable cardiac anatomy. IMRT techniques are used in the treatment of breast cancer through whole breast irradiation. Such a technique is used in cases where anatomic considerations determine distribution of the dose used. Moreover, when compared to standard techniques, IMRT techniques are very effective in reducing the rate of skin toxicity. Both standard IMRT applications and helical tomotherapy are widely researched on with respect to the treatment of breast cancer.
Coon and his colleagues conducted one such study in this field. Their study was a comparative analysis of the effectiveness of tomotherapy, IMRT, and 3D-CRT planning methods in reducing radiation doses on the left ventricle. The study focused on left- sided breast cancer patients. The study involved 15 women who, in addition to having left- sided breast cancer, had unfavorable cardiac anatomy. In comparison to 3D-CRT, both tomotherapy and IMRT reduced the volume of the left ventricle and the heart in general by more than 80%. The reduction was evident in areas that were exposed to more than 35Gy of radiation. However, it appeared that other normal tissues were exposed to higher doses of radiation in the case of IMRT and tomotherapy. There were significant differences between the normal tissues that were affected by tomotherapy and IMRT plans.
Many studies and randomized trials have concluded that the cardiac morbidity and mortality risk of women suffering from breast cancer varies depending on whether the patient has undergone radiotherapy or not. Such studies and randomized trials have found that the risk is higher among women who have received radiotherapy than among those who have not. As far as this development is concerned, parallels are drawn between radiotherapy and inoperable recurrent NSCLC. The variance in the risk among the different categories of women seems to be the same when it comes to inoperable recurrent NSCLC.
Some of the studies conducted in this field posit that the risk has significantly reduced with the introduction of better radiation equipment and techniques. However, other scholars argue differently. The opponents are of the view that the risk is not yet eliminated. The risks associated with the procedure are significant and cannot be downplayed. There is substantial risk among various categories of cancer patients. The categories include those cancer patients with unfavorable cardiac anatomy, those receiving biological or cardiotoxical systemic therapies, and those who are exposed to risk factors, such as smoking, diabetes and hypertension. In addition to this, there is need for long- term follow up to ascertain the efficacy of these techniques.
The Effects of Pneumonectomy
Pneumonectomy has various effects, especially among NSCLC patients. Some of these effects will be discussed in detail below:
Pneumonectomy and Parenchyma- Sparing Lung Resection (PSLR)
To assess how the outcomes of pneumonectomy affect NSCLC patients, Kawaguchi and his colleagues carried out a comparative study. The scholars compared the short term and long term outcomes among 34 primary lung cancer patients who had undergone pneumonectomy with those of 24 other patients who had undergone parenchyma sparing lung resection (herein referred to as PSLR). In the recent past, various PSLR techniques, such as angioplastic lobectomy, have become significant pneumonectomy alternatives. PSLR is commonly applied on patients with differing pulmonary functions. However, there are many cases where pneumonectomy is the only viable treatment, especially when the tumor needs to be completely removed. The viability is associated with, among others, technical and anatomical considerations. Majority of those oncologists and other practitioners advocating for PSLR base their arguments on the various limitations associated with pneumonectomy. They are of the view that as a technique, pneumonectomy is bedeviled with various demerits, such as poor quality of life (herein referred to as QOL) and postoperative complications. This notwithstanding, there are contradictions on the morbidity and mortality impacts of pneumonectomy.
Various considerations were made before subjecting the patients used in Kawaguchi and colleagues’ study to pneumonectomy procedures. In the study, patients were scheduled for pneumonectomy if the NSCLC had extensively invaded the fissure or hilum. On the other hand, PSLR was used in cases where there was need for complete removal of a lesion. 2 of the patients scheduled for pneumonectomy also had their left atrium resected. In the PSLR group, 1 patient received bronchovascular resection, 9 received angioplastic resection while 16 received bronchoplastic resection. Table 1 below shows the characteristics of the patients who were involved in the study:
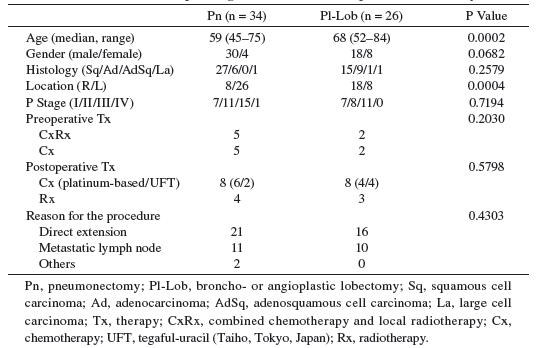
It is noted that the histology and gender characteristics of the two groups of patients used in the study were similar. In general, the study found that the disease free survival (herein referred to as DFS) among patients who had undergone pneumonectomy was 43%. The median survival time for this category of patients was found to be 22 months. The scholars also found that stage I and Stage II patients had a DFS of 73.3%, while stage III and stage IV patients had a DFS of 8.5%. There were no significant differences between the incidences of complications among the PSLR and pneumonectomy groups of patients.
1 patient who was suffering from bronchopleural fistula died while undergoing pneumonectomy. The respiratory variables of all the patients who participated in the study were comparable. However, after the operation was carried out, spirometric functions among the pneumonectomy group deteriorated significantly compared to that of the PSLR group. In addition to this, the pneumonectomy group developed exertional dyspnea after the procedure was carried out on them. Table 2 below shows that critical events (with the exception of lung cancer recurrence) occurred in 5 of the patients who underwent pneumonectomy. It also occurred in one of the patients who underwent PSLR. 4 of the 5 patients were afflicted by intercurrent disease and later died.
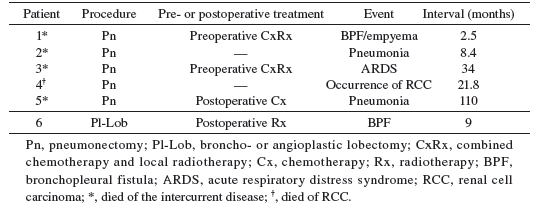
It is important to note at this juncture that surgery remains as one of the most essential strategies in the treatment of NSCLC. The extent and completeness of resection has direct physiological and oncological impacts on prognosis. Pneumonectomy is a central procedure in the treatment of NSCLC. However, it is noted that PSLR is used as an alternative for the purpose of conserving respiratory reserve. Studies have indicated that the survival rate among patients who underwent pneumonectomy and those treated using PSLR is comparable on complete removal of the tumor. However, pneumonectomy is very essential, especially to some of those patients who require complete removal of the tumor.
Kawaguchi and his colleagues found that the oncological outcomes for persons who have undergone pneumonectomy were very satisfactory. The outcomes remained satisfactory as long as the disease was in the first two pathological stages. However, most of the stage III and stage IV patients suffered recurrence early after the operation. The recurrence was recorded even after the tumor was completely removed. Such an observation concurs with the findings of other studies in the field, which have outlined that the pathological stage of the disease is crucial for survival. For the purposes of local control confirmation, pneumonectomy is an acceptable procedure. It is especially acceptable for pathological stages I and II. With respect to operative morbidity and mortality, reports indicate that the 2 variables were higher after pneumonectomy than after PSLR. However, other studies have not found significant morbidity and mortality differences between the two groups. Kawaguchi and his colleagues found that surgical mortality was comparable between the two groups of patients. The observation confirms the fact that surgical outcomes among NSCLC patients is improving with the advancement of preoperative and postoperative management procedures.
Studies conducted in this field have found that after 3 months, exertional dyspnea and respiratory function among persons who have undergone pneumonectomy are significantly impaired as compared to those who have undergone PSLR. In addition, such studies have documented the fact that there is a significant difference between pneumonectomy and lobectomy as far as exercise capacity and respiratory function recovery is concerned. For instance, the studies found that patients who underwent lobectomy lost their respiratory function early. However, the patients improved with time. It was noted that the loss of respiratory function was greater in the case of pneumonectomy. In addition, pneumonectomy patients showed no improvements with time.
In the study conducted by Kawaguchi and his colleagues, 4 patients died after undergoing pneumonectomy as a result of complications, which were not related to NSCLC. However, in the PSLR group, such deaths were not recorded. Storelli and his colleagues emphasized on the importance of monitoring non- cancer related complications after pneumonectomy. For example, studies have found that more deaths are caused by intercurrent complications among pneumonectomy patients than among lobectomy patients. However, it is important to point out that this phenomenon has not been exhaustively researched yet. Researchers suspect that the intercurrent deaths are caused by cardiopulmonary overloading.
Pneumonectomy and Sleeve Lobectomy (SL)
In recent studies, pneumonectomy is compared with sleeve lobectomy (herein referred to as SL) with regard to morbidity and late outcomes. One particular meta-analysis comparing the two procedures among stage I and stage II NSCLC patients found that SL had better outcomes in relation to mortality. However, there were no significant differences between the two procedures with regard to survival rate after 5 years. When it is technically and oncologically possible, surgeons prefer to use SL and not pneumonectomy. However, there are instances where pneumonectomy is the only option.
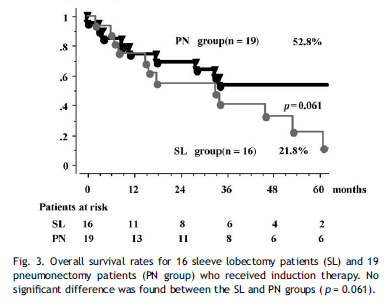
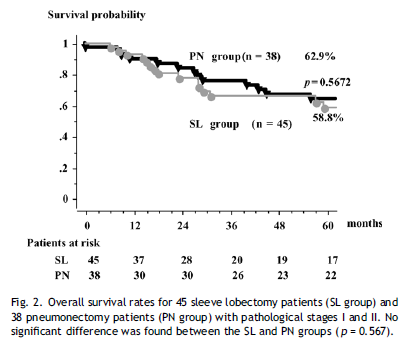
One of the most comprehensive studies comparing the two procedures was conducted by Shin-ichi and colleagues. The comparative study was conducted in Japan using data collected from 1211 patients over a period of 20 years. 3 patients in the SL group, who had undergone induction therapy, died as a result of respiratory failure (also referred to as emphysema). The patients died from serious complications. 1 patient in the pneumonectomy group, who had previously received induction chemoradiotherapy, succumbed to respiratory distress 6 days after the operation was carried out. In general, the 5 years’ rates of survival among the SL and pneumonectomy groups were 54% and 33% respectively. However, there were no significant differences in the rates of survival after 5 years for patients with stage I and stage II NSCLC in the two groups. From figure 1 below, it is obvious that the survival rate for pneumonectomy patients with stage III NSCLC, who were given induction treatment, was marginally better than that of SL patients.
Scholars note that lung cancer respectability is improving in tandem with advances in induction therapy, preoperative care, and surgical techniques. What this means is that for those patients who are in the early stages of NSCLC, it is possible to avoid pneumonectomy. Storelli et al. outlined that the SL to pneumonectomy ratio is almost 1.0. For stage I and stage II patients, SL is found to provide a better QOL and long-term rates of survival. Petrella et al. indicated that the operative mortality of SL is very low. It ranges between 1 and 7% as compared to that of pneumonectomy, which ranges between 4 and 12%. In addition, the study conducted by the scholars indicated that even among patients who had received induction therapy, SL is safer. It is also associated with fewer complications compared to those associated with pneumonectomy.
The morbidity and mortality results of SL and pneumonectomy procedures are acceptable, taking into consideration the increased number of patients undergoing induction therapy and extended resection. Shin-ichi et al. and other scholars found that the local rates of relapse are comparable for the two procedures. Shin-ichi et al. found that complete resection is the last resort when the practitioner feels that nothing else will work. Complete resection is used when nothing else will work after induction therapy on patients who have locally advanced lung cancer. Complete resection, according to the scholars, is a huge challenge for thoracic surgeons. The scholars also found that the five- year survival rate among stage I and stage II patients in the two groups was similar. In addition to this, stage III pneumonectomy patients who had undergone induction treatment reported better survival rates after five years than their SL counterparts. With regard to overall survival, morbidity, and mortality, Shin-ichi et al. did not find any drawbacks in pneumonectomy in comparison to sleeve resection. The table below is an indication of the survival probability recorded by the scholars in their study:
Pneumonectomy: Laterality and Survival
The use of pneumonectomy in the treatment of lung cancer is one of the surgical procedures for the condition, which is associated with high risks. Various studies in the field have attempted to find out the adverse outcome predictors among pneumonectomy patients. The main objective of such studies is stratification of the various risks associated with the procedure, as well as improved selection of patients to undergo the procedure. Some of the adverse outcome predictors identified by the various studies include, among others, neo- adjuvant therapy, cardiovascular disease, male sex, and age. Other studies have identified increased peri- operative risk among right pneumonectomy patients. The right pneumonectomy- induction therapy is considered to be especially morbid.
However, other studies conducted in the field have not established a link between increased peri- operative risk and literality caused by right pneumonectomy. Such a study was conducted by Fernandez et al.. The study was conducted to determine how laterality affects outcomes after the patient undergoes pneumonectomy. In addition, the scholars sought to determine how laterality interacts with radiotherapy. The study used data collected from 9746 patients sampled from the Surveillance, Epidemiology, and End Results (herein referred to as SEER) database from 1988 to 2006. The mean age of the patients was 62 years.
In addition, 56% of the patients had undergone left pneumonectomy while 44% had undergone right pneumonectomy. Pre- operative radiotherapy was administered on 7% of the patients, while 24% of the patients received postoperative radiotherapy. The patients who were taken through right pneumonectomy had various characteristics setting them apart from the rest of the sample. The patients were younger, they were diagnosed with more adenocarcinomas than squamous cell NSCLC, they received more induction radiotherapy than other form of treatment, and they had larger tumors, which were well differentiated, than those of the other patients. In addition, the patients had fewer metastatic lymph nodes as compared to the rest of the sample, and they underwent a surgical procedure that was less radical.
From their study, Fernandez et al. found that left pneumonectomies were associated with improved overall survival as compared to right pneumonectomies. As far as the mortality rate was concerned, the left pneumonectomies recorded 8 percent while the right procedures recorded 16 percent after one month. After 3 months, the mortality rate changed to 4 percent for right procedures and 9 percent for left procedures.
A review of cancer registries reveals that the risk associated with peri- operative right pneumonectomy is twice that of left pneumonectomy. When all other covariates involved in the procedures are controlled, it is clear that right pneumonectomies are important death predictors compared to the left pneumonectomies. Another comprehensive study conducted in this field found that the rate of mortality after undergoing right pneumonectomy was 10% in comparison to 1% for a left pneumonectomy. Fernandez et al. also confirmed that induction therapy increases the risk associated with pneumonectomies.
Preoperative radiotherapy, together with chemotherapy, is associated with a decrease in pulmonary function. Another study by Song et al. found that induction chemotherapy was associated with higher peri- operative mortality rates when compared to induction radiotherapy. It is important to note at this juncture that it is possible to safely perform pneumonectomies after neo- adjuvant therapy with favorable outcomes. The favorable outcomes can be achieved when there are many and highly experienced surgeons. However, the additional risks associated with the use of induction therapy have not yet been fully mapped out.
Fernandez et al. did not find any statistical significance on the impact of laterality on long- term survival among the patients. The findings were supported by those made in another study by Kappers et al. Kappers et al. did not find any relationship between pneumonectomy laterality and 5-year survival rate among the patients used. From these studies, it can be concluded that the rate of early mortality is high among patients who receive right pneumonectomy compared to those who undergo left pneumonectomy. Before administering a pneumonectomy, it is important for the surgeons to take into consideration the traits of individual patients. The considerations should be made with regard to the use of induction therapy, pulmonary function, comorbidities, laterality, and age.
Pneumonectomy and Neo- Adjuvant Chemoradiation Therapy
In their study, Kim et al. notes that over time, pneumonectomy has emerged as a relatively safe surgical procedure. Some investigators in the field are of the opinion that when it comes to survival after pneumonectomy, what determines postoperative mortality and morbidity is scale of operation. The mortality and morbidity rates are not determined by the use of neo- adjuvant therapy. In their study, Rea et al. noted that at times, right pneumonectomy may not give rise to expected curative outcomes among the patients. Such an observation is made especially if patients are dealing with complexities associated with other therapies, such as chemotherapy and radiotherapy. As a result of this, many clinicians have pointed out that right pneumonectomy should not be administered on patients after they have received chemoradiation.
The question of whether there are any long- term benefits associated with right pneumonectomy offered after the administration of neoadjuvant chemoradiation remains very controversial. Kim et al. sought to address this controversy in their study. The scholars conducted a study to find out the long- term survival and peri- operative risks associated with pneumonectomy after chemoradiation therapy among NSCLC patients. The researchers reviewed records of all NSCLC patients who had undergone pneumonectomy and subsequent chemoradiation treatment between 1983 and 2007. The patients participating in the study were diagnosed with locally advanced NSCLC.
The condition called for the administration of neoadjuvant treatment. The technique was aimed at attaining complete resection. In addition, the patients had completed radiation and chemotherapy concurrently. They had also undergone pneumonectomy after completing neoadjuvant therapy. Kim and his colleagues recorded various variables in the study. The variables included gender, age, and regimen of chemoradiation. Others were histopathology, 90- day mortality, survival, and major complications. Table 3 below is an illustration of the major complications associated with pneumonectomy after receiving neoadjuvant chemoradiation.
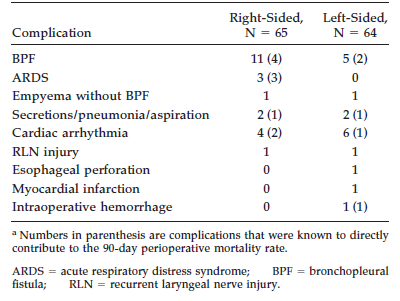
In all the regimens used in the study, the patients received chemotherapy together with split- course radiation therapy. Platinum- based regimens were used in administering chemotherapy. By 1994, the treatment included two main drugs. The drugs were 5- fluorouracil and cisplatin. Afterwards, etoposide was included in the regimen. In 1995, the treatment formula was adjusted to include three drugs. The three were paclitaxel, carboplatin, and etoposide. The latter was later eliminated as the study progressed. The mean radiation used in the course of treatment was 43Gy. Right and left pneumonectomies were conducted without any form of discrimination. The researchers did not discriminate against those patients in need of intrapericardial dissection. It is important to note at this juncture that the scope of the study by these scholars was limited. For example, the study did not include carinal pneumonectomies and those performed for malignancies, such as metastatic disease, neuroendocrine cancers, and mesothelioma.
The total number of pneumonectomies conducted was 129. Out of this, 64 were left pneumonectomies, while the other 65 were right pneumonectomies. The mean age of the patients used in the study was 57 years. The number of men in the sample was 79 and that of women 50. The histological distribution among the patients participating in the study was varied. It included 77 squamous carcinoma, 44 adenocarcinoma, 5 large cells, and 1 carcinosarcoma. In total, 43 patients had complications. The complications reported included, among others, bronchopleural fistula, acute respiratory distress syndrome, cardiac arrhythmias, empyema, pneumonia that required bronchoscopic intervention, myocardial infarction, laryngeal nerve injury, intraoperative hemorrhage, and esophageal injury. 19 patients had died 90 days after pneumonectomy was conducted.
The mortality rate within 90 days stood at 20% for right pneumonectomy procedure and 9% for left pneumonectomy procedure. The differences between the outcomes of the two procedures were not statistically significant given the fact that the p value used by the researchers in this study was 0.089. According to figure 3 below, the overall survival rate among the patients after five years was 33 percent.
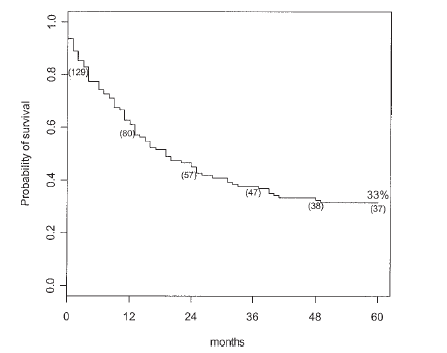
The five- year survival rate for the patients who had undergone right pneumonectomy was 32%, while that of the patients who had undergone left pneumonectomy was 34 percent. The difference was not statistically significant. In addition, the researchers conducted a univariate analysis to find out the five- year survival determinants. The results of this univariate analysis are presented in Table 4 below.
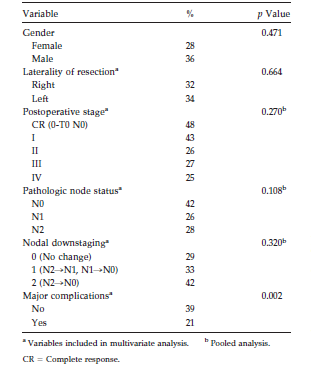
In addition to this, the researchers analyzed the five- year rate of survival with respect to postoperative stages. The survival rate was 47%, which included I-44%, II-25% III-25%, and IV-24%. Although the intergroup difference was not statistically significant, the p value of the first two stages, which are CR and I, was closer to the significant value than that of the others. The scholars also determined five- year survival rate with regard to N status. The respective findings were: N0- 43%, N1- 27%, and N2- 26%. In spite of the fact that Kim and colleagues used a relatively small sample size, the differences between N0 and N1 on the one hand and N0 and N2 on the other hand were close to the level of significance (p < 0.0558 & p < 0.0978). Out of the fifty four patients with N2 disease, 34 had a right- sided pneumonectomy procedure, while 20 were taken through a left pneumonectomy procedure. After five years, 7 patients out of the 34 were alive compared to 6 out of 20 for the other procedure.
Sixty one patients used in the study had tumor down- staging. Kim et al. found that there a positive correlation between the degree of down- staging degree and five- year survival rate. Specific evaluation of nodal down- staging revealed that there was a 43% N2- N0 down- staging and 33% N2- N1 or N1- N0. In addition, the scholars found that there was no change in N1 or N2 status in 29% of the patients. Again, probably because of the small sample size (although there were obvious trends), the differences were not statistically significant.
Kim et al. stratified the five- year rate of survival depending on whether the patients developed complications or not. The scholars found that when the patients did not develop complications, their rate of survival in five years was 39%. However, when the patients developed complications, the rate of survival in five years was reduced to 21%. The difference observed was statistically significant at p < 0.002 level of significance. When the researchers limited the complications to bronchopleural fistula and acute respiratory distress syndrome, the five- year rate of survival for the whole cohort was 17%. The decrease in the rate of survival was statistically significant in comparison to that of patients who did not develop complications (p< 0.001). When all other complications were taken into consideration, with the exception of bronchopleural fistula and acute respiratory distress syndrome, the rate of survival after five years rose to 28%. The difference between the two figures was not statistically significant when compared to patients with no complications. All the patients who suffered from acute respiratory distress syndrome died within ninety days.
When major complications, node status, postoperative stage, age, and lymph node down- staging were analyzed on a multivariate scale, there were no variables with a negative effect on the five- year rate of survival for patients who underwent left pneumonectomy. On the other hand, the development of major complications was the only variable that had a negative effect on the rate of survival among patients who underwent right pneumonectomy.
Chemoradiation is widely used as a neoadjuvant intervention in the treatment of cancer. In their study, Neuboeck et al. concluded that when chemoradiation is used before surgery in the treatment of cancer, it has a mild curative benefit. However, they found that patients who underwent pneumonectomy had a higher postoperative mortality rate as compared to patients undergoing other resections. Specifically, the researchers concluded that the number of death among right pneumonectomy patients was higher than that of left pneumonectomy patients.
Pneumonectomy is associated with a mortality rate of between 6 and 12 percent. Some studies report that the use of neoadjuvant chemoradiation increases the mortality rate of pneumonectomy patients. It is noted that even when neoadjuvant chemoradiation treatment is not administered, the mortality rate of right pneumonectomy lies between 13 and 38 percent. This notwithstanding, some scholars in this field have suggested that when neoadjuvant treatment is used, the mortality rate for right pneumonectomies reduces.
The peri- operative mortality rate recorded in the study conducted by Kim et al. was 16 percent. The researchers used a 90 day mortality rate given the fact that many of the deaths reported within the first three months are directly or indirectly traced back to the procedure. In addition to this, when the 90 and 30 days’ rates of mortality are compared, the mortality rate within 30 days is usually higher. As such, the 90 day mortality rate is more accurate as compared to the 30 day mortality rate.
The researchers found that peri- operative deaths were highly associated with the development of complications during the patients’ post- operative stay. Although the long- term rate of survival among the patients was not different with regard to laterality, there was a rather dramatic difference in their rate of mortality within 90 days. However, although Kim and colleagues conducted one of the most comprehensive studies of its kind, there is need for more studies in the field. For example, another study involving a shorter period of time and a larger sample would clearly elaborate on the statistical significance of the differences recorded.
The 30% pneumonectomy morbidity incidence, which was documented by Kim et al., was largely similar to that documented by other researchers in the field. Other researchers have sought to determine the correlation between neoadjuvant therapy and pneumonectomies. The findings made by Kim et al. emphasized on the importance of major complications in the rate of mortality among patients who have undergone pneumonectomy surgical procedures. The findings by Kim et al. concurred with those made by other scholars as far as complications and mortality rates among these patients are concerned. In addition, Kim et al. provided more information on how such complications are affected by concurrent neoadjuvant chemoradiotherapy. The study established that patients who have undergone pneumonectomy are vulnerable to bronchopleural fistula and acute respiratory distress syndrome.
Their vulnerability to these complications is significant, even in the absence of neoadjuvant treatment. Some reports have shown that there is no increase in the incidence of these two complications with regard to either right or left pneumonectomy surgical procedures. However, most clinicians have the intuitive presupposition- and others have gone ahead to demonstrate it- that right pneumonectomies are associated with a higher incidence of bronchopleural fistula compared to left pneumonectomies. Such clinicians include Pless et al.. The scholars performed a multivariate analysis, which demonstrated that there is a positive correlation between the formation of bronchopleural fistula and right pneumonectomies after patients are treated with preoperative radiation therapy.
Such observations underscore the fact that clinicians should always put in place measures to avert the disruption of the bronchial stump. Kim et al. documented that in the series, pericardial or pleural fat pads were used to buttress right- sided stumps. Although they did not conclude that this measure led to a significant reduction in the incidence of bronchopleural fistula, it is objective to posit that it was possible for the rate of incidence to increase.
The 2% rate of incidence for acute respiratory distress syndrome that was documented by Kim et al. was on the lower side in comparison to what has been reported by other scholars in the field. The incidence was lower than that reported by other scholars with respect to pneumonectomy, with or without neoadjuvant therapy. However, Kim and colleagues’ finding of 100 percent rate of mortality rate associated with acute respiratory distress syndrome in 90 days was similar to that of other researchers. It was also observed that all patients who suffered from acute respiratory distress syndrome developed the complication after right pneumonectomy. The observation supports the recommendation made by oncology experts that measures should be put in place to prevent mediastinal shifting. Measures should also be put in place to administer intravenous fluids, as well as promote aggressive respiratory toilet.
It is important to note at this juncture that the 33 percent overall rate of survival that Kim et al. reported was consistent with the survival rate documented in other studies conducted for pneumonectomies that are conducted after induction therapy. Disease down- staging was suggestive of survival in the series. Furthermore, the findings suggest that the down- staging of mediastinal lymph nodes independently influences the rate of survival. Again, this observation was consistent with those made by other investigators in the field.
Other studies have compared N0 disease with N2 disease. The studies found that the latter had a negative overall rate of survival. The researchers observed individuals affected by N2 disease. The patients observed had undergone lateral resection. The researchers found that 30 percent of the patients taken through right pneumonectomy survived five years after the operation. It was found that 21 percent of the patients taken through left pneumonectomy survived five years after the operation. Although the observation was not ideal, it suggests that it is possible to treat N2 patients using pneumonectomy.
However, due to low survival rate after five years, as well as the high postoperative rate of mortality when right pneumonectomy is used after induction chemoradiation treatment, mediastinal restaging should be used to ensure that there is no N2 persistent disease. Kim et al. suggested that right pneumonectomy should be avoided on patients with N2 disease after they have undergone therapy. The reason is that in most cases, the complications arising from the operation are fatal. It is noted that even if the patient survives the complications, the five- year rate of survival is very low.
Pneumonectomy and Heart Dislocation
According to Smulders et al., pneumonectomy procedure is likely to change the position of the heart. As a result of this dislocation, the function of the heart is affected. Smulders et al. investigated the impacts of pneumonectomy on the left ventricular function (herein referred to as LV) and right ventricular function (herein referred to as RV). In addition to this, Smulders et al. sought to investigate whether the function is affected by the laterality of pneumonectomy or the migration of the heart. The scholars gathered information from 15 patients who had survived for the past five years after undergoing pneumonectomy surgical procedure. In the study, the scholars used magnetic resonance imaging to determine the function of the LV and RV. The same was used to determine the position of the heart in the thoracic cavity.
Major resection of the lungs, like the one carried out in the case of pneumonectomy, is known to reduce the ventilator function of the heart. In addition, the resection is known to significantly affect the function of the right ventricle. After pneumonectomy, the RV undergoes dilation and its ejection fraction is significantly reduced. The resulting after- load, which is caused by increasing pressure in the pulmonary artery and resistance in the pulmonary vessels, is supposedly the main cause of the RV dysfunction experienced after pneumonectomy. It is, however, not clear to what degree the dysfunction recovers over time. It is also not clear whether the dysfunction plays a major role in limiting the exercise capacity of patients or not.
A number of years after lung resection is carried out, pulmonary hemodynamics are highly affected. In addition to this, large vessels, as well as the heart, migrate through the thorax. Fibrotic tissue is produced in the resulting pleural space, which in effect leads to changes in intra- thoracic pressure. The development has several ramifications as far as the patient is concerned. Among others, the changes lead to diaphragm elevation, lung over- distension, and shifting of the mediastinum, as well as the heart, to the operated side. Cardiac function and structure are also likely to change. The change depends on the laterality of the pneumonectomy and the position of the heart in the thorax.
In their study, Smulders et al. found that in the long term, there are various intrathoracic changes that take place after pneumonectomy. For example, there is a reduction in the stroke volume, which is compensated for by an increase in the heart rate. The compensation is an indication of a compromised cardiac functionality. In their study, they found no evidence of right ventricle hypertrophy. The lack of evidence means that it is not factually correct to attribute the decrease in stroke volume to increased pressure in the pulmonary artery. In addition to this, the scholars concluded that given the differences observed between right and left pneumonectomy patients, the under- filling of the right ventricle was the main cause of RV function compromise among right sided patients. On the other hand, the failure of the left ventricle was revealed as the main determining factor among patients who had undergone a left sided procedure. Generally, the scholars noted that the cardiac function of the patients was well preserved. Such preservations depend on the specific situations of the survivors.
There is extreme shifting of the mediastinum in cases where the post-pneumonectomy space is absolutely obliterated. MRI images reveal variations or changes in the location and amount of pleural filling with respect to the pleural filling itself and the hemidiaphragm. As a result of this, there is an expansion of the remaining lung. Smulders et al. concluded that patients who underwent right pneumonectomy did not suffer from the compression of the main bronchus on the left side.
According to Smulders et al., heart rotation occurred more on patients who had received a left sided procedure than on those who received right- sided surgical procedure. The survivors depicted huge differences with regard to heart rotation. However, it is important to note that the predictors of the degree of rotation are not quite clear. Many scholars believe that the final heart position is influenced by the variation in the shape of the thoracic cavity, ipsilateral hemidiaphragm elevation, and the extent of pleural cavity obliteration. In comparison, patients who have undergone right sided pneumonectomy experience a lateral shift and only a minor heart rotation. Several factors affect lateral shift of the heart among patients who undergo the right- sided procedure. One of the factors is the extent of pleural space obliteration.
The size of the sample used in the study by Smulders et al. was quite small. As such, it was not possible for the researchers to conclude whether there were differences on the impacts of pneumonectomy on the function of the heart between the two groups of patients. However, subtle differences were observed. First, the end-diastolic volume of the right ventricle and the mass of the left ventricle were lower among right pneumonectomy patients compared to left pneumonectomy patients. The subtle difference is as a result of the lateral shift that possibly impairs the infilling of the right ventricle, which is brought about by the compression of the thoracic wall. It is possible to use the same observation in explaining the low mass of the right ventricle among right pneumonectomy patients. The low mass of the left ventricle may result from the reduction in stroke volume on the wall of the left ventricle. In addition to this, left pneumonectomy survivors had a lower left ventricle ejection volume compared to their right pneumonectomy counterparts. Left pneumonectomy survivors also showed an increase in the end- diastolic volume of the left ventricle compared to right pneumonectomy survivors.
Smulders et al. did not establish a correlation between the ejection fraction of the left ventricle and the extent of the rotation of the heart. However, it is important to note that the failure to establish a correlation does not nullify the possibility of a causal correlation between the rotation of the heart and the loss of systolic function. It was not possible to carry out such an analysis using the available sample size of 15 survivors. The control group used by Smulders et al. in this study was composed of patients who were relatively younger compared to the pneumonectomy survivors. What this means is that there is a possibility the findings were biased. However, age as a single factor has little impact on the function and structure of the heart.
Smulders et al. did not find evidence of right ventricle hypertrophy or the dilation of the right ventricle. In this regard, pulmonary hypertension was not likely to occur among the patients in the study population. Other studies carried out to determine how pneumonectomy affects pulmonary and cardiac function have come up with varying conclusions. There are those concluding that among pneumonectomy patients, the pressure of the pulmonary artery and right ventricle systolic pressure are relatively normal at rest. However, the pressure increases during exercise given the fact that the pulmonary vascular bed has a smaller recruitment capacity. Such an observation is in agreement with the findings made by Smulders et al. in their study.
Pneumonectomy and Stage I NSCLC Survival
As mentioned earlier in this paper, surgery is the preferred form of treatment for NSCLC patients. At this first stage, the condition has a positive prognosis. The preferred mode of treatment at this stage is lobectomy. In comparison to smaller resections, pneumonectomy is associated with more operative risks and other physiologic effects. However, the procedure is inevitable at times. There are various confounding variables associated with poor survival among pneumonectomy patients. One of these variables is a higher stage of cancer. Some studies conducted in the field have found that the procedure has independent negative impacts when carried out among persons ailing from early NSCLC.
Alexiou et al. conducted a study to find out whether there was a correlation between pneumonectomy and the rate of survival among pathological stage I NSCLC patients. The sample used in the study was made up of 485 patients who were treated using various lung resection procedures. The population was divided into two groups. The first group (Group A) had 374 patients who had received smaller lung resection procedures. The second group (Group B) was made up of 111 pneumonectomy patients. A comparative analysis was carried out between the two groups based on various determinants. The determinants included, among others, demographics, histopathologic and clinical features. Others were overall rate of survival and rate of mortality associated with the surgical procedure.
Male participants were the majority in both groups, but the pneumonectomy group (group B) had significantly more men than group A. The preoperative spirometry of the patients in the two groups was relatively similar. Histopathologic examination was carried out. It showed that adenocarcinoma was main form of NSCLC in this category of patients. On the other hand, SCC was most common in the other group of patients in the study. Table 5 below summarizes the histopathologic findings made in the study:
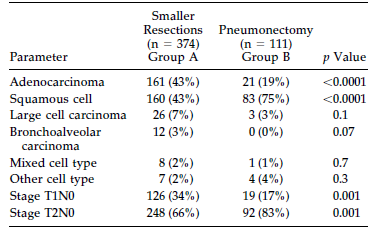
The operative mortality rate in group A was 2.4%, while that of group B was 8%. The main causes of death in the first group were pneumonia, pulmonary embolism, ventricular arrhythmias, myocardial infarctions, and peritonitis. Deaths in the pneumonectomy group were mainly caused by bronchopleural fistula, pneumonia, myocardial infarction, pulmonary embolism, adult respiratory distress syndrome (herein referred to as ARDS), and cardiorespiratory failure.
The Kaplan-Meier rates of survival for 1, 3 and 5 years were 85%, 63%, and 50% for group A and 66%, 47% and 44% for group B. The independent adverse survival predictors were pneumonectomy, older age, male gender, and T2 stage.
In comparison to similar studies carried out in this field, the number of patients who received pneumonectomy treatment in the study conducted by Alexiou et al. was quite high at 22.8%. The findings on operative rate of mortality were in agreement with those made in other studies that were carried out earlier on. Various studies have established the long- term effects of pneumonectomy on QOL and cardio- respiratory function. The studies have also shed light on the outcome predictors after the removal of a lung. However, it is important to note that the impact of pneumonectomy on overall survival is quite controversial.
In their study, Alexiou et al. found that as an independent variable, pneumonectomy led to decreased rate of survival in the study population. The significance of this observation cannot be downplayed, especially considering the fact that pneumonectomy patients were younger and had lower respiratory comorbidity prevalence than patients in group A. One may be tempted to explain away such an observation as a simple reflection of high operative mortality rate, which is associated with pneumonectomy. However, the differences in the rate of survival were evident three years after the operation. In this regard, the scholars conclude that pneumonectomy has a negative impact on the rate of survival both immediately and after the operation.
Nonetheless, it is important to note that the study conducted by Alexiou et al. had various limitations. For example, the study was limited by the fact that the scholars excluded from the study deaths that were caused by non- cancer related complications. The reason for this exclusion is that most death certificates for lung cancer patients indicate that they died of lung cancer even if they may have succumbed to a complication that is not directly linked to cancer. In this regard, there is a possibility of bias with respect to the conclusion that pneumonectomy is a predictor of poor long- term rate of survival.
Other studies conducted in the field concluded that as an independent variable, pneumonectomy is associated with poor rate of survival among stage I and II NSCLC patients. Thomas et al. carried out a similar study, which used data collected from 515 patients suffering from NSCLC. Out of the 515 patients in the sample, 81 had received a pneumonectomy. The rate of recurrence between the group of patients who had received pneumonectomy and those who had received smaller resections was fairly similar. However, the rate of survival (both short- term and long- term rates of survival) among the pneumonectomy group was significantly low compared to that among the other group of patients. Thomas et al. established that pneumonectomy was an important predictor of poor rate of survival across all NSCLC pathological stages. However, pneumonectomy was no longer a significant contributor after the researchers adjusted for other confounding variables. In addition to this, the study was quite limited when it comes to addressing the impact of pneumonectomy on NSCLC stage I patients. The limitation cannot be ignored given that only twelve such patients were used in the study.
Other studies conducted using fewer patients have identified various variables that determine survival. However, the studies do not provide information on the impact of lung resection on rate of survival. In this regard, the study conducted by Alexiou et al. was better placed to determine the degree of impact of lung resection on rate of survival. Another study by Thomas et al. found that male patients have low rate of survival compared to their female counterparts. As a result, the male gender is a predictor of poorer rate of survival. It is important to note that there is no conclusive scientific provided or available to support this observation. However, many scholars hypothesize that reproductive hormones play a partial role in the growth and development of NSCLC cells. One in- vitro research that was conducted on tissue with NSCLC found that there were large numbers of estrogen receptors. The study also concluded that tamosifen binds to the receptors, which in effect leads to antiproliferative of the tissue. In addition to this, 2- methoxyoestradiol is thought to be an angiogenesis inhibitor, which suppresses the growth of tumors. As a result, the compound induces apoptosis in lung cancer cells.
In their study referred to earlier, Alexiou et al. found that as an independent variable, squamous cells favored rate of survival among T1N0 patients. However, the scholars noted that it is not clear how histology of tumors relates to rate of survival among patients. Other researchers who conducted similar studies did not find any cell type difference with regard to rate of survival. However, other researchers documented that adenocarcinomas are associated with improved overall rate of survival among patients. Alexiou et al. found that SL and pneumonectomy had relatively similar rates of mortality.
However, they also noted that the pneumonectomy group of patients had a greater loss of respiratory function as compared to their SL counterparts. In spite of this difference, Alexiou et al. found that sleeve lobectomy is associated with various side effects. The complications included, among others, the formation of bronchial fistula, local recurrence, and stenosis. Alexiou and colleagues note that practitioners in this field should apply this conclusion with a lot of care. The conclusion should be applied with caution. The practitioner must take into consideration the functional and oncologic circumstances of specific patients.
It is possible to consider the disease process of NSCLC stage I as a localized phenomenon. In such a case, and when the tumor is completely removed, the rate of cure is very high. Nevertheless, most studies have documented that the rate of survival after five years among the patients is approximately 60%. The studies note that a third of these patients develop distant metastases. The distant metastases suggest the spread of tumor cells before surgery. The realization explains the reason why adjuvant therapy is gaining a lot of acceptance among NSCLC researchers and oncologists. More trials are underway to determine the effectiveness of this procedure.
However, given the fact that analysts have not yet established that adjuvant radiotherapy or chemotherapy is definitively beneficial, most hospitals are playing it safe. Practitioners in such hospitals are not administering this form of treatment on stage I NSCLC patients. Moreover, most oncologists are not yet convinced on the efficacy of adjuvant chemo or radiotherapy on stage I NSCLC patients. The main reason is that there is a high possibility of serious side effects associated with the procedures. In their study, Alexiou et al. conclude that pneumonectomy has potent adverse impacts on the rate of survival among stage I NSCLC patients. As a result of this, the scholars recommend that pneumonectomy should be avoided if it is possible to completely remove a tumor using the less aggressive and smaller resection procedures.
Radiotherapy and Local Recurrence: Bronchial Stump Recurrence
The discussion on the efficacy of radiotherapy as far as the treatment of tumors on bronchial stumps after resection is concerned is wide and deep. Law, Henk, Lennox and Hodson conducted a retrospective study whose major objective was to determine the value of radiotherapy in the treatment of bronchial carcinoma after resection. The scholars collected and analyzed from 43 patients who had undergone surgery to treat bronchial carcinoma. The surgery on the patients was conducted using either pneumonectomy or lobectomy procedures.
In their study, Law et al. found that five patients survived recurrence of bronchial carcinoma for five years or more. The tumors of the five patients were confined to the bronchial stump region and had received radical irradiation. When bronchoscopy was conducted later, it was revealed that the recurrent tumors had been completely eradicated. The scholars did not document any benefits associated with irradiation among 20 patients, who were suffering from recurrent NSCLC. Law et al. did not find any difference with regard to overall rate of survival or subsequent recurrence of cancer between patients who received radiotherapy after resection and those who did not undergo the procedure. In addition to this, the researchers did not establish any difference regarding prognostic features between the group of patients who received irradiation and those who did not. In spite of the fact that their study included all cases that occurred within a period of 10 years, the number of patients used was not large enough to demonstrate a probable small benefit of radiotherapy in the treatment of recurrent bronchial carcinoma. The scholars suggested that the patients who showed recurrence after irradiation may have had tumors that were biologically unfavorable.
Radiotherapy and Local Recurrence: EBRT
A number of studies in this field have documented the effectiveness of EBRT in the treatment of locoregional recurrent NSCLC. The studies documented this effectiveness using EBRT alone. Jeremic et al. conducted such a study to find out whether the technique was useful in treating recurrent NSCLC after a complete resection is carried out on a patient.
The researchers used medical records of NSCLC patients who had visited the Kragujevac University Hospital between 1982 and 1993. The scholars used a number of inclusive criteria. For example, patients who had developed locoregional recurrence after curative surgery were selected for the study. Patients who had small cell lung cancer, those who were receiving chemotherapy, and those who had developed distant metastases were excluded from the study. Radiation treatment was administered using 10MV photons from X-ray linear accelerators. The individuals addressed with a curative intent received between 55 and 60 Gy in 26 to 30 fractions.
On the other hand, those patients who were treated with a palliative intent received a total dose of 30 Gy. The radiation oncologist in charge determined the kind of treatment the patient would receive, whether curative or palliative. Parallel opposed fields were used for the first course (40-45 Gy) of curative therapy or the entire course of palliative therapy. After attaining spinal cord tolerance levels, the patients on a curative regimen received additional 10 to 15 Gy. The chi- square test and the student’s t– test were used to determine the differences between the symptom improvement and characteristics of the different groups of patients. Rate of survival for the patients was calculated using Kaplan- Meier method.
The patients were divided into two groups. One of the groups received low dose radiation therapy, while the other group received high dose radiotherapy. The potential prognostic factors for the two groups of patients were largely similar. The MST for all the patients selected for the study was 13 months. The participant’s rate of survival at one, two, three, four, and five years was 61%, 28%, 16%, 9.8%, and 9.7% respectively. The differences between the two groups with respect to MST and one to five years rates of survival were significant. The findings were 74%, 36%, 24%, 14%, and 14% for high dose and 32%, 11%, 0%, 0%, and 0% for low dose respectively (p<0.000).
Twenty eight out of the 39 patients (72%) received high dose EBRT. The condition of this group of patients improved with regard to symptoms. On the other hand, 8 out of 19 patients (42%) among those who received a low dose showed improvements. The difference between the two groups was statistically significant (p<0.029). Fifty percent of the patients who had received a high dose of radiation experienced re- recurrence, while 74% of those who received a lower dose experienced re- recurrence. Distant metastasis between the two groups was largely similar. Age, time from the first surgery to recurrence, the extent of initial surgery, performance status, histology, and weight loss had no impact on the rate of survival among the patients. Female patients performed significantly better compared to their male counterparts.
The initial stage of the disease had a significant impact on the rate of survival among the patients. Those who had an initial diagnosis of stage I disease performed better than those diagnosed with stage II and stage III. However, there was no significant difference between the outcomes of patients with stage II and stage III initial staging (p<0.18). The impact of recurrent staging on rate of survival was similar to that of similar staging. What this means is that patients who had recurrent stage I NSCLC had better outcomes with regard to MST and survival rates compared to their stage II and stage III counterparts. However, there was no difference between the outcomes of stage II and stage III patients. Patients with a recurrence at bronchial stump site had significantly better outcomes compared to those who had chest wall or nodal recurrence.
In addition, Jeremic et al. analyzed local re- recurrence with regard to the post- surgical location of recurrence, which had been treated using radiation therapy. However, there was no significant difference between the group of patients treated using a high dose and the group of patients treated with a low dose with respect to the various initial locations. When the outcomes of all 61 patients were analyzed, a marginal significance was evident.
In his study, Lester reported that the median rate of survival for the patients used was 12 months. In addition, a survival rate of 21 percent and 5 percent after two and four years respectively was recorded. In a similar study, Verstegen et al. documented a 12 month median rate of survival and a 10% rate of survival after 5 years. The scholars also observed that there was a 48% treatment failure, while 57% of the patients experienced distant metastasis. The findings of Jeremic et al. were in agreement with those of other researchers who documented an overall rate of survival of between 5 and 10% over a period of five years. The scholars also determined that the rate of survival for stage I NSCLC patients who had developed locoregional recurrence was better (at 57%) than that of stage II patients (at 13%) and stage III patients (at 3.7%). The survival rate for stage II and stage III patients was similar to that of newly diagnosed cases, which were treated using radiotherapy.
For patients with a recurrence in bronchial stump, high dose of radiation was particularly effective. The findings made by the scholars proved that in comparison to other sites, recurrence at the bronchial stump is favorably treated using radiotherapy. The median rate of survival for patients who had suffered recurrence at the bronchial stump was 38 months, while their five- year rate of survival was 33%. On the contrary, only one patient lived for more than five years after radiotherapy without the evidence of NSCLC. The patients who were diagnosed with combined nodal and stump recurrences, together with those who had pleura and chest wall recurrence, performed very poorly. The observation was in agreement with that made in other studies, which have posited incurability of recurrence at these sites.
Jeremic et al. confirmed that bronchial recurrence for stage I: T2N0 is associated with excellent rate of survival, which is comparable to that obtained through surgery among new cases at the same stage. Although there are very few NSCLC patients who fall under that category, it is essential to emphasize on the importance of using radiotherapy for improved treatment outcomes. Jeremic et al. did not determine whether such patients had better outcomes than their newly diagnosed counterparts, who were treated with EBRT. The scholars made an interesting observation. They found that incidences of local failure in most of the studies were quite similar. In most studies, the incidence is between 45 and 65 percent.
The pattern of failure in the study population was local. It is possible there are some biological characteristics responsible for the recurrence of the tumors. However, Jeremic et al. did not establish the presence of such biological properties. Such an observation, coupled with their findings using EBRT with doses of more than 55 Gy, is an indication of the possibility of achieving better outcomes by increasing the dose. Today, it is possible to target high doses to a tumor and attain improved irradiation with the use of three dimensional conformal radiotherapy techniques.
Jeremic et al. did not find any differences between the uses of high and low doses when they analyzed re- recurrences among the patients. They were trying to establish differences with respect to the initial location of the tumor and the dose of radiation used to treat the tumor. However, recurrences at the bronchial stump had least re- recurrence when treated curatively, compared to recurrences on other locations. In a similar study, Nitsche et al. also did not find any relationship between the pattern of failure and location of recurrence. Patients who had recurrence at the bronchial stump had lower rates of failure after irradiation with low dose than other patients. The same trend was observed among patients who were on higher doses of radiation. Jeremic et al. found that rate of survival was not only influenced by recurrent staging, but also by the initial staging. On the contrary, Nitsche et al. did not find any relationship between staging (either initial or recurrent) and the outcomes of treatment among the patients.
Radiotherapy and Local Recurrence: Aggressive Therapy
Curran et al. conducted a study to find out whether NSCLC patients who had developed locoregional recurrence should receive aggressive therapy. The sample used in the study included 11 female patients and 26 male patients with a median recurrence age of 63 years. All the patients used in the study had undergone lobectomy, bilobectomy, wedge resection, and pneumonectomy. Out of the 37 patients, twenty five were diagnosed with nodal recurrences. Table 6 below is a summary of the characteristics of the patients who had locoregional recurrence and newly diagnosed tumors before irradiation:
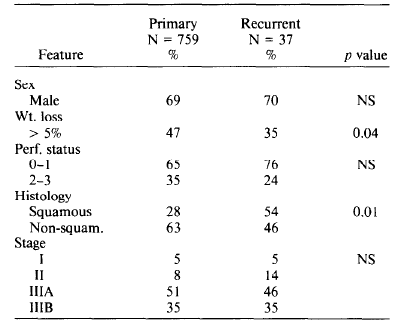
The information in table 6 above reveals that local recurrence patients had a higher squamous histology compared to primary patients. Curran et al. found that the median rate of survival for the two groups was the same (at 12 months), while the two year rate of survival was 22% among locoregional recurrence patients and 26% among primary patients. This is shown in figure 4 below:
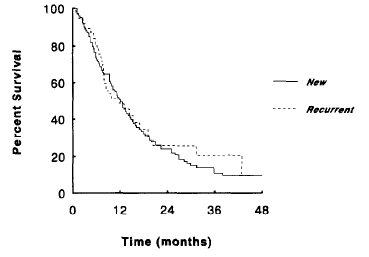
In addition, Curran et al. documented the tumor progression pattern among the recurrence patients after radiotherapy. They carried out the same procedure on 36 percent of the primary cases. The scholars did not find any significant differences between the patterns of failure among the patients with regard to site of recurrence. The researchers noted that the prevalence of locoregional recurrence among NSCLC patients after resection is largely determined by resection completeness, use of adjuvant radiotherapy, and histologic subtype of the cancer. The observation explains the reason why there are differences in the failure rates reported by different researchers in this field. The rate of locoregional recurrence is higher among stage III patients as compared to patients in the other stages. The rate of recurrence ranges from less than 10 percent for those patients who receive radiotherapy after surgical operation, to between 30 and 40 percent among those patients receiving incomplete resections and those who do not receive adjuvant radiotherapy.
Curran et al. note that in spite of the fact that there are at least 3000 cases of locoregional failure, there is little information on the outcomes of treatment among such patients. Some reports provide information on the use of aggressive surgical procedures, such as tracheal sleeve, pneumonectomy, resections of the chest walls, and completion pneumonectomy to locoregional recurrence after resection. The reports indicate that some patients survived in the long term after going through such aggressive procedures. However, the scholars acknowledge that the reports have various limitations. For example, it was not possible to ascertain rate of survival among such patients.
In the study conducted by Curran et al., only a small number of the patients met the criteria for salvage surgery as a result of high nodal involvement. It is only those patients with recurrences on the wall of the chest (without nodal involvement) that are treated with subsequent surgery. In their study, Petrović et al. reported that surgery was beneficial to newly diagnosed NSCLC patients with locally advanced disease. It was also beneficial to those patients with tumors confined to the chest wall as opposed to those with extensive nodal involvement. Curran et al. suggested that this postulation was applicable in locoregional recurrence.
Just like Curran et al., Clarke et al. found that when radiotherapy is used in the treatment of recurrent NSCLC, recurrence at the bronchial stump was favorably treated, leading to improved local control. Hallqvist, Bergman & Nyman conducted a study that used data collected from 50 patients, who were treated using either radiotherapy alone or a combination of radiotherapy and chemotherapy. The scholars observed a 13 month MST and 30 percent two- year rate of survival. They did not find any statistical advantage for using chemotherapy in combination with radiotherapy. Curran et al. found that the outcomes of patients with locoregional failures after a primary resection was highly comparable to that of newly diagnosed cases when treated with EBRT. The characteristics of patients before treatment, which influence rate of survival among newly diagnosed NSCLC patients, include, among others, nodal involvement degree, performance status, and weight loss before treatment. In addition, such characteristics predict the outcomes in locoregional recurrence patients.
In addition to this, Curran et al. found that the site of recurrence is very important in determining the rate of survival for patients undergoing radiation therapy for recurrent NSCLC. The scholars also found that the locoregional progression was predominant at the site of tumor failure. They concluded that measures should be put in place to address the problem. For example, the scholars recommend the use of tomotherapy to increase dose of radiation delivered to the bronchial region, which is not associated with the complications that come with higher EBRT doses. Studies have found that recurrences at the bronchial stump post improved outcomes when treated with tomotherapy than when treated using other procedures. The technique is very important and it helps in achieving local control of tumors on the wall of the chest. Some studies have pointed out that there are other approaches that are used to improve the outcomes of EBRT when treating patients with locally advanced NSCLC. The alternative approaches include, among others, fractionation radiotherapy, radiotherapy with chemotherapy, and radiotherapy followed by surgery.
Radiotherapy and Local Recurrence: Curative Radiotherapy
Kagami et al. conducted a retrospective study to determine the outcomes and characteristics of patients who were treated for recurrent NSCLC using surgery. The patients were later taken through curative radiotherapy. The investigators in this study used data gathered from the medical records of 32 patients who had visited the Hokkaido Cancer Center from 1981 to 1991. Three of the patients whose records were used in the study were female, while twenty five of them were male. Their median age was 66 years. The performance status of twenty five of these patients was either 0 or 1. In addition to this, there were six grade 2 patients, two grade 3 patients, and 0 grade 4 patients. By the time they were undergoing the initial surgical treatment, 12 patients were at stage I, 5 were at stage II, 9 at stage IIIA, 2 at stage IIIB, and pathological stage of 4 patients was unknown.
The recurrence of tumors among the patients was diagnosed using computed tomography, chest X- rays, or bronchoscopy. Ten of the patients were diagnosed with recurrence at the bronchial stump. Fourteen patients had supraclavicular and/or mediastinal lymph node recurrence, in addition to recurrence at the bronchial stump. Eight patients did not have bronchial stump recurrence, but they had supraclavicular and/or mediastinal lymph node recurrence. In all the patients used in the study, malignancy was confirmed either cytologically or histopathologically. Squamous cell carcinoma was present in twenty patients, adenocarcinoma in ten patients, and only one patient had large cell carcinoma.
The recurrence of the tumor was observed 5 to 47 months after the initial operation, with a median time of 18 months. Out of the total number of 32 patients considered for the study, none had distant metastasis. All the patients were irradiated using linear accelerator X-ray at 10MV, delivering 2.5 Gy each day for 4 days in a week. The patients received between 47.5 and 65 Gy of radiation. Twenty five patients out of the total number of patients used in the study received more than 60 Gy of radiation, while seven received 60 Gy or less. Chemotherapy was not offered to the individuals prior to initial resection and radiotherapy.
By the time the patients were diagnosed with recurrent disease, they presented various symptoms. The symptoms included, among others, hemoptysis in 7 patients, chest pain in 5 patients, cough in 2 patients, dyspnea in 2 patients, and dysphagia in 3 patients. Thirteen patients did not present any symptoms. One month after radiation therapy, the response of the patients was assessed using radiography and bronchoscopy. Eight patients had completely responded to the treatment, while 13 patients had responded partially. One patient among those who had received less than 60 Gy of radiation had completely responded to the treatment, compared to seven patients from among those who had received a total dose of more than 60 Gy. Fifteen patients had local failure only. Six had distant metastasis only, while six had both distant metastasis and local failure. Five patients did not have any evidence that pointed to treatment failure.
The rate of survival among the patients was 12.5%, 28.1%, and 56.2% after one, two, and five years respectively. The median survival time (herein referred to as MST) was 14 months. Four out of the 32 patients survived beyond five years. The patients who had completely responded to the treatment had a survival rate of 50% after three and five years, while the patients who had shown partial response had a 12% and 0% survival rate at three and five years. The figure below shows the overall rate of survival among the patients:
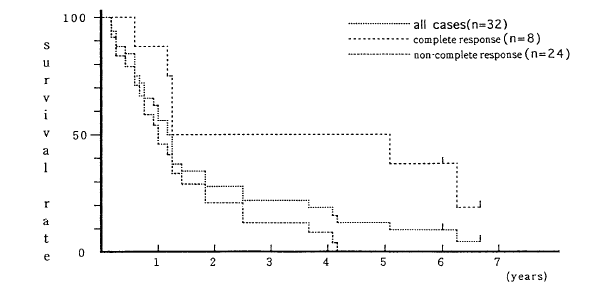
The MST for patients with bronchial stump recurrence was 15 months. The MST for patients with recurrence on the lymph nodes was 14 months, while that of patients with recurrence on the bronchial stump and lymph nodes was 9 months. Esophagitis and pneumonitis were the main toxicities that were experienced by the patients. All the toxicities were either grade 1 or grade 2. The patients did not suffer from severe toxicities in the long-term.
A large number of the patients who experience treatment failure develop distant and locoregional metastases. The development is evident in those patients who, in spite of definitive surgery, still experience treatment failure. However, Simone notes that between 10 and 35 percent of NSCLC patients develop isolated recurrence, whose prevalence is determined by the pathological stage, histological subtype, resection completeness, and administration of adjuvant radiotherapy. Twenty two out of the 32 patients used in the study conducted by Kagami et al. had locoregional recurrence at the lymph nodes and as such, surgery was not a viable salvage option. The findings made by Kagami et al. were in agreement with those made by Jeremic et al.. The latter, in their study, reported that patients who had a complete response to treatment survived longer than those who did not respond or those who had partial response. Kagami and colleagues found that there was a significant statistical difference between the rate of survival among partial responders and complete responders. The scholars concluded that radiotherapy is effective in curative treatment of locoregional recurrence among NSCLC patients.
Radiotherapy and Local Recurrence: High Dose 3D Conformal Radiotherapy
Radiotherapy is the main form of treatment available for stage III NSCLC patients. However, standard radiotherapy does not achieve satisfactory results. Consequently, it is used in combination with other modes of treatment, such as chemotherapy, to improve outcomes among patients and increase the chances of survival in the long- term. The other approach that is used to attain improved results is altered dose fractionation. There are various trials conducted in the field to determine the effectiveness of dose escalation for improved treatment of NSCLC. According to Simone, patients who received radiation doses of 60 Gy had better outcomes than those patients who received lower doses.
However, the toxicities that are related to radiotherapy also increase in tandem with the dose delivered. Zhang showed that with a limited target volume, it is possible to deliver between 64 Gy and 103 Gy of radiation safely using 3- D conformal radiation therapy. Everitt et al. increased the radiation dose from 55 to 72 Gy with the use of 3- D conformal radiotherapy for the treatment of stage III NSCLC patients. They documented that the incorporation of the 72 Gy dose with neoadjuvant chemotherapy (carboplatin or paclitaxel) gave rise to an MST of 24.5 months.
It is thought that high- dose irradiation has better outcomes for NSCLC patients in comparison to standard radiotherapy. Nakayama et al. conducted a study to compare the outcomes of stage III NSCLC patients who had received high- dose treatment using 3D- conformal radiotherapy with those of the patients who were treated using conventional radiotherapy. The scholars used information collected from 100 patients who were diagnosed with stage III NSCLC at Tsukuba Medical Center Hospital from May 1999 to April 2006. The diagnostics processes included a detailed history of the patient, chest radiography, physical examination, histological confirmation, and CT examination. Thirty three patients had stage IIIA disease, while 67 patients had stage IIIB disease.
The patients were divided into two groups. The first group was named the conventional group, while the second group was named the conformal group. Their average age was 64 years. There was a balance between the two groups, but the conformal group had a larger gross tumor volume average compared to the conventional group. The patients in the conventional group received an average irradiation of 60 Gy, while the patients in the conformal group received an average dose of 64 Gy. Twenty patients from the group that received conformal radiotherapy were put on hyperfractional irradiation that totaled to 70Gy. In this setting, the patients received 1.2 Gy of radiation twice a day as opposed to 2.0 Gy in a day. Fifty two patients were given sequential chemotherapy while 48 were given concomitant chemotherapy. The MST for the group that received conventional radiation treatment was 13.2 months while that of the other group was 17.3 months. The survival rates after one, two, and three years for the conventional group was 51.0%, 21.2%, and 9.2% respectively. On the other hand, the survival rates after one, two, and three years in the conformal group were 66.7%, 35.2%, and 31.1% respectively. There was a significant difference between the survival rates of the two groups (p<0.04).
The median disease- free survival time (herein referred to as DFS) for the patients in the conventional group was 6.3 months, while that of patients in the conformal group was 16.8 months. Again, the difference in disease- free rate of survival was statistically significant. The one and two years disease free survival rates in the conventional group were 30.2% and 9.3% respectively, while the rates for the conformal group were 49.5% and 30.1% respectively. The one, two, and three years local progression- free rates for the patients in the conventional group were 73.2%, 39.9%, and 30.1% while the corresponding rates for the patients in the conformal group were 86.5%, 78.3%, and 50.1%. There was a significant difference between the local progression- free rates of the two groups. The table below shows the primary site of recurrence among the patients that were considered for the study:
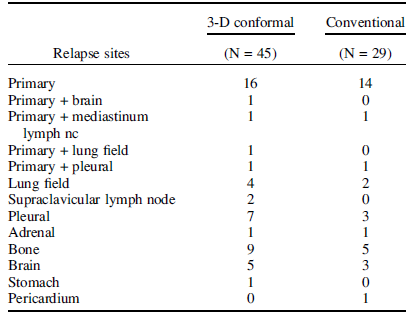
From the findings made by Nakayama et al., it was clear that increasing the dose of radiation therapy led to better outcomes in the treatment and management of stage III NSLCL. The use of 3D- conformal radiotherapy allows for the selection of optimal beam combination and direction. The ability to select optimal beam combination and direction makes it possible to escalate the dose of radiation without excessive lung, esophagus, cardiac, and spinal cord toxicities.
Wu et al. documented that increasing the dose of radiation increases the MST among stage I and stage II NSCLC patients. The MST for the patients used in the study was 35 months. Fifteen percent of the patients had grade 3 esophageal toxicities. Schild et al. reported on the findings made on 69 patients who underwent escalation radiation and concurrent chemotherapy. Grade 3 esophageal toxicities were observed among 40% of the patients who received gemcitabine and 17% among those who received paclitaxel and carboplatin. The rates of local control were improved, but on irradiation of regional nodes, there were increased toxicities in the lungs and in the esophagus. In conclusion, the researchers pointed out that where lymph nodes are involved, a reduction in the dose of radiation reduces toxicities and leads to improved rates of survival. By omitting nodal radiation, Zhang managed to escalate the dose of radiation without necessarily increasing the level of toxicity by the use of conformal radiotherapy.
McGibney, Holmberg, McClean & Armstrong conducted a similar study to find out the effectiveness of dose escalation among stage 1, stage II, and stage III NSCLC patients. All the patients used in the study were curatively treated with between 70 and 103 Gy. The scholars managed to achieve a MST of 16 months among stage III patients, who also had an overall survival rate of 37% after two years. The scholars concluded that it was possible to increase the dose to the targeted volume and achieve better outcomes by using of 3D- conformal radiotherapy. Werner-Wasik et al. compiled a retrospective report that involved 50 patients. All the patients used in this retrospective study had stage III locally advanced disease. By dose escalation, the scholars managed to attain an MST of 18 months and a 12 months median progression- free survival, where only two patients had experienced grade 3 esophageal toxicities.
In the study that was conducted by Nakayama et al., and which was referred to earlier in this paper, the MST was 17 months and the rate of survival after two years was 35% in the group that received 3D conformal irradiation. The findings were comparable to those made in other studies in the same field. The incidence of grade 3 esophageal toxicities was also quite low in the study by Nakayama et al. In another study that was done by Gillham et al., only 8 percent of the 68 patients used in the study developed grade 3 or worse esophageal toxicities.
Nakayama et al. used radiation that was between 60 Gy and 74 Gy, which was administered concurrently with carboplatin and paclitaxel. The researchers outlined that it was possible to predict esophageal toxicity by determining the length of esophagus that will be irradiated in the 40- 60 range of Gy. The scholars found that only one patient who was irradiated with more than 60 Gy using 3D conformal radiotherapy experienced grade 3 esophageal toxicity. The esophagus of this patient was 15cm in length. The study showed that it was possible to increase the survival of stage III NSCLC patients and reduce toxicities when the irradiation dose was increased by the use of conformal technology. The development can be achieved by avoiding the irradiation of the regional node. It is quite clear that the use of 3D conformal radiotherapy increases outcomes of treatment among NSCLC patients. However, it is important to note that most of the studies conducted in this field are retrospective in nature. As a result of this, the studies are bedeviled by a number of time related limitations. In this regard, clinical trials should be conducted to check the veracity of the findings in the reports.
Effects of Radiotherapy
Effects of Radiotherapy: IMRT and 3DRT on Cardiac Irradiation
Conformal radiotherapy techniques, such as IMRT, deliver radiation doses to tumors located in complex positions. It is noted that the techniques lead to reduced irradiation of uninvolved normal tissues compared to other techniques. The reduced irradiation has the potential of reducing the toxicity of organs, thus making it possible to escalate the dose of radiation targeting a specific volume. Sometimes, there is a risk of dose dumping and deposition in areas that were not delineated when organs that are at risk are avoided. At times, it is not possible to sufficiently irradiate the areas with the use of conventional radiotherapy, which leads to unexpected toxicity. Furthermore, IMRT is associated with improved dose homogeneity in the target volume and conformity. As a result, normal tissue receives minimal irradiation only.
While scientists are making efforts to perfect the IMRT technique, many oncologists are moving towards the use of combined modality treatments to manage solid malignancies. The shift is motivated and supported by the evidence gathered from various pre- clinical studies, which have justified the combination of radiation and drugs. The move is also supported by the results of various clinical trials. In spite of the fact that the quality of data regarding the volume of normal tissue that is exposed to toxicity when such regimens are used is not sufficient, combined modality treatments are in most cases linked to higher toxicity. One important question is how chemotherapy (intensity, type, and presence) affects the ranking of radiation techniques with regard to their level of toxicity. How does chemotherapy affect the ranking when the techniques are used to deliver the same amount of radiation while the distribution of dose on normal tissue is different? Specifically, there is the question of whether chemotherapy determines the impact of IMRT or 3D-CRT with respect to normal tissue toxicity among NSCLC patients.
NSCLC remains as one of the most difficult diseases to manage. Optimal non- surgical treatment involves the combination of radiation therapy and chemotherapy. The lung is not only surrounded by healthy tissue, but it is quite sensitive to toxicity. As a result of this, it is very difficult to provide curative therapy without the risk of side- effects. Vogelius et al. conducted a similar study in this area to determine the difference between tomotherapy, IMRT, and 3D- CRT with regard to the risk of radiation induced side effects on the lung. The scholars made their evaluations by including chemotherapy, which was believed to act isotropically and independently throughout the lung.
The scholars included 18 NSCLC patients in their study. The patients used in the study had sought for treatment from the University of Wisconsin Hospital. The patients were initially treated using tomotherapy, but they later developed locoregional recurrence. Vogelius et al. altered the three treatment plans to deliver up to 95% of radiation to the target volume. At the same time, the scholars minimized the impact and amount of radiation on the spinal cord, esophagus, and residual lung.
The researchers found that it is possible for the level of toxicity associated with the three regimens to change when other systemic agents are used. When chemotherapy is used as a priming dose throughout the lung at risk, regions of the lung that are exposed to low doses may contribute to reduction in local function, and as a result raise the level of side effects that the organ is exposed to. In this regard, regimens that focus on irradiating only a small volume of the lung have less damage than the ones that target a larger volume with a lower radiation dose. However, this effect is determined by the drug that is used, the combination used, and dose intensity.
The researchers concluded that when chemotherapy is used in combination with radiation therapy, 3D- CRT techniques lead to less toxicity among NSCLC patients. However, chemoradiation dose- effect models should be developed to optimize IMRT plans. Vogelius et al. are of the view that even when tangent treatments are used after patients are taken through breast conserving surgery, radiotherapy is still bedeviled with multiple side effects. The side effects are especially evident among many patients with unfavorable cardiac anatomy. The oncologist is faced with a dilemma given that the left side of the heart receives some amount of the radiation that is targeted at the tumor. In some cases, regions of the PTV are not sufficiently irradiated. Some oncologists recommend that in the case of a patient with a heart that is anteriorly positioned in the concavity, treatment is possible with the use of partial breast radiotherapy. However, unless there are specific indications that point towards partial breast radiation therapy, it is prudent to treat the entire breast.
In addition to this, it is important to note that it is possible to maximize the fluency and angles of tangent fields in a manner that leads to better irradiation of the tumor. If this is done, it is possible to have less cardiac exposure because it extensively blocks the heart. IMRT is especially useful in the geometrically challenging cases, such as pectus excavatum and bilateral cancer. Findings from studies conducted in this area indicate that the technique distributes the dose in a concave manner, leading to a reduction in the number of areas exposed to maximal dose and an increase in the region that is exposed to the lower doses. What this means is that there is an increase in both the median and mean of heart doses.
Coming up with cardiac toxicity models is especially difficult. There are various factors that contribute to this difficulty. The factors include, among others, the definition of the organ at risk (whether left ventricle, heart, or myocardium), scarcity of dosimetric data, and symptom latency of more than 10 years. The major assumption made when coming up with cardiovascular models is that both the heart and myocardium are homogeneously sensitive to radiation. By making this assumption, Hardy et al. plotted dose- response curves and used them to explain the effects of radiation on various partial heart volumes. However, when patients who are suffering from NSCLC, breast cancer, and Hodgkin’s disease are compared, the assumption is proven as false. When the data of NSCLC patients who have undergone a right pneumonectomy is analyzed using the same approach, the cardiac mortality dose- response curves are quite shallow in comparison to breast cancer patients’ data. The same outcome is seen in the case of Hodgkin’s disease. The most surprising observation is that the distribution of radiation dose in breast cancer and Hodgkin’s disease is largely similar. The similarity is brought about by the fact that the right side of the heart receives more radiation than the left part.
There is a lot of controversy surrounding the amount of radiation on the heart that leads to side effects and the type of side effects brought about by the radiation. Controversy also surrounds the determination of the parameters that are important in estimating cardiac toxicity. In this regard, determining the threshold volume beyond which the dose delivered using IMRT might be curative and safe is very essential for safe and optimal use of the technique. It is possible to establish such a threshold through the use of relative seriality.
Vogelius et al. used relative seriality on the high risk patients with tangent radiotherapy. When compared to the findings made by Schytte et al., Vogelius and colleagues indicate a lower risk of cardiac mortality associated with radiation therapy. In spite of the fact that the mean cardiac mortality rate for the study that was conducted by Hardy et al. was 2 percent; one of their subsets had a cardiac mortality of 4.5 percent. Because the patients who were included in the study conducted by Vogelius et al. had unfavorable heart anatomy, the series is largely comparable to that of Bellière et al., which was associated with very high cardiac mortality. Vogelius et al. observed a reduction in cardiac mortality among such high risk patients. The reduction was from 3.4 percent to 0.25 percent when the patients were treated using IMRT. In general, Vogelius et al. concluded that IMRT had a significant effect in reducing the maximal dose delivered to the heart. The effect was very important as it reduced cardiac mortality among patients with unfavorable anatomy.
Effects of Radiotherapy: IMRT and 3DRT on Cardiac Mortality
The use of 3D conformal techniques has reduced the amount of radiation that the heart is exposed to during the treatment of lung cancer and breast cancer. Lohr et al. carried out a study to determine the impact of radiation therapy on breast cancer patients. The study was a comparative analysis of the 3D conformal technique and the IMRT technique. The evaluation of the two plans was done on the basis of a 50 Gy total dose, which was set to be the mean dose for both IMRT and 3D conformal techniques for all patients. The two plans were thus compared with regard to target volume that was covered, the dose delivered to the left lung, right breast and heart, treatment time, treatment efficiency, and homogeneity. Dose- volume histograms were used to calculate the risk of complications.
There was an evident reduction in cardiac exposure in all the patients included in the study. The reduction was observed when IMRT was used. The technique reduced exposure to the maximal dose and to the regions of the heart that were exposed to more than 30 Gy of radiation. There was a 30.9% reduction in the maximal dose that the left ventricle was exposed to and a 10.7% reduction in the mean dose that the left ventricle was exposed to. The reason for this is that as the exposure to the maximal dose reduced, the mean dose also reduced.
In addition, IMRT reduced the heart volume that was exposed to radiation of more than 30 Gy from 45cm3 to 5.8 cm3. The volume of the heart exposed to more than 40 Gy reduced from 13.8 cm3 to 0.46 cm3. The comparison of the two techniques with regard to PTV (planning target volume) coverage and 3D- CRT was found to be only slightly superior. In the tangent techniques, 95 percent of the PTV was covered with 47 Gy of radiation, while in the case of IMRT, 95 percent of the PTV was covered with 45 Gy. IMRT had an acceptable level of homogeneity because only a small fraction of the targeted breast volume (3.8%) received radiations that were more than 110% of the prescribed dose. IMRT led to an increase in both the mean and median heart doses, but a significant reduction in the risk of excess mortality.
Effects of Radiotherapy: Strain Rate Imaging
The prospective cardiac function evaluation among NSCLC patients is important in identifying patients who are at a high risk of experiencing cardiotoxic. Left ventricular ejection fraction (herein referred to as LVEF) is traditionally determined by radionuclide ventriculography or echocardiography. It is then used in monitoring radiation therapy or chemotherapy- induced cardiotoxicity. However, recent studies show that it is not possible to determine early changes in cardiac and myocardial function using LVEF. In addition to this, the sensitivity of the global measure is further blurred considering the fact that the entire left ventricle is not included in the field of radiotherapy. As a result of this, the technique can only detect regional dysfunction after a person has received radiotherapy.
The shortcomings of LVEF have led to the adoption of strain rate imaging (herein referred to as SRI). The adoption of this technique has made it possible to quantify the myocardial deformation properties. As a result, it is now possible to evaluate the regional functioning of the myocardium. It makes it possible for oncologists to notice radiation induced changes in the heart before such alterations are detected using other techniques.
Erven et al. conducted a clinical trial to investigate radiation therapy- induced changes in the cardiac function of breast cancer patients using SRI. Thirty patients were included in the study. Twenty of the patients used in the study had left-sided breast cancer while 10 had right sided breast cancer. Tangent radiotherapy was used in the treatment of all the patients. They all received a total dose of 50 Gy and an additional dose of 16 Gy for those patients who had to undergo breast conserving surgery. However, the 16 Gy boost was not included in the study because its impacts on the dose delivered to the heart are negligible.
Erven et al. did not find any significant difference among the patients with regard to cardiac risk factors, adjuvant treatments, and age. Among the patients who had left- sided breast cancer, the mean radiation dose delivered to the left ventricle was 6.8 Gy while the mean volume of the left ventricle that received 30 Gy of radiation was 11.5%. The corresponding results for patients who had right- sided breast cancer were 0.7 Gy and 0%. The mean dose delivered on the basal, mid and apical left ventricle segment for the patients who had left- sided breast cancer were 4.5 Gy, 7.5 Gy, and 12.2 Gy respectively. They had a median dose of 3 Gy.
There was a slight reduction in the ejection fraction among the left- sided breast cancer patients, but no other conventional parameter had a significant change after receiving radiation therapy. When the patients who had received concurrent chemotherapy were excluded, there was no change at all.
When compared to the results of the baseline survey, there was a significant decrease on Strain (herein referred to as S) immediately after radiotherapy and after two months of follow up. However, there was no significant change in the Strain Rate (herein referred to as SR) among patients with left- sided cancer (p<0.001). Among right- sided patients, the change in deformation parameters was not significant (p<0.006). In comparison to the results of the baseline survey, there was a significant decrease in the apical segment S immediately after radiotherapy and after two months of follow up. The reduction in SR after therapy and after two months of follow up was also significant.
There was no significant change in the deformation parameters of the basal and mid segments in comparison to apical segments after radiotherapy. There was a significant reduction in the S values of the baseline and the segments that had received more than 2.5 Gy of radiation. There was no significant decrease in S value in the segments that had received less than 2.5 Gy of radiation. However, there was no change in the SR parameters for both levels of doses. When the segments that were irradiated with more than 2.5 Gy and those that were irradiated at less than 2.5 Gy were compared, there was a significant difference in both SR and S values immediately after radiotherapy and after two months of follow up. The researchers did not note any significant differences in the SR and S values of the two categories of patients at baseline level.
Erven et al. also tested the impact of confounding factors on the patients using a separate univariate analysis. They carried out the univariate analysis with regard to the reduction in the S value after radiotherapy. The scholars found that there were significant correlations between the reductions in S value on the one hand and the cancerous side, the patients BMI, the mean segmental dose of the left ventricle, and the left ventricle volume that was irradiated at 30 Gy on the other hand.
The findings of the study showed that the myocardial deformation among the patients treated with radiotherapy for breast cancer in the left side was reduced. The reduction was not evident among right- sided cancer patients. They demonstrated that the S and SR indices decreased significantly in the apical left ventricle segments of patients who had cancer on the right breast, but the basal and mid segments did not experience significant reduction.
The scholars also documented that parameters of echocardiography were not sensitive to heart function alterations after radiation therapy. They only recorded a slight reduction in the LVEF after radiotherapy among right- sided patients. However, the value of ejection fraction remained largely within the acceptable range. Aksakal et al. had demonstrated that the LVEF decreased immediately after treatment, but two months later, it went back to normal. Park et al. aimed at determining whether there were any changes in the ejection fraction after radiotherapy and treatment with trastuzumab. From their study, the scholars managed to show a reduction in the ejection fraction after therapy. However, the findings were quite questionable since the decrease in ejection fraction was similar among right and left- sided cancer patients. In addition to this, it was possible the slight reduction in ejection fraction noted in the clinical investigation conducted by Erven et al. was as a result of combined effects of radiotherapy and chemotherapy. The reason for this is that the slight reduction was not observable when the researchers excluded radiotherapy.
S and SR values in the basal, mid, and apical segments make it possible to evaluate dysfunction, which is particularly induced by radiation therapy. It can be achieved by making comparisons between segments that are irradiated at different doses. Erven et al. managed to demonstrate that myocardial function changed significantly after right and left- sided patients received radiation therapy. The findings were in agreement with those made by other researchers in the area. Additionally, Erven et al. demonstrated that there are functional changes between the basal, mid, and apical left ventricle segments after radiotherapy. It is quite certain that the regional differences in myocardial function result from radiotherapy. They are brought about by radiotherapy because the apical segment lies within the radiotherapy field as compared to the basal and mid segments. As a result of this, it is irradiated at high doses in most cases.
The researchers demonstrated that the segments that received more than 2.5 Gy of radiation had a significant reduction in S value after radiation therapy in comparison to the regions that were irradiated at lower dose levels. The investigators chose 2.5 Gy because it was the median dose for all the three segments. They found that the sensitivity of S was higher than that of SR in detecting slight changes in myocardial functions. The reason is that it is easier to interpret S data because it is more noise tolerant compared to the SR data.
Seddon et al. used IMRT to determine the effects of radiation therapy on the cardiac function among breast cancer patients. Six months after treatment, motion abnormalities in the regional wall were observed in 17 percent of the patients. The abnormalities were linked to perfusion defects. The deformities also occurred at the anterior part of the left ventricle, thus corresponding to the part of the heart that fell within the field of radiation.
Marks et al. conducted a retrospective research to evaluate the extent of myocardial perfusion and wall motion after radiation therapy in the long- term (five years and over). According to the scholars, there was abnormal motion of the regional wall in 36 percent of patients with left- sided cancer. However, no such motion was observed among right sided cancer patients. The scholars also detected myocardial perfusion abnormalities among 72 percent of patients with cancer on the left side and 17 percent among those with right- sided cancer. They also compared the benefits of SRI with those of single photon emission computed tomography (herein referred to as SPECT). The benefits included the ability to gather quantitative data, as well as higher temporal and spatial resolutions. Additionally, SRI is widely available, inexpensive, and patient friendly.
In order to draw clinical conclusions regarding the differences in deformation parameters, Erven et al. proposed that larger clinical investigations should be conducted. SRI is a very important technique considering the fact that in addition to detecting slight changes in myocardial functions, it also makes it possible for researchers to obtain regional information. For instance, Erven et al. were able to detect differences in cardiac reaction depending on the radiation dose.
Clinically observable cardiac damage takes more than ten years to develop. As a result, detecting changes in the functioning of the heart at an early stage could predict radiotherapy induced complications that the patient may suffer from later on in life. In addition to this, early cardiac safety assessment is very useful in evaluating new radiation therapy techniques. Today, such evaluations are carried out on the basis of volume data and heart dose. The evaluation is carried out in spite of the fact that radiation therapy induced cardiac dysfunction has dose- volume characteristics that are not yet properly established.
Marks et al. concluded that only doses that are beyond 30 Gy are important when estimating radiotherapy induced cardiac risk. There are other studies reporting the risk of cardiac mortality among patients exposed to radiation dose levels below 5 Gy. Erven et al. observed changes in myocardial function when the left ventricle was exposed to lower doses of radiation. Techniques such as IMRT, respiratory gating, and tomotherapy are known to reduce cardiac doses significantly. However, all the three techniques are time consuming and resource intensive. Such limitations are very relevant in the treatment of NSCLC when the rise in the disease load is taken into account. In this regard, there is need for improved insight to determine the correlation between volume metrics, heart doses, and the resulting toxicity. Such data will be used to sort patients according to the technique that offers them more benefits.
Erven et al. took into account myocardial function alterations only. However, they did not provide any physiopathological mechanisms for this. Moreover, the early changes in myocardial function that were induced by radiation therapy cannot be extrapolated to mean the patients will develop clinical complications in the long- term. Regardless of this, it is quite conceivable that cardiac morbidity may arise because the damage on the endothelial cells will lead to microvascular thrombosis. The damage will later lead to myocardial fibrosis.
Effects of Radiotherapy: Myocardial Perfusion Defects
A large body of evidence points to the fact that archaic radiation therapy techniques, which are used in managing localized NSCLC, reduce cancer- related deaths. However, the techniques results in increased cardiovascular disease and mortality rates. Increased cardiovascular disease among radiotherapy patients who had undergone right pneumonectomy occurred because the techniques exposed the myocardium and coronary arteries to large radiation doses.
In order to reduce this exposure, advanced techniques are designed to deliver high doses of radiation to targeted tumor, but reduce the irradiation of the heart . Tomotherapy is one of the most recent techniques that has received global acceptance in reducing cardiac irradiation. However, it is important to note that heart irradiation during radiotherapy is not completely done away with. There is a possibility that even the most advanced techniques will lead to increased cardiac irradiation.
Evans et al. conducted a study to provide answers to the question of heart irradiation. The patients who were enrolled in their study had undergone radiation therapy to treat left- sided breast cancer. The scholars managed to show that radiation therapy leads to perfusion defects that are dose- volume dependent. They also demonstrated that the defects persist for up to five years after therapy. In addition to this, it was proved that the defects are positively correlated to motion abnormalities in the regional wall. Pregnant patients and those who had contraindications to radiation therapy were not included in the study.
Any pre- existing heart disease, such as arrhythmia, coronary disease, angina, congestive heart failure, and myocardial infarction, and other main risk factors that can lead to the development of cardiac conditions, such as a history of using tobacco, hypercholesterolemia, diabetes mellitus, family history obesity, and age, were obtained for all the patients before the study was initiated. The participants’ menopausal status, chemotherapy and hormonal therapy details, and BMI were also recorded.
All the patients were treated using tangential radiotherapy, where each received a total dose of between 46 and 50 Gy. The dose was delivered in fractions of between 1.8 and 2 Gy each day. Some patients, whose breasts were still intact, received an additional 16 Gy.
The investigators reasoned that set- up errors would have the highest effect than other errors among patients who had a small percentage of their left ventricle within the radiation therapy field. Among patients with large volumes of the left ventricle in the radiation therapy fields, it was noted that slight changes in the set- up of the patient would change the volume of the left ventricle that falls under the fields. However, the scholars found that this had no impact on the development of perfusion defects. In the same manner, slight set- up deviations would not necessarily result in cardiac irradiation among patients whose hearts were out of the field of radiation. In this regard, the study by Evans et al. mainly revolved around a group of 17 patients whose left ventricles had the least interaction with the field of radiation.
The scholars used the single photon emission computed tomotherapy (SPECT) technique to determine ejection fraction, regional wall motion, and myocardial perfusion. The study included 108 patients. One of the study’s objectives was to determine the relationship between the volume of the left ventricle that was irradiated and factors that were specific to the patients, as well as perfusion defects. They considered the perfusion defects rate at various intervals after the patients had completed radiation therapy. The time points were 6 months, 6- 24 months, 36- 60 months, and 6- 60 months.
The scholars did not take into account the severity of defects. On the contrary, they only indicated their presence or absence. Each patient was selected once for each of the intervals, regardless of whether the defect would persist in the next time points or not. At the four time points, the scholars evaluated 99 patients (6 months), 108 patients (6- 24 months), 14 patients (36- 60 months), and 108 patients (6- 60 months). The perfusion defects rates for the different time points were recorded. The rates were 34%, 43%, 68%, and 55% respectively. In concurrence with earlier studies, the left ventricle percentage that fell under the field of radiation remained as an important perfusion defects’ predictor after treatment with radiation therapy.
When the investigators conducted a univariate analysis on the data collected, they found that a BMI of more or equal to 25kg/M2 was the only factor specific to patients with a direct and positive correlation with the development of perfusion defects at various time points after radiation therapy. The corresponding rates of perfusion defects for the different time points were for patients with a BMI of more or equal to 25kg/M2 were recorded. The results were 43% (for 6months), 55% (for 6- 24 months), and 68% (for 6- 60 months) respectively. The rates of perfusion defects for patients whose BMI was less than 25kg/M2 was also recorded. The results were 21% (for 6 months), 24% (for 6- 24 months), and 33% (for 6- 60 months) respectively. The variation between the two categories of patients was statistically significant (at p<0.0024, p<0.0024, and p<0.004 respectively). The patient’s racial background had a significant effect on the outcomes of perfusion defects in the first time point of 6 months. It was found that non- Caucasian patients had a 78% perfusion defect rate while Caucasians had a 50% rate. The differences after the first time point were not very important.
From the multivariate analysis, it was found that controlling the effects of the body mass index of more or equal to 25kg/M2 and the irradiated volume of the left ventricle were the only factors specific to patients with a positive relationship with the rate of perfusion defects over various time periods after receiving radiation therapy. Patients with a BMI of more or equal to 25kg/M2 had a 2.50 to 4.40 propensity of developing perfusion defects after radiation therapy as compared to patients with a BMI of less than 25kg/M2.
There were set-up errors recorded in 83 patients out of the 87 patients that were evaluated in this regard. Thirty three of the patients had very deep tangents while the tangents were too low for 50 patients. There were no set-up errors recorded in four patients. The investigators evaluated the effects of patients’ BMI on set- up errors. There were no significant differences between the deep set-up errors of patients with a BMI of less than 25kg/M2 and those of patients with a BMI of more or equal to 25kg/M2. However, there was a significant difference between the shallow set-up errors of patients with a BMI of less than 25kg/M2 and those of patients with a BMI of more or equal to 25kg/M2.
The researchers analyzed the results to determine the impacts of set- up errors on the incidence of perfusion defects. They examined this phenomenon using 17 patients whose left ventricles were 0.02% and 1% within the field of radiation. The patients had a very low risk of developing radiotherapy cardiac complications and dysfunction because of the small volume of the left ventricles that was irradiated. Very deep set-up errors were noted among 6 patients and very shallow errors in 10 patients. One patient was included in this analysis because the simulated tangent depth was the same in the port films. The researchers found that the patient who had very deep tangents had increased likelihoods of developing perfusion defects compared to his counterparts whose tangents were too shallow.
In this study, 13 patients did not have any part of their left ventricle irradiated by the fields of radiation therapy. Six patients had very deep set-up errors. An additional six patients had very shallow errors while one patient had the same depth of tangent for both port films and simulation. In this category of patients, only one had a perfusion defect after radiation therapy. The patient had a BMI of more than 25kg/M2 and a very deep set-up error during treatment. For patients in this group, there was no relationship between set-up errors and BMI or set-up errors and perfusion defects.
The findings made by Evans et al. showed some discordance in the 36- 60 months interval. It was possible the discordance was caused by the fact that the number of patients evaluated in the time- point was significantly less compared to that in the other intervals or to that of patients who have recovered from their earlier defects. Seddon et al. showed that the dependence of perfusion defects on radiation dose is quite constant with the passing of time. In addition to this, some patients were not scanned at later time periods because the investigators rescanned those patients who had shown defects in the earlier time points. Such a bias in selection may have largely contributed to the findings in later time points.
In the same manner, the impacts of BMIs that are more or equal to 25kg/M2 were only noted in the other time periods, with the exception of 36- 60 months. It is possible the inconsistency was caused by the fact that only a few patients fell within the time point. It can also be explained by the fact that perfusion defects have a reversible nature. However, it is important to note that there is a possibility the manner in which high BMI contributes to perfusion defects is linked to set-up errors. In the entire cohort, there was a relationship between a high BMI and very deep set-up errors. What this means is that there is a high possibility that a large volume of the left ventricle will be irradiated. The observation was not made on patients with a low BMI. Similarly, the high incidence of very deep set-up errors among the patients who had only a very small volume of their left ventricle in the radiation field, and who had a BMI of more or equal to 25kg/M2 , seemed to have contributed to increased rates of perfusion defects.
One of the most interesting findings in the clinical investigation conducted by Evans et al. was that set-up errors in treatment can increase the effects of radiation therapy on normal tissue. What this means is that care should be taken when setting up the treatment. The quality of the immobilization device, morphologic changes, as well as other such factors is known to have an impact on patient’s set- up quality on a day to day basis. It is possible to improve the accuracy of set- up by embracing techniques like cone- beam CT, on- board imaging, and optical methods.
Nogueira et al. investigated the link between radiotherapy induced toxicity and cardiac risk factors using animal models. The researchers suggested that dietary cholesterol and radiation therapy affects the incidence of coronary atherosclerosis in birds. They made similar observations when they used rats and rabbits in place of birds. They also found that left ventricle hypertrophy and hypertension made rats more susceptible to radiation induced heart ailments than other techniques.
Many studies have documented the effects of incidental irradiation on the heart, especially with respect to the treatment of Hodgkin’s disease and breast cancer. However, very few studies have reported on the impacts of factors that are specific to patients on the modulation of radiation therapy induced toxicity in the heart. Askoxylakis et al. researched on the effects of age on myocardial infarction after radiation therapy among women who had received treatment for locoregional breast cancer. When they controlled for age, the researchers found that the relative risk for myocardial infarction among women with breast on the left side was 1.18 in comparison to those who had cancer on the right- side breast.
When they factored in age, the scholars found that the relative risk for myocardial infarction among women with left- sided breast cancer was higher for those who were less than 60 years of age compared to those who were more than 60 years. They also determined that in the long- term, the effects of laterality of cancer on myocardial infarction after radiation therapy were very pronounced. The relative risk for myocardial infarction in left versus right –sided cancer among women who were less than 60 years increased from 1.45 in five years after radiation therapy to 5.3 in ten years after radiation therapy.
Askoxylakis et al. examined how radiation induced heart disease is affected by different clinical factors years after the patients have received treatment. They concluded that hypertension, increased age, history of tobacco use, hypercholesterolemia, obesity, and diabetes mellitus were positively correlated with risk to cardiac morbidity after receiving radiation therapy. Evans et al. did not find such factors to be predictive for perfusion defects that are induced by radiotherapy. However, it is important to note that the end points of the various studies are different. For example, perfusion defects in the case of Evans et al. and myocardial infarction for Askoxylakis et al. are different.
Evans et al. concluded that the irradiated left ventricle is one of the main predictors of perfusion defects that are induced by radiotherapy among patients with breast cancer on the left side. It suffices to note that radiotherapy affects NSCLC patients who have undergone right pneumonectomy in the same manner. Patients who have high BMIs are also at a high risk of developing perfusion defects after radiotherapy because they are more likely to have very deep set-up errors compared to other patients. In order to reduce the risk of perfusion defects, deliberate efforts should be made to make sure that the heart is excluded from the radiation field during simulation and treatment.
Effects of Radiotherapy: Changes in Myocardial Perfusion and Coronary Artery Distribution
Some of the factors mentioned in most studies with regard to the development of cardiac toxicity after radiation therapy are volume of the irradiated left ventricle, chemotherapy treatment, large radiation fractions, hyperlipidemia, and orthovoltage radiation. SPECT is one of the most important and fundamental techniques used to access myocardial perfusion.
There are very few studies conducted to determine the time it takes to develop radiation induced cardiac defects. Lind et al. carried out a study to establish the relationship between changes in myocardial perfusion on the one hand and the percentage of the left ventricle that is irradiated, coronary distribution, and factors related to increased risks of complications of the heart on the other hand. The study was carried out on left sided breast cancer patients. In addition to this, the scholars attempted to examine the perfusion defects’ time course. The study involved 69 patients. The characteristics of those patients are shown in the table below:
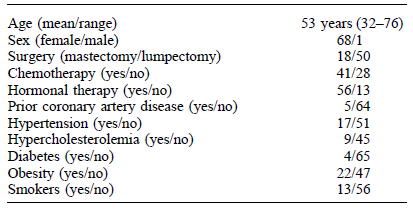
The patients received adjuvant chemotherapy before receiving radiation therapy. Hormonal therapy was administered after radiotherapy. The patients received a total dose of between 46 and 50 Gy using tangential radiation therapy in fractions of 2 Gy per day. A cardiac block came in handy at this juncture. It was applied to shape the fields to reduce irradiation of the heart. After receiving radiation therapy, the patients were scheduled for SPECT at 6 months, 12 months, and 18 months. The perfusion scans before radiotherapy and afterwards were then analyzed.
In this study, two methods of analysis were used to analyze the scans. The two methods were the bull’s eye view method and the semi- quantitative technique. In the quantitative method (bull’s eye view), perfusion defects were attributed to the right coronary artery (herein referred to as RCA), left circumflex artery (herein referred to as LCX), and left anterior descendent artery (herein referred to as LAD). LAD distribution changes after six months were categorized variously. They were categorized as nonexistent if their extent was less than 1%, small if the extent was between 5 and 10%, medium if more than 10% but less or equal to 20%, and large if they were more than 20%. In the quantitative method, severity that was not evident was accorded no point, mild-1 point, moderate- 2 points, and severe- 3 points. Afterwards, the results obtained from the two methods were compared.
The investigators found that tangential radiotherapy among patients was correlated to perfusion defects in the short- term in the LAD distribution, which corresponds to radiation portals. They did not find any defects in the RCA or LCX distributions because the two do not fall under the tangential beams. They also managed to confirm that the volume of the left ventricle that is irradiated is the largest contributor to the changes in LAD distribution SPECT six months after radiation therapy. The patients included in the study did not develop any cardiac events of clinical importance in the short term. However, the investigators recommended that the volume of heart falling under the radiation fields should be reduced. They also recommended that 3D conformal radiotherapy should be used in the place of tangential radiation therapy. The reason for this is because perfusion defects may bring about clinical complications in the long- term.
In addition, Lind et al. proposed that the tamoxifen intake and hypercholesterolemia may contribute to the development of perfusion defects. Other studies have mentioned that high- lipid diets are positively correlated to cardiac morbidity after radiation therapy. In other studies, tamoxifen was shown to have a positive relationship with fibrosis and changes in lung density. However, such studies noted that the observation cannot yet inform practice. As a result, the relationship between radiation therapy induced morbidity and tamoxifen should be studied further.
Radiation therapy is known to cause cardiac injury through two major mechanisms. The mechanisms include damaging the macrovasculature or the microvasculature. The latter is brought about by the destruction of endothelial cells in the capillaries of the heart muscle after they are irradiated. Such damages lead to vessel lumen obstruction, capillary swelling, and myocardial fibrosis. On the other hand, macrovasculature damage occurs when atherosclerotic lesions form in the walls of capillaries. The perfusion changes observed by Lind et al. were mainly as a result of microvasculature damage. It is not yet established whether such changes have the potency of leading to myocardial infarction. The researchers were unable to determine how perfusion defects develop over time after radiation therapy. However, they noted that the defects increased after 12 months. However, the difference between the increase and the time- points 6 months after radiation therapy was not statistically significant.
When the researchers compared the two methods, they found that they complemented each other with regard to earlier results attained using the qualitative method alone. The two methods had a similar directional trend with regard to tracking SPECT changes after radiation therapy for the first six months. The quantitative method was regarded as more objective and more reproducible than the semi- quantitative method. The method was especially useful in tracking changes when the same patient was used in two studies.
Lind et al. managed to demonstrate that the volume of the left ventricle that was irradiated significantly influenced SPECT changes after radiation therapy. They noted that such changes corresponded to the radiation portals. Moreover, the intake of tamoxifen and hypercholesterolemia were two factors that seemed to influence perfusion changes.
Effects of Radiotherapy: RT Parameters and Cardiac Abnormalities
One way to evaluate the effects of radiation therapy on the heart among NSLCL patients is to study the results of cardiac diagnostic tests. As aforementioned, it is known that radiation therapy can lead to perfusion changes among NSCLC and breast cancer patients. When the dosimetry plans of patients are evaluated, it is quite clear that abnormal cardiac results depend on the dose of radiation. It is also noted that the results are sensitive to radiation therapy parameters. The long- term consequences of the abnormalities in cardiac tests that indicate early damage of the heart tissue are unclear. However, it is possible to avoid adverse consequences by modifying radiation therapy parameters. Correa et al. conducted a study and documented findings on how radiation therapy had affected the cardiac functionality among left sided breast cancer patients. They sought to assess the relationship between radiation therapy parameters and cardiac diagnoses of CAD. In addition, they sought to analyze the relationship between congestive heart failure and myocardial infarction among the patients tested.
The retrospective study used the records of 599 women who had visited and received treatment from the Hospital of Pennsylvania University from 1977 to 1995. Several exclusion criteria were used in selecting participants. For example, the investigators excluded from the study patients who were on a follow- up regimen for a period of less than two years, patients with preexisting heart ailments, and those who had received irradiation on the internal mammary node. Out of the original 599 patients, 416 were selected to participate in the study. Their mean follow- up time was 12.6 years while the median was 12 years.
As noted earlier, SPECT is a method that is commonly used in detecting congestive heart failure, myocardial perfusion, and CAD among patients with symptoms of heart disease, such as chest pains. When SPECT stress myocardial perfusion imaging is used to detect CAD among women, the method is shown to have a specificity of 71% and a sensitivity of 77%. On the other hand, SPECT stress echocardiography has a specificity of 60% and a sensitivity of 82%. The patients who were taken through cardiac testing were treated with a 60- 66 Gy total radiation dose. Twenty one patients were chosen and put in the control group. They were offered similar tangential radiation therapy, but were not offered cardiac testing. In addition, patients in the control group did not have symptoms of cardiovascular disease. They had a median follow- up of 12 years. All the radiation treatment plans were formulated before the introduction of 3D- conformal radiation therapy.
The investigators retrieved the results of hormonal therapies, chemotherapies, cardiac diagnoses, and blood tests that the patients had undergone in the past from records. Correa et al. used the Framingham model to determine the absolute risk of developing CAD among patients over a period of ten years after radiation therapy. The model incorporates risk factors like age, lipoprotein cholesterol, total cholesterol, smoking, diabetes status, and blood pressure. The model is accepted as a conventional measure of cardiovascular risk. However, it does not take into account various risk factors, such as obesity, physical inactivity, and the cardiovascular history of a family. Moreover, the model does not present a direct correlation between the predicted risk and the rate of event in the population under observation.
Correa et al. used the students’ t-test to compare the results. The analysis involved continuous variables and the chi- square test for discrete variables. The researchers used logistic retrogression to test the relationship between radiotherapy treatment parameters, test abnormalities, and cardiac diagnoses.
Sixty four patients out of the total 416 patients had received 84 diagnostic heart studies at a median time of 12 years after receiving radiation therapy. Forty six tests were echocardiograms while 38 were myocardial perfusion. Twenty two patients had undergone both echocardiography and myocardial perfusion imaging. The investigators found that there were consistencies between the two tests among twenty patients while both of them had inconsistencies in two patients.
Out of the 62 patients, 20 had chest pains, 17 had CAD evaluations, 12 had shortness of breath, and 9 had palpitations. The study indications of 4 patients were not known. Correa et al. (77) found that there was no difference between the test indications of patients with normal results and those with abnormal results. The characteristics of the patients at the time they underwent diagnosis and subsequent hormonal and chemotherapy regimens are tabulated below:
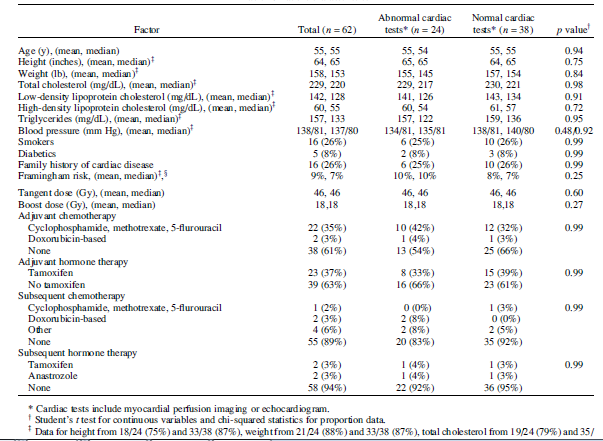
With regard to heart risk factors at the time the patients were undergoing radiation therapy, the patients who had normal cardiac study and those who had abnormal cardiac study were similar in age, weight, height, lipoprotein cholesterol, total cholesterol, cardiovascular disease family history, triglycerides, incidence of diabetes, and smoking status. Sixty two patients out of the total 416 and who had received treatment for breast cancer on the left side had also received diagnostic testing of the heart. It was found that 24 out of the 62 had abnormal results. Twenty one out of 38 of those who were tested had SPECT perfusion defects while 11 out of 46 had motion abnormalities of the regional wall after echocardiography. When the Framingham model was applied to the patients at the time they were receiving radiation therapy, the mean estimated cardiac risk was 9% for the group of 62 patients who were tested.
The mean risk of developing CAD over a period of ten years for the normal testing group was 8% while that of the abnormal testing group was 10%. In spite of the fact that the cardiac risk was predicted as quite low at baseline, the incidences of abnormalities of cardiac testing were very high. The actual cardiac risk was 39% while the predicted risk was 9%. As a result of this, the difference between the two cannot be ignored (p<0.001). Twenty one out of 24 abnormalities were in the LAD territory and two in the LEX territory.
Matzinger et al. demonstrated that maximum heart length and width, as well as the central lung-distance are parameters with a positive correlation with the volume of the heart that is irradiated. The two parameters were obtained for all the patients who were involved in the study. When the median central lung-distances for the patients who had abnormalities in the cardiac tests were compared with those of patients with normal tests, there was a significant difference. The patients whose cardiac tests had abnormalities had a 1.9- 3.6 cm central lung- distance range while the corresponding range for their counterparts was 1.2- 3.1 cm. When maximal heart lengths and widths were compared between the groups, the difference obtained was not statistically significant.
When the group of 24 patients with abnormalities in their cardiac tests was compared to the group of 21 patients who were used as controls, the maximum heart width for the 24 patients was significantly larger than that of the controls. The investigators also observed a trend that was tending towards significance in the difference between the central lung distances among the two groups. The researchers did not find a significant difference between the maximum heart length of the group with abnormal cardiac tests and the control group.
Correa et al. also investigated the relationship between radiotherapy parameters and the development of congestive heart failure, myocardial infarction, and CAD among the 62 patients who had undergone cardiac tests. Forty percent of the patients had developed CAD, 26 percent developed myocardial infarction, and 23 percent developed congestive heart failure. The investigators determined that the median central lung distance for the 14 patients with congestive heart failure was larger compared to that of the 48 patients who had not developed the condition. When the patients who had CAD were compared with those who did not have the disease, the former were found to have a significantly larger median central lung distance, maximum heart width and length. In the same manner, myocardial infarction patients had larger radiation therapy parameters than those who did not have the disease.
Correa et al. managed to demonstrate that the incidence of cardiac diagnostic tests abnormalities among women with left- sided breast cancer was higher than expected from the cardiovascular risk profiles of the patients. The abnormalities were anteriorly located, thus corresponding to the part of the heart that was irradiated during radiation therapy. Moreover, the cardiac diagnostic tests abnormalities and development of congestive heart failure and CAD were correlated to potentially modifiable radiation therapy parameters. When compared to the study that was conducted by Matzinger et al., the percentage of symptomatic patients who had abnormal cardiac tests in this particular study was high (39%). However, Matzinger et al. had found a higher percentage of abnormal cardiac tests among asymptomatic breast cancer patients who had received tangential radiation therapy. After seven years of follow up, Ring et al. showed that 17 out of 24 patients had myocardial perfusion defects. Eight out of the 24 also had motion abnormalities of the regional wall. In one year of follow up, perfusion defects had developed in six out of twelve left sided breast cancer patients with early disease.
In the study that was conducted by Correa et al., 88% of abnormal cardiac tests involved the LAD territory. Vikström et al. also determined that there is a positive correlation between the LAD irradiated volume and radiation therapy parameters. Correa et al. found that the radiation dose that is delivered to the LAD strongly depends on the central lung distance, but the dose delivered to the other coronary vessels only had a minimal relationship with the central lung distance. They found that when the central lung distance was increased from 1.86 to 2.86 cm, the volume of the LAD that was irradiated at 40 Gy increased by 35%.
The group with abnormalities in cardiac diagnostic tests represented persons whose hearts were irradiated at relatively high doses than the others because of the 2.6 cm median central lung distance. In their study, the patients who had larger central lung distances had more cardiac tests’ abnormalities. As a result, they had higher chances of having larger volumes of their hearts irradiated. In the retrospective study that was conducted by Ring et al., there was a relationship between radiation therapy parameters and the development of perfusion defects. They compared the SPECT images of left sided breast cancer before receiving radiation therapy and 6 months later. They found that out of the twenty patients who had received irradiation, 12 of them developed new myocardial perfusion defects. The perfusion changes were minimal in the myocardial regions that were irradiated at between 0 and 10 Gy.
However, the regions that were irradiated at more than 41 Gy were found to have a 20% increase of perfusion defects. Vikström et al. conducted a clinical investigation and determined that the perfusion defects on the LAD territory, 18 months after radiation therapy, had an independent association with the volume of the left ventricle that was irradiated. In addition to reporting that there were persistent perfusion changes among patients who were irradiated at 45 Gy between 18 and 24 months after radiotherapy, the researchers pointed out that patients developed new perfusion defects in the long- term, between three and six years.
Correa et al. also demonstrated that there is a relationship between the central lung distance and congestive heart failure and CAD. Although the underlying mechanism that governs such observations is not yet known, some studies have linked radiation therapy parameters with cardiac morbidity and mortality. Vikström et al. investigated the impact of maximum heart distance on radiation induced heart disease. However, they did not find a direct relationship between increased maximum heart distance and increased cardiac morbidity. Nevertheless, they observed that patients whose maximum heart distances were larger than 3 cm had a higher risk of developing ischemic cardiac disease than patients in other categories. The main reason why a significant trend may not have been established is that the sample size was quite small.
The differences between the findings of Correa et al. and those made by Vikström et al. are due to the fact that the risk factors among the two populations were different. For example, in the Correa et al. study, all patients had cardiovascular disease symptoms. More than half of these patients had elevated levels of cholesterol, while 25% of them were smokers. In the Vikström et al. study, only 14% of the patients had hypercholesterolemia while 9% were smokers. The median maximum heart distance in the Correa et al. study was 1.8cm while in the Vikström et al study, it was 1.3cm.
When modern radiation therapy techniques are used, the risk of developing radiation induced cardiac illness is not certain. However, Matzinger et al. found that the volume of the heart that was irradiated among 6 percent of all the patients who received radiation therapy with modern megavoltage tangents was high enough to result to ischemic heart disease.
Radiotherapy Effects: Tomotherapy and Radiation Induced Pneumonitis
Helical tomotherapy is a modern IMRT technique that was mainly developed for the purpose of dose escalation and reduction of radiation induced lung injury. The IMRT dose distribution to the lung and other surrounding tissues and organs is quite complex when compared to conventional radiotherapy. In this regard, there is a possibility that the pattern of lung injuries sustained after tomotherapy is quite different from that seen after conventional radiotherapy. Park et al. conducted a study to determine the pattern of tomotherapy induced pneumonitis among NSCLC patients. The study was aimed at determining how tomotherapy affected patients three months after completing treatment. The thirty five patients who were included in the study were treated using tomotherapy between 2005 and 2007.
Twelve of them had primary NSCLC while the rest received treatment for metastatic disease. Four patients were later excluded from the study due to peripheral atelectasis, which made it difficult to interpret CT results of radiation induced pneumonitis. The remaining thirty one patients had simulation CT scans before commencing treatment. After treatment, 25 of them underwent CT examinations two times within the first three months. The patients were scheduled to receive other CT scans in two months intervals for one year. One oncologist and two radiologists determined the diagnosis of radiation pneumonitis among the patients.
Twenty one patients with 67 targets were the first to receive CT examination one month after radiotherapy. Thirteen patients had changes in the lung in 34 targets within three months after treatment, while 8 patients had changes in 14 targets within the first month of radiotherapy. Five patients were offered steroid therapy while the rest did not have symptoms of radiation pneumonitis within the first three months of tomotherapy.
Over the past decade, various techniques were designed to increase tumor dose and reduce irradiation of normal tissues. Helical tomotherapy is designed in such a way that set-up errors are identified with ease and corrected on time. It also makes it possible to modify treatment depending on information gathered from MV CT images. Consequently, tomotherapy is reported to have the capacity to reduce lung injury and to enhance the local control of lesions.
Radiation induced lung injury is mainly caused by the irradiation of the lung tissue at a radiation of 40 Gy or more. Studies have found that radiologic manifestations in the normal lung are quite rare when the tissue is irradiated at a dose lower than 20 Gy. Park et al. found that the CT findings of radiation pneumonitis were most common at the ground glass opacities’ focal area. The findings were very similar to radiation pneumonitis that is induced by conventional radiation therapy. However, the ground glass opacity distribution in relation to the PTV was quite different from that of conventional radiotherapy. They found that radiation pneumonitis occurred at the periphery of the PTV. They also observed that radiation pneumonitis was more pronounced in the regions that received low radiation dose than those in the regions that were irradiated at higher doses. The resulting centrifugal pattern was off- center in relation to the PTV.
The findings made by Park et al. were similar to those made by Gillham et al.. The latter sought to determine the pattern of radiation pneumonitis when other modern techniques, with the exception of tomotherapy, were used in the treatment of NSCLC. They established that radiation pneumonitis did not occur in relation to the dose, but rather as ground glass opacities. The observation is attributed to the complex arrangement of beams in these techniques. Because these techniques are quite related to tomotherapy, it suffices to note that tomotherapy induced radiation pneumonitis does not correspond to PTV. It does not correspond in spite of the fact that the technique is used to deliver high doses of radiation.
The beam that delivers radiation in tomotherapy is longer than the one used in conventional and conformal radiotherapy. In this case, the tomotherapy low dose area is larger than in the other techniques because of increased leakage and scatter. Additionally, there is an increased chance of double exposure at the regions that are in the periphery of the PTV. Consequently, the regions that are exposed to lower doses in tomotherapy are larger and irregular and the regions that receive high doses are concentrated around the target. The heterogeneous distribution of irradiation dose leads to a radiation pneumonitis pattern that is not in congruence with the PTV. Currently, there is need for more research on the biological changes that follow radiation pneumonitis in the areas that are exposed to the low dose.
The number of patients in the Park et al. study was quite small to come up with conclusive inferences. Furthermore, they excluded other factors that impact on the development and progression of radiation pneumonitis, such as age, preexisting lung disease, radiation techniques, and chemotherapy history. Additionally, their conclusions were based on observations they made in three months, which is a relatively short period of time. However, it is reasonable to agree that there is a difference between the radiation pneumonitis that is induced by tomotherapy and the one induced by other techniques. The finding that the distribution of radiation pneumonitis is different when tomotherapy is used is very helpful in preventing misdiagnosis. Additionally, it would help physicians to avoid using unnecessary procedures when patients who have received tomotherapy thoracic irradiation pay follow- up visits.
Radiotherapy Effects: Pneumonitis and Fibrosis
There is irrefutable evidence suggesting that high doses of radiation could be safely delivered to enhance the local control of NSCLC. Kong et al. conducted a study that compared the effects and benefits of continuously increasing radiation from 40 Gy to 50 Gy. They managed to demonstrate that NSCLC was effectively controlled when the radiation dose was set at 60 Gy. Retrospective studies are implying that if the dose is safely increased beyond 60 Gy, local control of the disease would also improve. At the end of the day, the overall rate of survival among patients will also increase.
High dose radiation therapy is not used on a routine basis in practice because of toxicity concerns. In addition to cardiac complications, lung toxicities are the leading source of this concern. Radiation pneumonitis develops in approximately 30 percent of all patients who receive thoracic irradiation . As such, it is one of the most dose- limiting toxicities associated with the use of radiation therapy in the treatment of NSCLC. Therefore, coming up with a strategy to deliver high dose of radiation during the treatment of NSCLC goes a long way in improving the patients’ therapeutic ratio. Kong et al. hypothesized that it would be possible to safely deliver radiation doses of more than 66 Gy using 3D conformal techniques.
They conducted a clinical trial to determine the highest dose of radiation that could be used for the treatment of NSCLC with only a small volume of the heart irradiated. They documented the final late and acute toxicity results for the purpose of investigating the relationship between dose and volume with relation to lung toxicity. They also sought to identify the predictors of radiation fibrosis and pneumonitis.
The patients who were involved in this study had either recurrent or newly diagnosed stage I to stage III NSCLC. In addition, the patients had not received any earlier thoracic radiation. Their ECOG performance status was also taken into consideration. The study did not emphasize on the extent of pulmonary compromise or weight loss. The first group of patients who were treated between 1992 and 1997 received radiation therapy only. Between 1997 and 2000, patients suffering from recurrent or stage III disease were offered neoadjuvant chemotherapy, which consisted of two cycles of vinorelbine and cisplatin. In addition to this, radiation therapy was administered from the 50th day of treatment. Some patients could not be treated with high doses of radiation after receiving chemotherapy. As a result of this, they were separated from the study group and treated using the standard radiation and fractionation.
From 1992 to 2000, 122 NSCLC patients were considered for the study. However, 13 patients were later excluded because of diverse reasons. Consequently, 109 patients were enrolled for the analysis. The median follow up duration for the patients was 9.2 years (110 months). All the 109 patients were followed- up for at least five years, except for one patient who died four and a half years after receiving radiation therapy. The table below shows the overall toxicity of the patients:

It was found that approximately one third of the patients had acute toxicity of grade 2 to grade 3. The most common complications were pulmonary fibrosis, pneumonitis, and esophagitis. Other toxicities included nausea, fatigue, skin reactions, pericardial effusion, bronchial stenosis, and rib fractures. Six patients succumbed to hemoptysis and pleural effusion, but it was not clear whether the complications were as a result of tumor progression or radiation therapy. The maximum- tolerance radiation dose was attained among patients who had lung Veff > 0.31. Eighty three patients were treated with more than 69.3 Gy of radiation in fractions of 2.1 Gy. None of the patients had grade 4 to 5 toxicities of the lung, but 14% developed grade 2 or 3 pneumonitis. On the other hand, 13.5% of the patients developed grade 2 or 3 fibrosis.
The median onset time for patients who developed grade 2 or 3 pneumonitis was 72 days from the time radiation therapy was initiated. When the investigators carried out univariate analysis, they found out that there was a significant association between NTCP, lung Veff, V13, V20, MLD (mean lung dose), total lung volume, primary GTV, and T stage on the one hand and pneumonitis on the other hand. However, other factors, such as neoadjuvant chemotherapy administration, total tumor dose, tumor location, DLCO and FEV1 at the start of radiation therapy, pulmonary function tests, weight loss, performance status, gender, and the age at which radiotherapy was started, did not have a significant relationship with pneumonitis.
The scholars found that 74% of the patients who had grade 2 to 3 fibrosis also had symptomatic pneumonitis (grade 2 to 3), while 26% had pneumonitis of grade 0 to 1. The median time for the diagnosis of fibrosis was 8 months from the time the patients received radiation therapy. As opposed to the findings made in pneumonitis, the researchers found that there was a relationship between fibrosis and gender. Women were found to be at a higher risk of developing fibrosis than men. But there was no significant relationship between fibrosis and V13 or GTV. Like in the case of pneumonitis, univariate analyses revealed a significant correlation between fibrosis on the one hand and V20, NTCP, and MLD on the other hand.
In general, 20% of all the patients had symptomatic fibrosis or pneumonitis. Univariate analysis revealed that gender, total lung volume, T stage, NTCP, lung Veff, V20, V13, and MLD were significantly related to lung toxicity. Kong et al. managed to demonstrate that when patients are followed up for a long time to determine toxicity, it is possible to safely use high doses of radiation (60 Gy to 66 Gy) for the treatment of NSCLC by the use of conformal techniques. For instance, despite that 76% of the patients were treated with a radiation dose of more than 69.3 Gy, none of them developed either pneumonitis or fibrosis of grade 4 or 5. Furthermore, there was a relationship between the occurrence of symptomatic lung toxicity and the tumor radiation dose on the one hand and such dosimetric factors of the lung as V13, V20, lung NTCP, and MLD on the other hand.
Although the traditional belief is that radiation lung toxicity of grade 2 to 3 is highly correlated to the prescribed dose, Kong et al. did not find such a relationship. The belief that toxicity is linked to the total dose has its origin on the irradiation of the whole organ. It is established that when the entire lung is irradiated, the total dose tolerance reduces sharply when 26 Gy of radiation is delivered in 20 fractions. For instance, Chi et al. found that when the lung is irradiated uniformly using 2D treatment planning, lung toxicity increased when the dose was increased from 40 Gy to 60 Gy. However, when 3D irradiation techniques are used, the correlation between lung tolerance and the prescribed tumor dose is easily predictable because of non- uniform irradiation of the lung.
The observation is made since the dose is highly concentrated on the region adjacent to the tumor. What this implies is that when 3D techniques are used, delivery of the dose is improved. The dose applied on the tumor does not correspond to that applied on adjacent healthy tissues. In this regard, patients who are on a similar prescribed treatment dose have different volumes of irradiated normal lung depending on the size of the tumor, beam arrangement, and tumor location. Kong et al. concluded that the total irradiation dose is not directly linked to pneumonitis. The observation is in agreement with that made by Bertelsen et al.. However, they also demonstrated that distribution of radiation dose in the uninfected lung and maximum dose prescribed is assessed based on the relationship between dose and volume as opposed to tumor dose, regardless of the lung’s dosimetry.
In the study conducted by Kong and colleagues, the patients who had smaller volumes of irradiated lung were treated using higher radiation doses than the other patients. The different doses imply that in the determination of toxicity, the volume of the lung that is irradiated is more important than the tumor dose. The observation explains why both fibrosis and pneumonitis had a significant association with volumetric factors, such as V20, V13 (percentages of the lung receiving 20 Gy and 13 Gy respectively), total lung volume, and primary tumor volume. The significance of the lung and tumor volumes is evident because of their correlation with the volume of the lung that was irradiated. However, after taking into consideration the lung- dosimetric factors, the lung and tumor volumes became insignificant.
The findings from the study significantly contribute to the findings made in other studies that point out the independent relationship between dosimetric factors like MLD, V13, and V20 and radiation pneumonitis risk. In addition to integrating the impacts of the lung volume dose distribution, MLD seems to provide a better description of toxicity when conformal treatments are used. Despite that V20 is the most common parameter used in many clinical investigations compared to other parameters, its use is mired by controversies. Controversies are evident when it comes to the question of exactly how V20 is related to pneumonitis of grade 3 and beyond.
Bertelsen et al. reported 8% for 20% to 30% V20 patients, while Ramella et al. documented 50% for a 25% to 30% V20. The outcome is accommodated because V20 varies with the shape of the dose- volume histogram (herein referred to as DVH), which is dependent on the arrangement of beams in various institutions. Kong et al. found that MLD was significantly related to the incidence of symptomatic fibrosis and pneumonitis. However, it is important to note that statistical significance is not an automatic prediction of toxicity. In addition, the investigators found that the predictive ability of MLD, V20, and V13 for clinically significant lung toxicity was similar.
In spite of this, it is important to note that the findings documented by Kong et al. are limited by the patients who had received chemotherapy and number of toxicity events. As a result of this, the findings and conclusions made were limited to the population that was studied and the dose prescription method. The study demonstrated a lung- volume-dose-lung toxicity relationship that may not be directly used in practice because the point- dosimetric factors heavily depend on the shape of the DVH. Kong et al. pointed out that high radiation doses should be used with the inclusion of a limited lung volume.
The researchers studied the toxicities of fibrosis and pneumonitis, combined and separately. The separate analysis was performed because fibrosis differs from pneumonitis with regard to molecular regulation, radiographic appearance, clinical presentation, and histopathologic presentation. The separate analysis was also important because fibrosis may not always be a pneumonitis sequel. As a result, it may have different predictive factors. For a long time, fibrosis was regarded as a radiographic finding that has a voxel level dose- dependent relationship.
Bertelsen et al. reported that the occurrence of fibrosis was dependent on volume and dose. It has a 30 Gy – 40 Gy threshold dose. Most of the studies that have included radiographic fibrosis have not found a clinical significance of the condition. There is a lack of literature on clinically significant radiographic fibrosis, but Kong et al. managed to draw a relationship between fibrosis and radiation pneumonitis. It is worth noting that grade 2 and higher fibrosis was far less predictable in the study as compared to pneumonitis. Despite that there was a very significant relationship between V13 and pneumonitis, such a correlation was nonexistent in the case of fibrosis. Ramella et al. noted that the functional capacity and volume of the lung may have a relationship with fibrosis symptoms. However, the scholars did not present any reasons or justifications for such observations. More studies are needed in the future in this field. Such studies should include more patients than the current studies, as well as make use of multiple dosimetry and reserve variables. That way, the studies will effectively ascertain such a predictive ability.
Lastly, from the findings made by Kong et al., it is noted that the practice of using only a 60 Gy dose for the treatment of NSCLC is rather conservative, especially when conformal techniques are used. Although the appearance of lung toxicity of grade 2 and beyond is regarded as clinically significant given that it may affect the QOL of patients, grade 1 lung complications, which have very little clinical significance, are more common than such complications. For most NSCLC patients who receive radiation therapy, the main challenge is locoregional recurrence and failure. As more studies continue to indicate that the use of higher doses is effective in the treatment of NSCLC, there should be a consideration of the traditional use of 60 Gy radiation dose.
Radiation Therapy Effects: Pneumonitis Diagnosis Challenges
The lung injury caused by radiation therapy is one of the main reasons why it is not possible to increase the total radiation dose in the treatment of NSCLC patients. The dose cannot be increased even in the days of conformal therapy. As noted earlier in the study, between 5 and 30 percent of all patients who receive thoracic irradiation experience radiation- induced lung injury. Acute symptoms of lung injury occur between one and six months after radiotherapy. The symptoms that characterize radiation pneumonitis include coughing, shortness of breath, and mild fever. In most patients, especially those who have been diagnosed with NSCLC, the symptoms are not very specific. As a result, it becomes quite hard to diagnose radiation- induced pneumonitis. There are other conditions that have similar clinical presentation. There is no formal evaluation for scoring pneumonitis.
Kocak et al. conducted a study to examine the difficulty of coming up with a clinical diagnosis for radiation pneumonitis. The study was conducted from 1991 to 2003. It involved 251 NSCLC patients who were on a follow- up program for at least six months. After radiation therapy, clinical evaluation was conducted to determine the symptoms of radiation induced pneumonitis. The physicians who conducted the study reviewed records of all NSCLC patients who were diagnosed with grade 2 or higher radiation induced pneumonitis. They classified the patients as either ‘hard to score’ or ‘classic’. Patients who were categorized as having classic pneumonitis had shortness of breath and they were treated using steroids. Such patients did not present other clinical factors like tumor regrowth or cardiac disease. A patient was classified as having ‘hard to score’ pneumonitis depending on whether they presented other complications in addition to shortness of breath or not. They were also treated using steroids. While some patient responded to the treatment, others did not.
All the patients were treated using 3D radiation therapy. Forty seven of the patients had a very high shortness of breath, which was consistent with pneumonitis. The patients were treated using steroids. Thirty one of those who had shortness of breath were classified as having classic pneumonitis. Thirteen of the forty seven had other confounding complications, such as chronic obstructive pulmonary disease (herein referred to as COPD), congestive heart failure, or tumor progression and regrowth. Three other patients had developed bronchial stenosis in addition to having shortness of breath. The researchers found that the ‘hard to score’ patients had a higher COPD rate than the ‘classic’ patients. The observation reflected the fact that preexisting COPD is a confounding factor for pneumonitis diagnosis.
Many researchers have endeavored to come up with methods that relate clinical and dosimetric parameters to radiation induced pneumonitis. They have demonstrated that the risk of pneumonitis is directly proportional to the volume/parameters/increasing dose. Nevertheless, the findings that most of them have documented as they attempt to demonstrate the correlation are suboptimal. For instance, in the study that was conducted by Ramella et al. patients whose V20 was greater than 40% had a radiation pneumonitis rate of 36%. However, the V20 of close to half of those patients who developed pneumonitis was lower than that. In this regard, the sensitivity for V20 that is greater than 40% was approximately 48%. In another study that was conducted by Yirmibesoglu et al., the sensitivity and accuracy of all the DVH classes was poor. In this regard, the scholars came to the conclusion that the most accurate and ideal DVH metric is not yet identified. Consequently, it is important to expand the predictive models so that they can include biological, clinical, and dosimetric parameters.
One of the main difficulties that investigators face in attempts to come up with additional biological, dosimetric, and clinical perimeters is the quality of endpoint data. In the study conducted by Kocak et al., twenty eight percent of the patients had other clinical factors, thus making the scoring of injury very imprecise. Such endpoint impressions are very important and should be put into consideration in the construction of predicting models. There is virtually no conventional method that is well established to provide accurate information on toxicity scores. For example, Kocak and colleagues used the review of physicians to identify ‘hard to score’ patients. Such a criterion is subject to a lot of criticism. Nonetheless, the methods were still reasonable to some extent. A prospective evaluation was conducted for all the patients who were included in the study. As a result, the opinions of the physicians who provided treatment were effectively documented.
The uncertainty riding on the scoring of pneumonitis has a significant effect on studies that are meant to test models. The predictive models, which are constructed on the basis of dosimetric parameters alone, are regarded as quite effective when the patients whose pre- radiation therapy pulmonary function is very poor are excluded. Ramella et al. pointed out that when such patients are not included in studies that are meant to test predictive models, the V30 and NTCP models have a high correlation with the outcomes of the remaining patients. They also pointed out that SPECT models have a better prediction of pneumonitis among patients with a DLCO of more than 40% before radiation therapy. Patients with very low pre- radiation therapy DLCO and FEV1 have a higher probability of developing pulmonary symptoms that are not essentially caused by radiotherapy. They also indicated that the NTCP model has a positive relationship with incidences of radiation pneumonitis among Hodgkin’s patients than among lung cancer patients.
Most physicians traditionally diagnose radiation pneumonitis using an exclusion method, where they first rule out other etiologies. Such a differential diagnosis includes lymphangitic tumor spread or local recurrence, respiratory infection, drug toxicity, cardiac disease, and pulmonary emboli. In the study conducted by Kocak et al., different patients developed symptoms at varied times after radiotherapy. Because of the small number of such events, it was not possible for the researchers to carry out a comparative analysis between the ‘classic’ intervals and ‘hard to score’ intervals. The symptoms of radiation pneumonitis are very similar to those of pneumonia. Among patients with a COPD history, respiratory infection results in exacerbation of lung disease. Many COPD exacerbations are as a result of environmental factors like temperature and air pollution, as well as respiratory infections.
In the study that was conducted by Kocak et al., 50% of the patients categorized as ‘hard to score’ had at least one respiratory infection. There is a typical association between infection and positive cultures and high fever. Symptoms that are caused by the progression or recurrence of tumors are particularly challenging among NSCLC patients. In most cases, when the diagnosis is neoplasm in nature, there is an interval of more than four months between radiotherapy and clinical presentation, presence of associated hemoptysis, and metastatic disease. Kocak et al. concluded that it was difficult to score radiation pneumonitis among 28 percent of the patients in the series because of the presentation of confounding conditions.
Radiation Therapy Effects: Pneumonitis Grade ≥ 3 Predictors
Various investigators have pointed out that the outcomes of SBRT for early NSCLC are largely comparable to those of surgery. In order to improve the safety of SBRT procedures, it is important to establish the factors that cause severe radiation pneumonitis. Takeda et al. conducted a study to determine the factors that are linked to grade ≥3 radiation pneumonitis after NSCLC patients were treated with SBRT.
The retrospective study gathered information from NSCLC patients who were followed- up for at least six month and who had ≥ 1 radiation pneumonitis. The study included 133 subjects who received treatment from February 2005 to February 2009. One hundred and eleven patients had primary tumors while 22 had metastatic tumors. All patients underwent pulmonary function tests before radiation therapy. The patients were treated with a total dose of 50 Gy that was delivered in 5 to 10 fractions. After receiving treatment, the patients were followed-up on a monthly basis to monitor the appearance of radiation pneumonitis through X- ray examinations. The follow- ups continued for at least six months to allow for the stabilization of the clinical findings. In addition to this, the patients were examined every three months using CT scans after SBRT.
The researchers investigated various factors to determine whether or not they were associated with the development of radiation pneumonitis. The factors included age, sex, operability, disease, pulmonary comorbidity, performance status, laboratory results, total dose, and pulmonary function tests. The post- treatment, dosimetric, and clinical factors were assessed for correlation with radiation pneumonitis risk of grade ≥ 3. Among the patients included in the study, 36 developed grade 0 disease, 69 had grade 1, 21 had grade 2, while 7 had grade 3. None of the patients treated using SBRT developed grade ≥ 4 radiation pneumonitis. Five of the patients were offered treatment twice due to metachronous metastases. However, such patients did not develop a condition that was more than grade 3. For the patients who were diagnosed with grade 2 and grade-3 pneumonitis, symptoms appeared simultaneously or subsequently to graphical appearance.
Four out of the seven patients who had grade 3 pneumonitis were treated using steroids. The symptoms were resolved after treatment. One patient who was 80 years did not receive any treatment, but was closely followed- up by a physician. Two other patients who were not offered steroid treatment had developed severe COPD and received oxygen therapy from home. With regard to the extent of graphical radiation pneumonitis, four patients had a high degree of graphical pneumonitis beyond the region that was irradiated with a high dose. Two of the patients had IPF and three of the four (including one with IPF) were offered steroid therapy. For the rest of the patients, graphical radiation pneumonitis was in correspondence with the region that had received high dose radiation. The table below shows how various factors are associated with radiation pneumonitis:
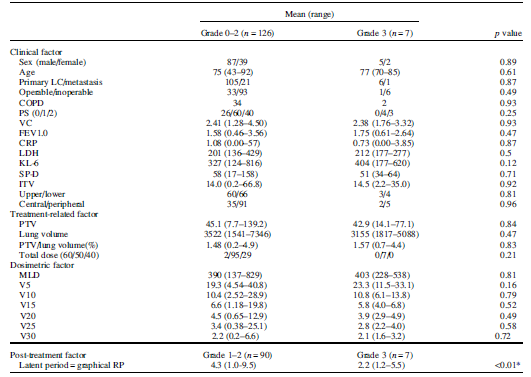
The investigators also determined that when the latent period of radiation pneumonitis was short, the graphical appearance occurred early. One explanation for this is because graphical appearance occurred first among all patients who had grade 2 or 3 radiation pneumonitis. They determined that the risk for grade 3 radiation pneumonitis was 75 percent when graphical pneumonitis occurred a month after radiation therapy and 40 percent when it occurred within two months of radiotherapy. Only one patient developed grade 3 pneumonitis three months after SBRT. Thus, the grade 3 radiation pneumonitis beyond two months was 1.2 percent. Various researchers have analyzed the factors that correlate with severe radiation pneumonitis. Some of the factors are patient- specific, others are treatment- specific, while others are dosimetric.
Ramella et al. conducted a prospective study that included 70 NSCLC patients who were treated with a total radiation of 40 Gy. The aim of the study was to determine the risks that are linked to radiation- induced changes. According to the researchers, mean lung dose (V7 and V10) were predictors of lung toxicity. But the researchers did not find any other factor that was significantly associated with radiation toxicity. They determined that the upper region of the lung was more tolerant to radiation than the lower region. Ramella et al. studied perifocal changes that took place in the lungs after SBRT.
On the other hand, Huang et al. studied the dosimetric and clinical factors of radiation pneumonitis that called for the use of steroids after conventional radiation therapy. Their study was carried out using the medical records of 385 patients who had stage I NSCLC. They did not find any predictive factors. Likewise, Takeda et al. did not find any correlation between the various dosimetric and clinical factors on the one hand and the risk of radiation pneumonitis before the administration of radiation therapy on the other hand. The only factor that had a significant correlation with the risk of radiation pneumonitis of grade ≥ 3 was graphical appearance in the first one month.
However, it is essential to note that SBRT is still under development and the number of patients who are offered radiotherapy using the method is still very limited. Moreover, the follow up period for such patients is shorter in comparison to other radiation therapy techniques. In addition, the dosimetric and clinical factors that are correlated with radiation pneumonitis after conventional radiation therapy are quite inconsistent in diverse investigations. In the same manner, risk factors related to grade 3 radiation pneumonitis are regarded as inconsistent for both SBRT and other radiotherapy techniques. In this regard, it becomes important to pay attention to risk graphical appearance and other risk factors outlined by other investigators of radiation therapy.
Huang et al. conducted a retrospective study that included 385 NSCLC patients who were irradiated with a 60 Gy to 70 Gy radiation dose. They endeavored to determine the lung injuries that are suffered by such patients after treatment. The cases in the study were divided into three. The first group of 307 patients was very stable and did not require corticosteroids. The second group of 64 patients attained stability after steroid therapy. The third group of 14 patients succumbed to complications despite the administration of steroids.
Ramella et al. conducted a study to determine prognostic factors among 31 NSCLC patients who had severe radiation pneumonitis. They established that the extent of radiation therapy, whether in field or out of field, had an independent association with the survival of patients. They also pointed out that latent period among patients with out of field radiation pneumonitis was significantly shorter than among in- field patients. The observation implies that pulmonary injury among patients with out of field radiation pneumonitis was more severe compared to that among patients with in-field. The injury was associated with a rapid onset of symptoms.
It is believed that disease process leading to out- of -field radiation pneumonitis differs pathophysiologically with that of classic radiation pneumonitis. Some specialists have suggested that in the case of radiation pneumonitis, the damage to lung tissue is caused by hyperactivity of the immune system. As the inflammatory reaction spreads from the field of radiation, it impairs the process of gaseous exchange.
When SBRT is used to treat NSCLC patients, PTV graphical changes take place between two and six months after therapy. In the study conducted by Takeda and colleagues, graphical changes took place within two months, with the exception of one patient who had grade 3 radiation pneumonitis. Takeda et al. did not establish a significant relationship between comorbidities, such as other diseases of the lung, COPD, and IPF, and radiation pneumonitis of grade ≥ 3. However, careful observation should be given to patients who have pulmonary comorbidities. For example, out of the seven patients with radiation pneumonitis of grade 3, two had severe COPD. The two patients were taken through oxygen therapy from home, but they were not given steroids because they only had graphical radiation pneumonitis in and around the PTV. In such a case, it is quite difficult to differentiate between COPD’s natural progression and grade-3 radiation pneumonitis. In this regard, it is expedient to check the pulmonary function of the patient before deciding on SBRT indication.
Moreover, out of the seven patients with grade 3 radiation pneumonitis, two of them had IPF. The two patients also showed grade 3 radiation pneumonitis with extensive graphical radiation pneumonitis. Ramella et al. reported that patients who have IPF have a 25 percent acute exacerbation frequency. The development is the reason why IPF is regarded as a contraindication of radiation therapy. Studies have often indicated that SBRT is associated with IPF patients. However, the therapy is bedeviled by many controversies.
Radiotherapy Effects: Patient- Specific Characteristics for Lung Toxicity
As aforementioned, there are many studies already conducted to determine the predictive factors for severe dyspnea and radiation pneumonitis. However, the findings of the studies differ from one to the other, and sometimes they even contradict. Among the various reasons proffered to explain the disparity in findings is the lack of a standard measure for scoring toxicity. In addition to there being different scoring systems, there are different grades used in assessing outcomes .
Researchers have identified various dosimetric parameters that are correlated with radiation induced lung toxicity. There are three approaches that use DVH information in the calculation of these parameters. The three include the Vdose, MLD, and NCTP. One particular review found that the three approaches were related to the risk of lung injury, but investigators have not determined which of the three DVH approaches is superior. In spite of the fact that the approaches are associated with radiation induced lung injury, their predictive power is low considering the range of radiation dose used for treatment. It is believed that models using more than one parameter, in addition to including patient specific characteristics, have better outcomes. However, the exact combination of dosimetric parameters- predictive factors that should be used on a day to day clinical practice is not yet established.
Dehing-Oberije et al. conducted a study to determine the patient characteristics and dosimetric factors that are related to post- therapy dyspnea. They also evaluated the possibility of using the factors to come up with a predictive model for lung injury suffered after the administration of radiation therapy. The researchers used the records of NSCLC patients. The records were made between January 2002 and January 2007. All the patients included in the study did not receive elective nodal irradiation. They received irradiation for five days in a week.
Information from 42 patients was used in the study to determine the effectiveness of dose escalation. The total radiation offered to that group of patients was between 46.9 and 79.2 Gy. The radiation dose was delivered twice daily in a 1.8 Gy fraction. The two fractions were separated by 8 hours. Another group of 193 patients were treated according to the standard regimen that was in place up to August 2005. Stage I and II patients received a total dose of 70 Gy, while stage III patients received a total irradiation of 60 Gy subsequent to induction chemotherapy. The group of patients was irradiated once daily at 2 Gy.
The third group of 122 patients was treated according to the provisions of a new regimen. Patients in this group received a total radiation dose of between 54 and 79.2 Gy. They were irradiated twice daily at 1.8 Gy depending on spinal cord dose limitation or MLD. The two sessions of radiation therapy were separated by eight hours. Eleven patients received concurrent chemotherapy. The last group of 70 patients was treated using the standard regimen. They received a total dose of 45 Gy in two daily fractions of 1.5 Gy. They received a concurrent chemotherapy combination that was different from that of the fourth group.
Majority of the patients used in the study were male. In addition, the mean age of the entire population was 69 years. The performance status for most of the patients was between 0 and 1. By the time the treatment was starting, 41% of the patients were smokers. MLD was determined for 407 subjects and V20 for 270 patients. The mean MLD and V20 were 13.5 Gy and 21.0% respectively. Seventy six patients had grade 2 lung toxicity, 40 patients had grade 3, and 6 patients had either grade 4 or 5 toxicity. The scholars conducted a multivariate analysis to determine that the impacts of certain factors on the development of grade 2 or more lung toxicity after radiation therapy. The factors examined included gender, age, performance status, comorbidity, FEV1, smoking status, and equivalent radiation dose. In addition, the scholars examined other factors, such as weight loss, fractions given per day, chemotherapy, and MLD. They found that FEV1 was the strongest factor.
Dehing-Oberije et al. found that MLD and V20 are very limited as far as the dose range that is currently used for clinical purposes is concerned. Many studies have made efforts to determine the link between lung toxicity and dosimetric parameters. However, because the studies define the normal lung differently, it becomes difficult to conduct a comparative analysis of the studies and to establish the dose constraints that are applicable in practice. In spite of the fact that studies have not yet determined the strongest dosimetric parameter, there is a general consensus that the parameters are important in determining radiation induced lung injury.
At very high levels, such as those of MLD that is beyond 20 Gy and V20 that is greater than 35 percent, the incidence of radiation induced pneumonitis increases with an increase in dosimetric parameters. However, the contribution of such dosimetric levels in the range of radiation dose that is used clinically is rather small. Jun et al. outlined that there is a correlation between radiation pneumonitis and dosimetric factors when high radiation doses are used in radiation therapy. A sigmoid- shaped dose- outcome curve is used to model the correlation between the incidence of toxicity outcome and dosimetric parameters. The risk seems to increase rapidly when set at 20 Gy MLD or 35% V20.
However, the dose of radiation used in practice is less than these values. The difference explains why Dehing-Oberije and colleagues reported that dosimetric parameters lower than the above mentioned thresholds have only a mild influence. The observation also explains why the characteristics of patients and treatment related factors are useful for predicting severe dyspnea within the traditional range of radiation dose.
Some studies have pointed out that there is no correlation between the performance status of NSCLC patients and radiation induced severe dyspnea. However, there are others that point out a relationship between performance status of patients and development of radiation induced lung injury. In addition, conflicting results are evident in studies that endeavor to determine whether smoking has a relationship with radiation pneumonitis. When Tucker et al. analyzed data collected from the records of 580 patients, they found that the risk of developing radiation pneumonitis of grade 3 and beyond among patients who smoked was lower compared to that among other patients. Dehing-Oberije et al. also documented similar findings.
It is possible to explain the observation by the poor oxygenation of tissues since the binding capacity of hemoglobin for carbon monoxide is more than two hundred times that of oxygen. It was also found that hypoxia resists radiation induced cell death because the production of free radicals is lower than in other cases. As a result, less DNA is damaged. It is suggested that cigarette smoke activates an unfolded protein response, which protects the lung from the oxidant injury that is induced by radiation.
Different studies give conflicting results on whether or not the age of a person predicts radiation induced lung injury after radiation therapy. Some studies have reported a higher incidence of severe dyspnea among older patients than among younger patients. Other studies have not found such a correlation. Dehing-Oberije et al. determined that as an independent variable, age influenced the development of severe dyspnea among NSCLC patients after radiotherapy. Other studies have discussed the contribution of preexisting lung ailment to such developments. Some of the studies found that patients with COPD and impaired pulmonary function (as measured by FEV1 or DLCO) are more likely to develop radiation induced pneumonitis than the other patients.
However, there are other researchers who have found border line significance only. Still, others have found no significance at all. Dehing-Oberije et al. found that radiation therapy patients with low FEV1 measurements were likely to have severe dyspnea. It is important to note that one of the main limitations of the study conducted by Dehing-Oberije et al. was that the baseline FEV1 score for some patients was not available. In this regard, it is not possible to rule out that some patients, whose baseline pulmonary function was faulty, also had a low severe dyspnea score before radiotherapy.
Some studies have documented that the risk of lung injury associated with radiation therapy increases when chemotherapy is introduced. One of the reasons for such an observation is the use of many chemotherapy regimens. When chemotherapy is offered together with radiation therapy, the risk of developing lung injury is increased. However, there are other studies which have not found a relationship between the use of chemotherapy (sequential or concurrently) and radiation induced lung toxicity.
Dehing-Oberije et al. decided to measure the outcome of radiation therapy using severe dyspnea because clinical symptoms are enough to make an assessment. However, in this study, the scholars had no information on blood markers. Markers, such as TGF-β, are linked to the development of injury in the lungs after radiation therapy. However, most of the information that is available so far remains largely inconclusive.
Radiotherapy Effects: Berberine (TGF-β and sICAM-1)
Available evidence indicates that most patients develop lung toxicity after radiation therapy in two basic phases. The phases are early pneumonitis and late fibrosis. In the first case, the patient loses type I pneumocytes, the permeability of capillaries increases, and there is development of interstitial edema. The second phase is a repair process and it develops as the patient losses capillaries. There is thickening of the alveolar septa t and the alveolar space becomes obliterated.
One of the most common histopathological changes that take place when a person has radiation induced lung toxicity is inflammatory infiltration of the cells. The development is a dynamic process that involves chemokines, profibrotic cytokines, and proinflammatory cytokines. The processes are brought about by fibroblasts, macrophages, and epithelial cells. Intercellular adhesion molecular-1 (ICAM-1) and transforming growth factor-beta-1 (TGF-β) play critical roles in the pathogenesis of radiation induced lung injury. As a result, investigators have suggested their involvement in the development of lung toxicity after radiotherapy. In some reviews, researchers have outlined that TGF-β and ICAM-1 are switch cytokines, which are activated after radiation and afterwards promote cellular events, which lead to radiation induced toxicity of the lungs. Monitoring the two cytokines is an important step towards coming up with an intervention to prevent lung toxicity after radiotherapy.
Currently, there are two main drugs administered on patients suffering from lung toxicity after radiation therapy. The two drugs are cortisone and adrenocorticotropic hormone. There are other therapies used to treat toxicity after radiation therapy. However, they are largely ineffective among many patients. Additionally, they have adverse side effects, such as osteoporosis risk. Many patients, as a result, decline using them. Herbal drugs are regarded as efficacious alternatives to such drugs because of the lower risk of adverse side effects. Some of the newest therapies on trial include Chinese herbal drugs. For a long time, berberine was used as an antidiarrheal and antimicrobial drug. Experimental trials have pointed out that berberine attenuates liver fibrosis and inflammation by reducing TNFα- and TGF-β. Moreover, it was established that it attenuates tissue damage and destroys superoxide anion radicals.
Liu et al. conducted a study to determine whether berberine has therapeutic effects that can be explored for the treatment of radiotherapy effects on the lungs. All the patients who were involved in the study had inoperable stage III NSCLC. The patients did not have a history of any other cancer. The subjects received berberine at the time when they were undergoing 3D radiation therapy. On the other hand, the patients used in the control group were offered starch. The patients were treated using a total dose of 60 to 70 Gy, which was delivered in a single dose of 2 Gy every day. Lung DVHs were used to calculate V20 and V30. During the entire observation period, all the patients were offered similar medications.
Lung toxicity was graded from 0 to 4. It was then scored on the basis of pulmonary function loss, clinical symptoms, and radiological abnormalities. Before the treatment was administered, blood samples were obtained from the patients. Samples were also obtained after three, six, and twelve weeks. The samples were divided into two. The Enzyme Linked Immunosorbant Assay (herein referred to as ELISA) technique was used to measure the levels of TGF-β1 in the plasma after centrifugation. The other set of samples was used to determine the level of sICAM-1 in the serum. The two tests were conducted by different independent investigators who also averaged the values.
A spirometer was used to determine pulmonary function tests. The three measurements were forced vital capacity (herein referred to as FVC), FEV1, and DLCO. The tests were carried out before radiation therapy, after six weeks, and six months after radiotherapy. After completing therapy, all the patients were followed- up after six weeks, once a month for six months, and thereafter at intervals of four months. During the follow up visits, several evaluation tests were carried out. They included a physical examination and hepatic and renal function. Thoracic CT scan and clinical examinations were used to determine whether the patient had developed pneumonitis or not.
The prospective study was carried out between July 2004 and July 2006. It involved 90 patients, but five of them succumbed to cancer within the first six months. As a result of this, they were excluded from the study. The death of the two patients was a result of metastatic disease. One patient died of complications that were caused by metastatic disease and radiation induced lung toxicity while two patients succumbed to cardiac disease. Consequently, the patients were divided into two groups (42 in berberine group and 43 in control group). The table below shows the baseline characteristics of the patients. Study arms were properly balanced with regard to gender, age, disease stage, performance status, histology, GTV, lung function, smoke history, and irradiated lung volume.
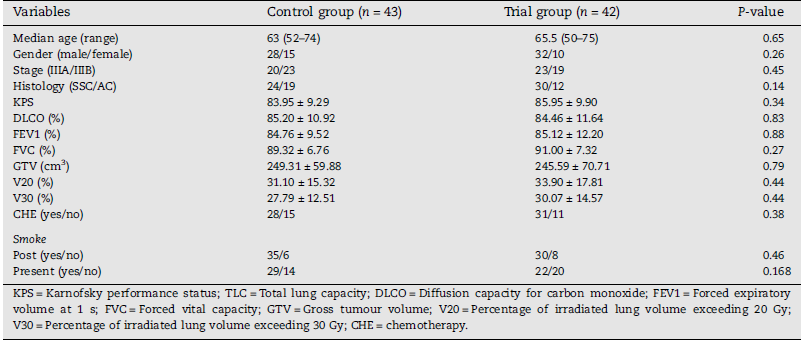
Liu et al. did not find any significant difference between the levels of sICAM-1 in the serum of the two groups at baseline. However, as the two groups were undergoing treatments, sICAM-1 levels increased and reached a maximum at twelve weeks. For the control group, the sICAM-1 levels after three, six, and twelve weeks were significantly higher than the levels at baseline. However, in the berberine group, only the six and twelve weeks levels were significantly higher than baseline levels. After six and twelve weeks, the levels of sICAM-1 in the berberine group were significantly lower than in the placebo group at a p <0.001.
The levels of TGF-β1 for both groups increased and reached a maximum after six weeks. The TGF-β1 level in the plasma was significantly lower in the trial group compared to the control group after three and six weeks. Compared to the level of TGF-β1 before the administration of radiotherapy, the control TGF-β1 levels were significantly higher than the baseline levels after three, six, and twelve weeks. However, trial TGF-β1 levels were significantly higher than baseline levels after three and six weeks.
With regard to changes in pulmonary function, the investigators found that FEV1 and DLCO values were significantly higher for the berberine group, but the significance of the FVC was marginal. Liu et al. also compared the decrease in the three pulmonary function test measurements for both groups. At the sixth week and sixth month, there was a reduction in the pulmonary function values for both groups. They noted that at the sixth week, decrease of FVC from baseline was less in the berberine group compared to the control group. The FEV1 and DLCO decrease at the sixth month was larger for the berberine group than for the other group, but the reduction was still significantly lower than in the placebo group. The observation implied that berberine had protected the patients from reducing pulmonary function variables. Other comparisons did not yield statistical differences.
Liu et al. found that 19 patients in the group that had received berberine and 31 patients in the placebo group had developed lung toxicity. After six months of radiation therapy, 15 out of 42 patients in the berberine group and 28 out of 43 in the placebo group had lung toxicity of grade 3 or more. None of the patients in the two groups had experienced grade 4 lung toxicity. There was significantly lower incidence of lung toxicity in the berberine group compared to the control group at six weeks and six months.
The median follow- up duration was 22 months. The MST for the berberine group was 23.1 months while that of the controls was 19.8 months. The difference in the tumor response and survival of the two groups was not statistically significant. Esophagitis was identified as the most common toxicity in the two groups. However, none of the 85 patients died or developed treatment delay as a result of the complication. There was no statistical difference between the developments of esophagitis in the two groups. Two patients had grade- 3 esophagitis, one in the berberine group and another in the placebo group. The other adverse events suffered by the patients were quite similar in the two groups.
The researchers managed to demonstrate that berberine reduced the incidence of lung toxicity, improved pulmonary function, and reduced the level of TGF-β1 and sICAM-1. Berberine did not have any adverse effects on the patients in the trial group, but apparently, it did not influence their survival. The results indicated that it is possible to use berberine in treating radiation induced lung injury.
Other studies pointed out that there was a correlation between the increase in TGF-β1 and sICAM-1 on the one hand and the development of lung injury after radiation therapy on the other hand. There is also evidence in support of the assumption that chronic inflammation stimulates the development of fibrosis as cytokines, chemokines, and growth factors are released. TGF-β1 and sICAM-1 are some of the most important released cytokines because they participate in lung toxicity pathogenesis. The level of TGF-β1 in the plasma is the main factor associated with the risk of radiation induced lung toxicity. As a result of this, the level of this compound in the plasma is utilized as a biological marker of lung toxicity after radiation therapy.
Some researchers have demonstrated that anti-TGF-β1 antibodies reduce the levels of TGF-β1. As a result, the antibodies can attenuate radiation induced lung toxicity that is caused by thoracic irradiation. ICAM-1 is a well-known LFA-1 (lymphocyte function associated antigen-1) ligand that in found on leukocytes. The interaction between ICAM-1 and LFA-1 is important for the activation of T-lymphocytes and the migration of lymphocytes into the inflammatory site. Research has determined that after radiation therapy, ICAM-1 is expressed on the cells of the lungs. Such studies have determined that ICAM-1 is an important factor in lung toxicity pathogenesis. It is believed that measuring soluble ICAM-1 is important in the monitoring and evaluation of radiation induced lung disease.
Studies have determined that the use of IMRT and amifostine can reduce lung toxicity by a large degree. However, there is no literature documenting that the use of traditional herbs, such as berberine, is effective in the treatment of acute lung toxicity. For a very long time, berberine was used by the Chinese for medicinal purposes. It is still used today in various herbal preparations. Liu et al. demonstrated that berberine serves as an anti-inflammation drug by inhibiting the synthesis of some cytokines, which are essential for the inflammation process. They also pointed out that berberine suppresses chemotaxis and the phagocytosis and migration of macrophages.
Experiments have demonstrated that in addition to antagonizing TGF-β1 effect, berberine reduces the production of matrix metalloproteinase-2 and kinae-plasminogen, which contribute to the production of extracellular material. Furthermore, it was found that not only does berberine reduce liver fibrosis, but it also enhances the effect of radiation in killing tumors. De Jaeger et al. determined that berberine blocks NF-kB translocation, which is a molecule that plays an important role in inflammation. In the Liu et al. series, the patients received a daily administration of berberine and they managed to demonstrate that the medicine reduces sICAM-1 and TGF-β1 in the blood among radiation therapy patients. However, they did not find a significant difference between the tumor response and survival of patients in the trial and control groups. The implication of the finding is that reduction in sICAM-1 and TGF-β1 is only achieved with respect to lung injury. The results suggested there is a probability the reduction of sICAM-1 and TGF-β1 levels plays a significant role in enhancing therapeutic impacts of berberine.
Chapter Summary
In chapter two, the researcher took the reader through a critical analysis of the literature that is found in this field. The aim was to locate the current study within the broader field of radiation oncology. The literature review also helped the researcher to identify gaps existing in this field, gaps that will be addressed in the current study. Disagreements and agreements among various scholars in this field were also analyzed. In chapter three, the researcher will provide the reader with an analysis of the steps that were taken in carrying out the current study. Some of the issues that are addressed in chapter three include selection of sample, collection of data, and data analysis.
Materials and Methods
Introduction
In chapter 3, the reader will be provided with information touching on the steps that were taken or followed in collecting and analyzing data for the current study. Some of the issues that are addressed include, among others, study design, eligibility of patients used in the study, and statistical analysis. Limitations and potential weaknesses of the methodology will be identified and explained where necessary.
Study Design
The current study was a clinical trial that aimed at gathering preliminary results of tomotherapy for the treatment of inoperable recurrent non- small cell lung cancer at stump site after right pneumonectomy. The results were gathered by escalating radiation dose and reducing radiation exposure to the right- shifted heart and to the only one remnant left normal lung caused by right pneumonectomy. Patients who had received induction chemotherapy were not included in the study. The development, review, and management of the trial were carried out according to the international standards that govern human experimentation. The Soonchunhyang University Bucheon Hospital review board approved of the study before the inclusion of any of the twenty three patients. All the patients consented to the trial in writing before they were included.
Patient Eligibility
The patients used in the study were histologically proven to have stages I-III NSCLC. They were only eligible if it was possible to encompass the entire detectable tumor under the tomotherapy radiation field. The detectable tumor referred to include the primary tumor and lymph nodes that were involved. The patients with supraclavicular metastasis in the nodes were not included.
All the patients were more than 18 years of age and had a performance status of more or equal to 70%. Because the interest of the study was to independently figure out the efficiency of tomotherapy in dose escalation to the targeted tumor and toxicity reduction, patients undergoing concurrent chemotherapy were not included in the study. Other patients who were ineligible were those who had undergone other kinds of resections that were less than a pneumonectomy, those who received left pneumonectomies, those who had received radiotherapy prior to the study, those with small cell lung cancer, and those with distant metastasis. All the patients included in the study had developed loco regional recurrence after the curative right pneumonectomy. In the 23 cases, the histology at recurrence was similar to that of initial tumor. The staging evaluations that were carried out included the medical history of patients, complete blood counts, physical examination, biochemical tests, bronchoscopy, tomography and chest X-rays, ultrasound images of the abdomen, as well as liver, brain, and bone radionuclide scans. Locoregional recurrence was diagnosed using computed tomotherapy or abnormal observations on bronchoscopy. The characteristics of the patients before radiation therapy are shown in the table below:
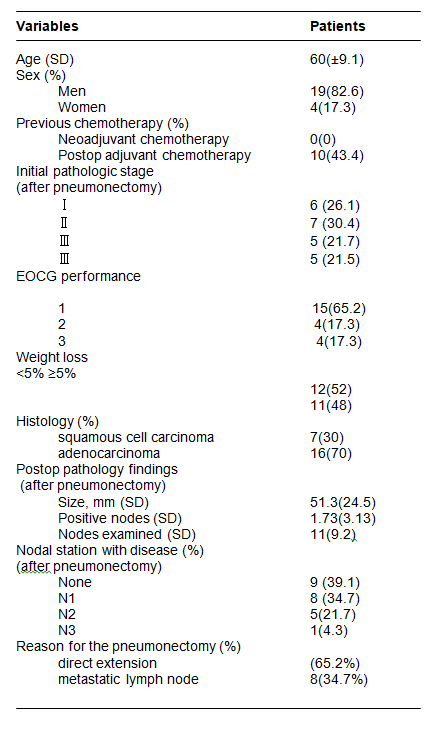
Statistical Analysis
The overall rate of survival at one and two years was calculated using the Kaplan-Meier method. The prognostic factors of the patients were evaluated using Cox regression model and log- rank test. The Common Terminology Criteria for Adverse Event version 3.0 was used to assess the toxicity effects associated with radiation therapy.
Treatment Planning
Helical tomotherapy was used to deliver a dose of 2.9 Gy for a period of 30 days to all patients. As a result, the total radiation received was 69 Gy per patient. Radiation was targeted at both the primary tumor and involved nodal regions. However, elective nodal irradiation was not carried out. Planning imaging involved a thin slice treatment planning 4D- CT and CT. Respiratory motion was reduced and normalized using a double vacuum immobilization system. In order to determine the extent of the gross tumor volume (herein referred to as GTV), the researchers used PET imaging. The Tomotherapy Treatment Planning System was used to plan treatment.
There are three parameters that affect treatment times and dose conformity when using tomotherapy. The three are modulation factor, pitch, and width of the field. In this particular study, the field modulation factor was 4, the pitch was 0.28, and the width was 2.5cm. In the current study, 99% of PTV was set to be irradiated at 69 Gy at 2.3 Gy in 30 fractions. In order to prevent the irradiation of the left normal lung, the researchers used directional blocking. The dose that was delivered to normal organs was limited to less than 4 Gy for the left lung. The volume of the heart that would receive more than 2.5 Gy of radiation was limited to less than 10%.
Evaluation of Survival and Toxicity
All the patients were followed up for evaluation which included chest CT, chest X-ray, and physical examinations. The examination was carried out at intervals of three months for a period of two years after the completion of radiotherapy, and thereafter at six- month intervals. Overall, survival of the patients was calculated from the time they started treatment to December 2011 or when the patient died.
Chapter Summary
The aim of chapter three was to provide the reader with information on the steps that were followed in conducting the study. The study design, patient eligibility, and treatment plan adopted for the study were discussed. In addition, the researcher looked at the statistical analysis that was used, as well as the evaluation of survival and toxicity among the patients used for the study. A total of 23 patients were used in this study. In chapter 4, the findings of the study will be presented.
Results
Introduction
The findings made from the study design that was described in chapter 3 are presented in chapter 4. Among others, the researcher will analyze the findings on prognostic factors and survival, treatment failure among the patients used in the study, lung function and complications.
Prognostic Factors and Survival
We found that there were no significant differences between the overall survival rates among patients who had suffered recurrence for stage I to stage II and those at stage III NSCLC (p<0.16). We analyzed the impacts of prognostic factors like age, performance status, disease free interval (herein referred to as DFI), and the dose of radiation on the overall survival of patients. Of all these factors, the escalation of the total radiation dose from 60 Gy to 69Gy had a significant impact on the survival of patients. The results are shown in the table below:
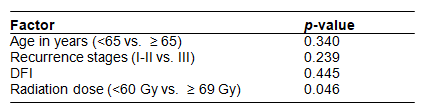
The overall survival rate for the patients used in the study is presented in the figure below:
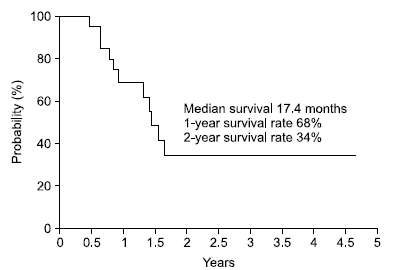
Treatment Failure
Twelve patients (52%) experienced treatment failure after completing radiation therapy. Seven of the twelve had re- progression at 4 months median time after radiotherapy. Four out of the seven patients died of local progression of NSCLC and one died of distant progression after local progression. Five patients died of distant progression of the disease at the liver, brain, bone multiple lymph nodes.
All the patients were tested for pulmonary function before the salvage treatment and afterwards. The two tests that were used in the analysis were forced expiratory volume in one second (herein referred to as FEV1) and diffusing lung capacity for carbon monoxide (herein referred to as DLCO). There was a significant decrease in DLCO after treatment for locoregional recurrence (p<0.030). However, there was no difference in the mean of FEV1 values before and after radiation. We also compared the DCLO and FEV1 values of the patients before right pneumonectomy with the values after radiation therapy. There was a statistically significant difference. The results are shown in the table below:
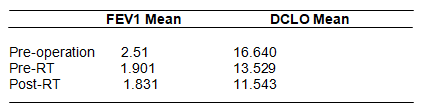
Various grades of radiation pneumonitis were observed among 7 patients (30%). One of the patients included in the study had grade 3 radiation pneumonitis and was treated using steroid therapy. The patient recovered. Within six months after the radiation treatment, three patients died of pulmonary complications. One patient died of bacterial pneumonia while two died of radiation pneumonitis. Nine patients (39%) experienced radiation esophagitis after the treatment. Five patients suffered grade 3 esophagitis and as such, they required fluid support during radiation therapy.
Chapter Summary
In this chapter, the reader was provided with information touching on the findings that were made in the study. In chapter 5, these results and findings are discussed. A conclusion is also provided in chapter 5.
Discussion and Conclusion
Despite the use of pneumonectomy and other resection procedures for the treatment of NSCLC, up to 30% of the patients experience recurrence. Locoregional recurrence is very important for the attainment of overall survival and cure for NSCLC patients. As a result of this, subsequent treatment is required. Although reoperation is adopted for the treatment of some patients, the procedure is very limited. The two main modes of treatments for loco regional recurrence are chemotherapy and radiotherapy. Various retrospective studies have documented that the median overall survival for such patients is between 10 and 20 months. There are various prognostic factors, which have diverse impacts on the overall survival. They include where the recurrence has occurred, the objective of the treatment (palliative or curative), disease-free interval, and the incorporation of chemotherapy.
Various studies have suggested that patients who have undergone resection after recurrence have a rate of survival that is comparable to that of those who have just been diagnosed with NSCLC. The observation is made when the two groups of patients receive curative radiotherapy or chemotherapy. For the attainment of cure, the researchers have pointed out that patients who have suffered from NSCLC recurrence should be offered aggressive therapy. One of the main concerns of administering curative radiotherapy to NSCLC recurrence patients is the impact of such treatment on their pulmonary and cardiac functions. In the current case, the lung function of the patients was already compromised because of their first operation after they were initially diagnosed with NSCLC. Even if the pulmonary function of the patients is normal after right pneumonectomy, there is always the likelihood that salvage radiation interferes with lung function.
The 17% median overall survival and 34% survival rate within two years were comparable to the findings of other investigators. For instance, Rea et al. documented that the overall survival among 45 locoregional recurrent NSCLC patients was 11 months. They also found that patients who were treated with a dose of more than 50Gy had better health outcomes than their counterparts who had received lower palliative doses. In another retrospective study that included 30 patients who were irradiated with 47 to 60 Gy for the treatment of recurrent NSCLC, the overall survival rate was 29% while the median survival rate was 14 months. They found that the use of radiotherapy prognostically indicated survival.
Yamamoto et al. reported that the median survival of 35 patients who were treated with radical radiotherapy for curative purposes was 25 months. On the other hand, those who were treated with lower does for palliative purposes had a 10.6 months median survival. Kim et al. also conducted a study to determine the efficacy of using radiotherapy in the treatment of recurrent NSCLC after right pneumonectomy. The scholars found that the median survival among 38 patients was one and a half years. The two-year rate of survival was 37%. In this particular study, the dose administered on the patients was between 55 and 60 Gy. There was statistically significant difference between the 2 year rate of survival and median survival depending on whether the salvage radiation was used with a palliative or curative intent (37% and 11%, 18 months and 7 months respectively).
Another study that compared the use of radiotherapy among patients who were resected with those who had not received surgical treatment used a radiation dose of 55Gy for those suffering from recurrent disease and 60Gy newly diagnosed NSCLC. The median survival rate for the patients in both groups was 11 months while the 2- year rate of survival was 21% and 27% among the recurrent and newly diagnosed patients respectively. When the patients who had bronchial stump recurrence were compared to those having lesions in the chest wall or lymph nodes, a significant difference was evident. In this study, the investigators concluded that aggressive radiotherapy should be offered to those patients who have suffered locoregional recurrence after resection and those who have just been diagnosed with NSCLC.
Gómez-Caro et al. carried out a study to draw comparisons between newly diagnosed NSCLC patients and those who had locoregional recurrence after resection. They suggested that locoregional recurrence patients should receive aggressive chemotherapy and radiotherapy. In their study, they did not find any significant differences in the overall rate of survival among stage I to stage III patients suffering from newly diagnosed disease and recurrence patients. They also carried out a multivariate analysis for the prognostic role of chemotherapy PFS in five years. Some studies differ to some extent when it comes to prognostic factors. For example, some of them have associated recurrence on the bronchial stump with greater survival, but others have not found such correlations. Additionally, other studies postulate that increased radiation doses lead to improved outcomes among patients who had received a resection and later suffered from locoregional recurrence.
In the current study, we found that the dose of radiation had a statistical significance when it comes to the overall survival of the patients. The observation explains why only four patients in the study succumbed to aggressive tumors. Most oncologists are of the opinion that there is a positive relationship between the dose of radiation and health outcomes. In this regard, if it is possible to reduce toxicity to a minimum, it is expected that higher doses of radiation would increase local control. The findings on the dose- outcome relationship in the current study are applicable to other cases because unlike other researchers who have only performed retrospective studies on the same, we performed a clinical investigation. There is a higher possibility that when high doses of radiation are used among patients suffering from newly diagnosed NSCLC, better outcomes are achieved than in the case of locoregional recurrent NSCLC.
Currently, the lung cancer toxicity grading systems are classified on the basis of symptom severity as opposed to PFT parameters. Various studies were carried out to find out the relationship between lung and heart complications and PFT after the administration of radiotherapy. Generally, a FEV1 decrease is indicative of obstruction in the lung while a DLCO decrease is indicative of impairment in partial diffusion of the lungs. We found that there was significant decrease in lung functions after the administration of salvage radiation. There are other studies with the opinion that the lung’s diffusing capacity reduces when a person receives radiotherapy for locoregional recurrent NSCLC. In this regard it is very essential to consider the impact of radiation on pulmonary function before settling for salvage radiation.
References
Ishikawa H, Nakayama Y, Nakano T, et al. Effect of histologic type on recurrence pattern in radiation therapy for medically inoperable patients with Stage I non-small-cell lung cancer. Lung. 2006;184(6): 347-353.
Oshita F, Ohe M, Yamada K, et al. Phase II study of nedaplatin and irinotecan with concurrent thoracic radiotherapy in patients with locally advanced non-small-cell lung cancer. British Journal of Cancer. 2010;103(9): 1325-1330.
Behzadi A, Yee U, Lowe V, Deschamps C. The role of positron emission tomography in the management of non-small cell lung cancer. Canadian Journal Of Surgery. 2009;52(3): 235-242.
Lam S. Photodynamic therapy for lung cancer. Semin Oncol. 1994;21(6Suppl 15): 15-19.
Song S, Jeong S, Choi E, et al. Clinical significance of NQO1 C609T polymorphisms after postoperative radiation therapy in completely resected non-small cell lung cancer. Lung Cancer (01695002). 2010;68(2): 278-282.
Steger V, Spengler W, Walles T, et al. Pneumonectomy: calculable or non-tolerable risk factor in trimodal therapy for Stage III non-small-cell lung cancer?. European Journal Of Cardio-Thoracic Surgery. 2012;41(4): 880-885.
Ichiki Y, Nagashima A, Chikaishi Y, Yasuda M. Pneumonectomy for non-small cell lung cancer. Surgery Today. 2012;42(9): 830-834.
Peñagarícano J, Chao M, Van Rhee F, Moros E, Corry P, Ratanatharathorn V. Clinical feasibility of TBI with helical tomotherapy. Bone Marrow Transplantation. 2011;46(7): 929-935.
Tada T, Fukuda H, Inoue Y, et al. Non-small cell lung cancer: radiation therapy for locoregional recurrence after complete resection. International Journal Of Clinical Oncology. 2005;10(6): 425-428.
Dai J, Gu J, Wu X, et al. Genetic variations in the regulator of G-Protein signaling genes are associated with survival in late- stage non-small cell lung cancer. Plos ONE. 2011;6(6): 1-10.
Ohguri T, Imada H, Korogi Y, et al. Systemic chemotherapy using paclitaxel and carboplatin plus regional hyperthermia and hyperbaric oxygen treatment for non-small cell lung cancer with multiple pulmonary metastases: preliminary results. International Journal Of Hyperthermia. 2009;25(2): 160-167.
Yamauchi Y, Izumi Y, Nomori H, et al. Percutaneous cryoablation for the treatment of medically inoperable stage I non-small cell lung cancer. Plos ONE. 2012;7(3): 1-5.
Wheeler S, Wu Y, Weiner B, et al. Use and timeliness of radiation therapy after breast-conserving surgery in low-income women with early-stage breast cancer. Cancer Investigation. 2012;30(4): 258-267.
Bellon J, Harris E, Haffty B, et al. ACR appropriateness criteria conservative surgery and radiation – stage I and II breast carcinoma. Breast Journal. 2011;17(5): 448-455.
Coon AB, et al. Tomotherapy and multified intensity-modulated radiotherapy planning reduce cardiac doses in left-sided breast cancer patients with unfavorable cardiac anatomy. Int. J. Radiation Oncology Biol. Phys. 2010;78(1): 104–110.
Sharma C, Harris L, Haffty B, Yang Q, Moran M. Does compliance with radiation therapy differ in African-American patients with early-stage breast cancer? Breast Journal [serial online]. March 2010;16(2): 193-196.
Schmitz K, Speck R, Rye S, DiSipio T, Hayes S. Prevalence of breast cancer treatment sequelae over 6 years of follow-up. Cancer (0008543X). 2012;118: 2217-2225.
Kawaguchi T, Tojo T, Kushibe K, Kimura M, Nagata Y, Taniguchi S. Short-term and long- term outcomes after pneumonectomy for primary lung cancer. Ann Thorac Cardiovasc Surg. 2008;14(1): 289-293.
Pless M, Gambazzi F, Stillhart P, Lieb T, Brutsche M. Induction chemotherapy followed by parenchyma-sparing surgery in medically inoperable NSCLC—results of a feasibility study. Lung Cancer (01695002). 2008;62(2): 228-235.
Kappers I, van Sandick J, Burgers S, Belderbos J, van Zandwijk N, Klomp H. Surgery after induction chemotherapy in stage IIIA-N2 non-small cell lung cancer: why pneumonectomy should be avoided. Lung Cancer (01695002). 2010;68(2): 222-227.
Rea F, Marulli G, Sartori F, et al. Tracheal sleeve pneumonectomy for non small cell lung cancer (NSCLC): short and long-term results in a single institution. Lung Cancer (01695002). 2008;61(2): 202-208.
Gómez-Caro A, Garcia S, Gimferrer J, et al. Determining the appropriate sleeve lobectomy versus pneumonectomy ratio in central non-small cell lung cancer patients: an audit of an aggressive policy of pneumonectomy avoidance. European Journal Of Cardio-Thoracic Surgery. 2011;39(3): 352-359.
Storelli E, Tutic M, Weder W, et al. Sleeve resections with unprotected bronchial anastomoses are safe even after neoadjuvant therapy. European Journal Of Cardio-Thoracic Surgery. 2012;42(1): 77-81.
Petrella F, Radice D, Spaggiari L, et al. The impact of preoperative body mass index on respiratory complications after pneumonectomy for non-small-cell lung cancer: results from a series of 154 consecutive standard pneumonectomies. European Journal Of Cardio-Thoracic Surgery. 2011;39(5): 738-744.
Shin-ichi T, Hajime M, Masaru K, Yoko M, Noriyoshi S, Masayoshi I, Toshiteru T, Mitsunori O. Comparison of surgical results after pneumonectomy and sleeve lobectomy for non-small cell lung cancer: trends over time and 20-year institutional experience. European Journal of Cardio-thoracic Surgery. 2006;29: 276—280.
Yamamoto H, Takagi H, Goto S, Matsui M, Umemoto T. A meta-analysis of adjusted and unadjusted observational studies of sleeve lobectomy vs pneumonectomy for non-small cell lung cancer. Thorax. 2011;4: 145.
Demir A, Gunluoglu M, Sansar D, Melek H, Dincer S. Staging and resection of lung cancer with minimal invasion of the adjacent lobe. European Journal Of Cardio-Thoracic Surgery. 2007;32(6): 855-858.
Fernandez FG, Seth D, Force MD, et al. Impact of laterality on early and late survival after pneumonectomy. Ann Thorac Surg. 2011;92: 244 –50.
Neuboeck N, Lindenmann J, Smolle-Jüttner F, et al. Intraoperative radiotherapy (IORT) – alternative treatment in functionally nonresectable nonsmall cell lung cancer (NSCLC). European Surgery: ACA Acta Chirurgica Austriaca. 2010;42(5): 209-213.
Posther K, Harpole D. The surgical management of lung cancer. Cancer Investigation. 2006;24(1): 56-67.
Grodzki T, Alchimowicz J, Witkowska D, et al. Additional pulmonary resections after pneumonectomy: actual long-term survival and functional results. European Journal Of Cardio-Thoracic Surgery. 2008;34(3): 493-498.
Kim AW, Faber LP, Warren WH, et al. Pneumonectomy after chemoradiation therapyfor non-small cell lung cancer:does “side” really matter? Ann Thorac Surg. 2009;88: 937– 44
Smulders SA, Holverda S, Vonk-Noordegraaf A, et al. Cardiac function and position more than 5 years after pneumonectomy. Ann Thorac Surg. 2007;83: 1986–92.
Sonoda S, Kumagawa Y, Inada EA. Case of cardiac herniation after extrapleural pneumonectomy for malignant thymoma. Journal Of Anesthesia. 2010;24(6): 926-929.
Kiev J, Parker M, Xian Z, Kasirajan V. Cardiac herniation after intrapericardial pneumonectomy and subsequent cardiac tamponade. American Surgeon. 2007;73(9): 906-908.
Gopaldas R, Angelico R. Incarcerated biatrial thromboembolus after extrapleural pneumonectomy: a surgical conundrum. American Surgeon. 2010;76(9): 1022-1025.
Alexiou C, Beggs D, Onyeaka P, et al. Pneumonectomy for Stage I (T1N0 and T2N0) nonsmall cell lung cancer has potent, adverse impact on survival. Ann Thorac Surg. 2003;76: 1023–1028.
Thomas P, Doddoli C, Thirion X, et al. Stage I non-small cell lung cancer: a pragmatic approach to prognosis after complete resection. Ann Thorac Surg. 2002;73: 1065–70.
Law MR, Henk JM, Lennox SC, Hodson ME. Value of radiotherapy for tumour on the bronchial stump after resection for bronchial carcinoma. Thorax. 1982;37: 496-499
Jeremic BA, Shibamoto YB, Milicic BA, et al. External beam radiation therapy alone for loco-regional recurrence of non-small-cell lung cancer after complete resection. Lung Cancer. 1999;23: 135–142.
Lester J. Palliative thoracic radiotherapy in NSCLC. Current Medical Literature: Lung Cancer. 2008;1(4): 105-110.
Verstegen N, Lagerwaard F, Haasbeek C, Slotman B, Senan S. Outcomes of stereotactic ablative radiotherapy following a clinical diagnosis of stage I NSCLC: comparison with a contemporaneous cohort with pathologically proven disease. Radiotherapy & Oncology. 2011;101(2): 250-254.
Nitsche M, Christiansen H, Lederer K, Griesinger F, Schmidberger H, Pradier O. Fludarabine combined with radiotherapy in patients with locally advanced NSCLC lung carcinoma: a phase I study. Journal Of Cancer Research & Clinical Oncology. 2012;138(7): 1113-1120.
Curran WJ, Herbert SA, Patrickm SM, et al. Should patients with post-resection locoregional recurrence of lung cancer receive aggressive therapy? Int. J. Radiation Oncology Biol. Phys. 1992;24: 25-30.
Petrović M, Ilić N, Kostić G, et al. Risk factors for brain metastases in surgically staged IIIA non-small cell lung cancer patients treated with surgery, radiotherapy and chemotherapy. Vojnosanitetski Pregled: Military Medical & Pharmaceutical Journal Of Serbia & Montenegro. 2011;68(8): 643-649.
Hallqvist A, Bergman B, Nyman J. Health related quality of life in locally advanced NSCLC treated with high dose radiotherapy and concurrent chemotherapy or cetuximab – pooled results from two prospective clinical trials. Radiotherapy & Oncology. 2012;104(1): 39-44.
Clarke K, Taremi M, Sun A, et al. Stereotactic body radiotherapy (SBRT) for non-small cell lung cancer (NSCLC): is FDG-PET a predictor of outcome? Radiotherapy & Oncology. 2012;104(1): 62-66.
Kagami Y, Nishio M, Narimatsu N, et al. Radiotherapy for locoregional recurrent tumors after resection of non-small cell lung cancer. Lung Cancer. 1998;20: 31–35.
Simone C. The role of palliative care in patients with NSCLC. Current Medical Literature: Lung Cancer. 2011;5(1): 1-16.
Jeremić B, Munshi A, Agarwal J, et al. Surgery versus radiotherapy in early-stage NSCLC. Current Medical Literature: Lung Cancer. 2010;4(2): 37-43.
Zhang X, Li Y, Chang J, et al. Intensity-modulated proton therapy reduces the dose to normal tissue compared with intensity-modulated radiation therapy or passive scattering proton therapy and enables individualized radical radiotherapy for extensive stage IIIB non-small-cell lung. International Journal Of Radiation Oncology, Biology, Physics. 2010;77(2): 357-366.
Everitt S, Schneider-Kolsky M, Yuen K, Budd R, Mac Manus M. Dose escalation of radical radiation therapy in non-small-cell lung cancer using positron emission tomography/computed tomography-defined target volumes: are class solutions obsolete? Journal Of Medical Imaging & Radiation Oncology. 2008;52(2): 168-177.
Nakayama H, Satoh H, Kurishima K, Ishikawa H, Tokuuye K. High-dose conformal radiotherapy for patients with stage III non–small-cell lung carcinoma. Int. J. Radiation Oncology Biol. Phys. 2010;78(3): 645–650.
Wu K, Jiang G, Zhao S, et al. Three-dimensional conformal radiation therapy for non–small-cell lung cancer: A Phase I/II dose escalation clinical trial. International Journal Of Radiation Oncology, Biology, Physics. 2003;57(5): 1336.
Schild S, Korte S, Wong W, Vora S, Younggren J, Ezzell G. Treatment planning for dose escalation in non-small cell lung cancer (NSCLC). Medical Dosimetry. 2004;29(3): 196-203.
McGibney C, Holmberg O, McClean B, Armstrong J. Analysis of dose distribution in the ‘Rind’ – a volume outside the PTV – in 3-dimensional conformal radiation therapy of non-small cell lung cancer. Radiotherapy & Oncology. 2003;66(1): 87.
Werner-Wasik M, Swann R, Sause W, et al. Increasing tumor volume is predictive of poor overall and progression-free survival: secondary analysis of the radiation therapy oncology group 93-11 phase i-ii radiation dose-escalation study in patients with inoperable non–small-cell lung cancer. International Journal Of Radiation Oncology, Biology, Physics. 2008;70(2): 385-390.
Gillham C, Zips D, Baumann M, et al. Additional PET/CT in week 5–6 of radiotherapy for patients with stage III non-small cell lung cancer as a means of dose escalation planning? Radiotherapy & Oncology. 2008;88(3): 335-341.
Vogelius SI, Westerly DC, Cannon GM, et al. IMRT may increase pneumonitis risk relative to 3D-CRT in patients receiving combined chemotherapy and radiation therapy: a modeling study of dose dumping. Int J Radiat Oncol Biol Phys. 2011; 80(3): 893–899.
Hardy D, Liu C, Cormier J, Xia R, Du X. Cardiac toxicity in association with chemotherapy and radiation therapy in a large cohort of older patients with non-small-cell lung cancer. Annals Of Oncology. 2010;21(9): 1825-1833.
Schytte T, Hansen O, Stolberg-Rohr T, Brink C. Cardiac toxicity and radiation dose to the heart in definitive treated non-small cell lung cancer. Acta Oncologica. 2010;49(7): 1058-1060.
Bellière A, Girard N, Mornex F, et al. Feasibility of high-dose three-dimensional radiation therapy in the treatment of localised non-small-cell lung cancer. Cancer Radiotherapie. 2009;13(4): 298-304.
Lohr F, El-Haddad M, Dobler B, et al. Potential effect of robust and simple imrt approach for left-sided Breast cancer on cardiac mortality. Int. J. Radiation Oncology Biol. Phys. 2009;74(1): 73–80
Huang E, Hope A, Bradley J, et al. Heart irradiation as a risk factor for radiation pneumonitis. Acta Oncologica. 2011;50(1): 51-60.
Gandhi L, Linden P, Plant P. Chemotherapy and radiotherapy. Current Medical Literature: Lung Cancer. 2012;5(4): 133-137.
Aksakal E, Sevımlı S, Karakelleoğlu Ş, et al. Assessment of the left atrial longitudinal myocardial function by the strain and strain rate echocardiography in patients with rheumatic mitral stenosis. Turkish Journal Of Medical Sciences. 2011;41(6): 965-974.
Erven K, Jurcut R, Weltens C, et al. Acute radiation effects on cardiac function detected by strain rate imaging in breast cancer patients. Int. J. Radiation Oncology Biol. Phys. 2011;79(5); 1444–1451.
Park S, Hong S, Shim W, et al. Relationship between strain rate imaging and coronary flow reserve in assessing myocardial viability after acute myocardial infarction. Echocardiography. 2010;27(8): 977-984.
Seddon B, Cook A, Yarnold J, et al. Detection of defects in myocardial perfusion imaging in patients with early breast cancer treated with radiotherapy. Radiotherapy & Oncology. 2002;64(1): 53.
Marks L, Yu X, Borges-Neto S, et al. The incidence and functional consequences of RT-associated cardiac perfusion defects. International Journal Of Radiation Oncology, Biology, Physics. 2005;63(1): 214-223.
Barker P, Houle H, Li J, Miller S, Herlong J, Camitta M. Global longitudinal cardiac strain and strain rate for assessment of fetal cardiac function: novel experience with velocity vector imaging. Echocardiography. 2009;26(1): 28-36.
Evans ES, Prosnitz RG, Yu X, et al. Impact of patient-specific factors, irradiated left ventricular volume, and treatment set-up errors on the development of myocardial perfusion defects after radiation therapy for left-sided breast cancer. Int. J. Radiation Oncology Biol. Phys. 2006;66(4): 1125–1134.
Nogueira L, de Almeida A, Barroso R, et al. Evaluation of rib microstructure in Wistar rats using SR-μCT after radiation therapy simulation for breast cancer. Applied Radiation & Isotopes. 2012;70(7): 1296-1299.
Askoxylakis V, Jensen A, Hof H, et al. Simultaneous integrated boost for adjuvant treatment of breast cancer- intensity modulated vs. conventional radiotherapy: the IMRT-MC2 trial. BMC Cancer. 2011;11(1): 249-256.
Lind PA , Pagnanelli R, Marks LB, et al. Myocardial perfusion changes in patients irradiated for left-sided breast cancer and correlation with coronary artery distribution. Int. J. Radiation Oncology Biol. Phys. 2003;55(4): 914–920.
Matzinger O, Heimsoth I, Tienhoven G, et al. Toxicity at three years with and without irradiation of the internal mammary and medial supraclavicular lymph node chain in stage I to III breast cancer (EORTC trial 22922/10925). Acta Oncologica. 2010;49(1): 24-34.
Correa CR, Das IJ, Litt HI, et al. Association between tangential beam treatment parameters and cardiac abnormalities after definitive radiation treatment for left-sided breast cancer. Int. J. Radiation Oncology Biol. Phys. 2008;72(2): 508–516.
Ring A, Reed M, Coleman R, et al. The treatment of early breast cancer in women over the age of 70. British Journal Of Cancer. 2011;105(2): 189-193.
Vikström J, Hjelstuen M, Mjaaland I, Dybvik K. Cardiac and pulmonary dose reduction for tangentially irradiated breast cancer, utilizing deep inspiration breath-hold with audio-visual guidance, without compromising target coverage. Acta Oncologica. 2011;50(1): 42-50.
Chi A, Zhongxing L, Komaki R, et al. Dosimetric selection for helical tomotherapy based stereotactic ablative radiotherapy for early-stage non-small cell lung cancer or lung metastases. Plos ONE. 2012;7(4): 1-6.
Park HJ, Kim J, Park SH, Kay C, Jung S. Early CT findings of tomotherapy-induced radiation pneumonitis after treatment of lung malignancy. AJR. 2009;:193: 209-213.
Kong F, Hayman JA, Griffith KA, et al. Final toxicity results of a radiation-dose escalation study in patients with non–small-cell lung cancer (NSCLC): predictors for radiation pneumonitis and fibrosis. Int. J. Radiation Oncology Biol. Phys. 2006;65(4): 1075–1086.
Bertelsen A, Hansen O, Brink C. Does VMAT for treatment of NSCLC patients increase the risk of pneumonitis compared to IMRT? – a planning study. Acta Oncologica. 2012;51(6): 752-758.
Ramella S, Trodella L, D’Angelillo R, et al. Adding Ipsilateral V20 and V30 to conventional dosimetric constraints predicts radiation pneumonitis in stage iiia–b nsclc treated with combined-modality therapy. International Journal Of Radiation Oncology, Biology, Physics. 2010;76(1): 110-115.
Kocak Z, Evans ES, Zhou S, et al. Challenges in defining radiation pneumonitis in patients with lung cancer. Int. J. Radiation Oncology Biol. Phys. 2005;62(3): 635–638.
Chi A, Zhongxing L, Komaki R, et al. Dosimetric selection for helical tomotherapy based stereotactic ablative radiotherapy for early-stage non-small cell lung cancer or lung metastases. Plos ONE . 2012;7(4): 1-6.
Yirmibesoglu E, Higginson D, Marks L, et al. Challenges scoring radiation pneumonitis in patients irradiated for lung cancer. Lung Cancer (01695002). 2012;76(3): 350-353.
Takeda A, Ohashi T, Kunieda E, et al. Early graphical appearance of radiation pneumonitis correlates with the severity of radiation pneumonitis after stereotactic body radiotherapy (SBRT) in patients with lung tumors. Int. J. Radiation Oncology Biol. Phys. 2010;77(3): 685–690.
Ramella S, Trodella L, D’Angelillo R, et al. Beams arrangement in non-small cell lung cancer (NSCLC) according to ptv and dosimetric parameters predictive of pneumonitis. Medical Dosimetry. 2010;35(3): 169-178.
Huang E, Hope A, Bradley J, et al. Heart irradiation as a risk factor for radiation pneumonitis. Acta Oncologica. 2011;50(1): 51-60.
Dehing-Oberije C, De Ruysscher D, Van Baardwijk A, Yu S, Rao B, Lambin B. The importance of patient characteristics for the prediction of radiation-induced lung toxicity. Radiotherapy and Oncology. 2009;65(2): 345-351.
Jun D, Guang L, Xiaobe L, Lei Y, Shuo Z, Zhan Y. Analysis of related factors associated with radiation pneumonitis in patients with locally advanced non-small-cell lung cancer treated with three-dimensional conformal radiotherapy. Journal Of Cancer Research & Clinical Oncology. 2010;136(8): 1169-1178.
Tucker S, Jin H, Liao Z, et al. Impact of toxicity grade and scoring system on the relationship between mean lung dose and risk of radiation pneumonitis in a large cohort of patients with non–small cell lung cancer. International Journal Of Radiation Oncology, Biology, Physics. 2010;77(3): 691-698.
Barriger R, Fakiris A, Hanna N, Yu M, Mantravadi P, McGarry R. Dose–volume analysis of radiation pneumonitis in non–small-cell lung cancer patients treated with concurrent cisplatinum and etoposide with or without consolidation docetaxel. International Journal Of Radiation Oncology, Biology, Physics. 2010;78(5): 1381-1386.
Park E, Ramnath N, Park Y, et al. High superoxide dismutase and low glutathione peroxidase activities in red blood cells predict susceptibility of lung cancer patients to radiation pneumonitis. Free Radical Biology & Medicine. 2007;42(2): 280-287.
Jackson I, Liguang C, Batinic-Haberle I, Vujaskovic Z. Superoxide dismutase mimetic reduces hypoxia-induced , TGF-β, and VEGF production by macrophages. Free Radical Research. 2007;41(1): 8-14.
De Jaeger K, Seppenwoolde Y, Kampinga H, Boersma L, Belderbos J, Lebesque J. Significance of plasma transforming growth factor-β levels in radiotherapy for non–small-cell lung cancer. International Journal Of Radiation Oncology, Biology, Physics. 2004;58(5): 1378.
Kunyu Y, Palm J, Rübe C, et al. Matrix-Metallo-Proteinases and their tissue inhibitors in radiation-induced lung injury. International Journal Of Radiation Biology. 2007;83(10): 665-676.
Liu Y, Yub H, Zhanga C, et al. Protective effects of berberine on radiation-induced lung injury via intercellular adhesion molecular-1 and transforming growth factor-beta-1 in patients with lung cancer. International Journal of Radiation Biology. 2007;84(10): 65-66.