Introduction
- Conscious Sedation:
- Drug-induced repression of consciousness during procedural interventions (Fencl, 2016).
- Consciously sedated patient:
- Responds with verbal cues or tactile reflexes.
- Protective airway reflexes.
- Unimpaired cardiovascular function.
- Adequate spontaneous breathing.
- Considerations for a nurse (RN):
- Patient evaluation & monitoring.
- Knowledge of pharmacological agents & their side effects.
- Proper airway management.
Sedation exists in a continuum. Producing an appropriate depth of sedation is required to avoid respiratory complications. A patient under an appropriate level of conscious sedation exhibits various purposeful responses. He/she has the ability to respond through verbal cues or tactile reflexes and can counteract airway obstruction due to foreign materials. In addition, the patient shows unimpaired cardiovascular function and spontaneous breathing. The general considerations for practitioners to avert conscious sedation-related respiratory complications include patient evaluation and monitoring competency, knowledge of pharmacology of drugs – dosing and side effects – and skills in airway management.
Patient Evaluation
- History/physical exam – vitals & heart/lung auscultations;
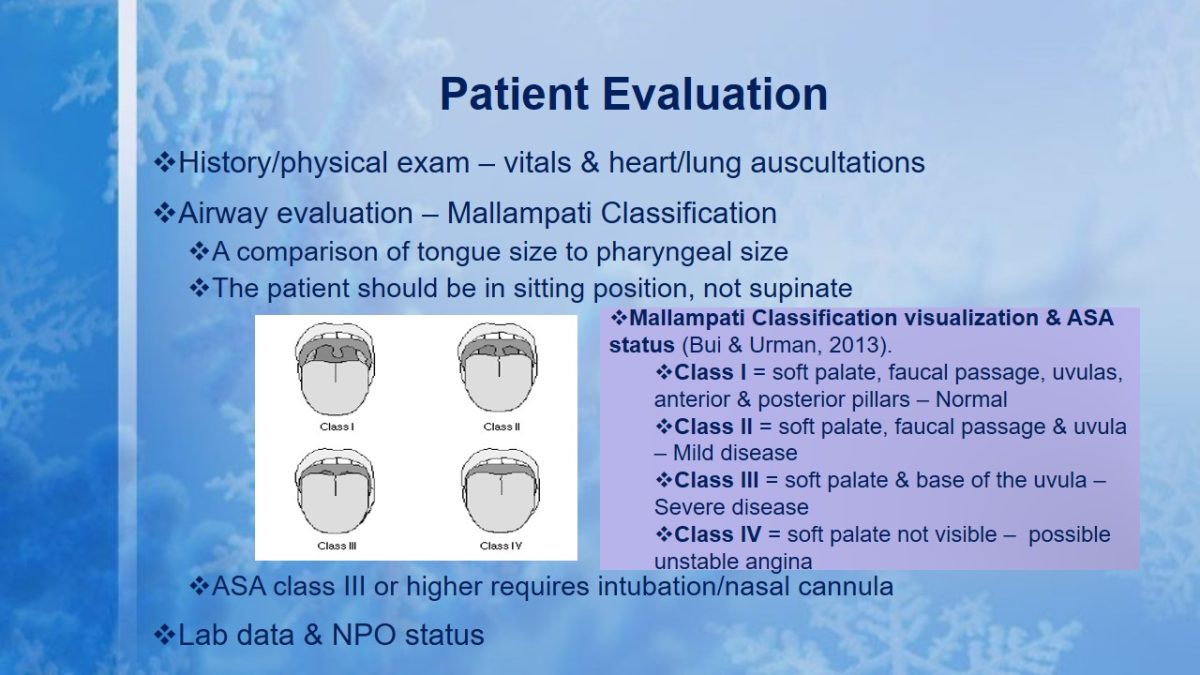
- Airway evaluation – Mallampati Classification:
- A comparison of tongue size to pharyngeal size;
- The patient should be in sitting position, not supinate;
- Mallampati Classification visualization & ASA status (Bui & Urman, 2013).
- Class I = soft palate, faucal passage, uvulas, anterior & posterior pillars – Normal;
- Class II = soft palate, faucal passage & uvula – Mild disease;
- Class III = soft palate & base of the uvula – Severe disease;
- Class IV = soft palate not visible – possible unstable angina.
- ASA class III or higher requires intubation/nasal cannula.
- Lab data & NPO status.
Patient evaluation before and during the procedure is the standard practice in sedation. It entails a focused physical exam to check vitals and lung/heart auscultations, airway evaluation, a patient history review, e.g., failed sedations, identifying drug allergies, determining the preoperative NPO status, and lab tests. The Mallampati Classification determines the ASA risk of the patient. It involves comparing the size of the tongue to that of the pharyngeal. A better view of the airway passage is obtained when the patient is seated, not when in a supine position. The ASA class III and IV are indications for intubation to prevent respiratory complications, e.g., unstable angina.
Pre-procedure Preparation & Monitoring
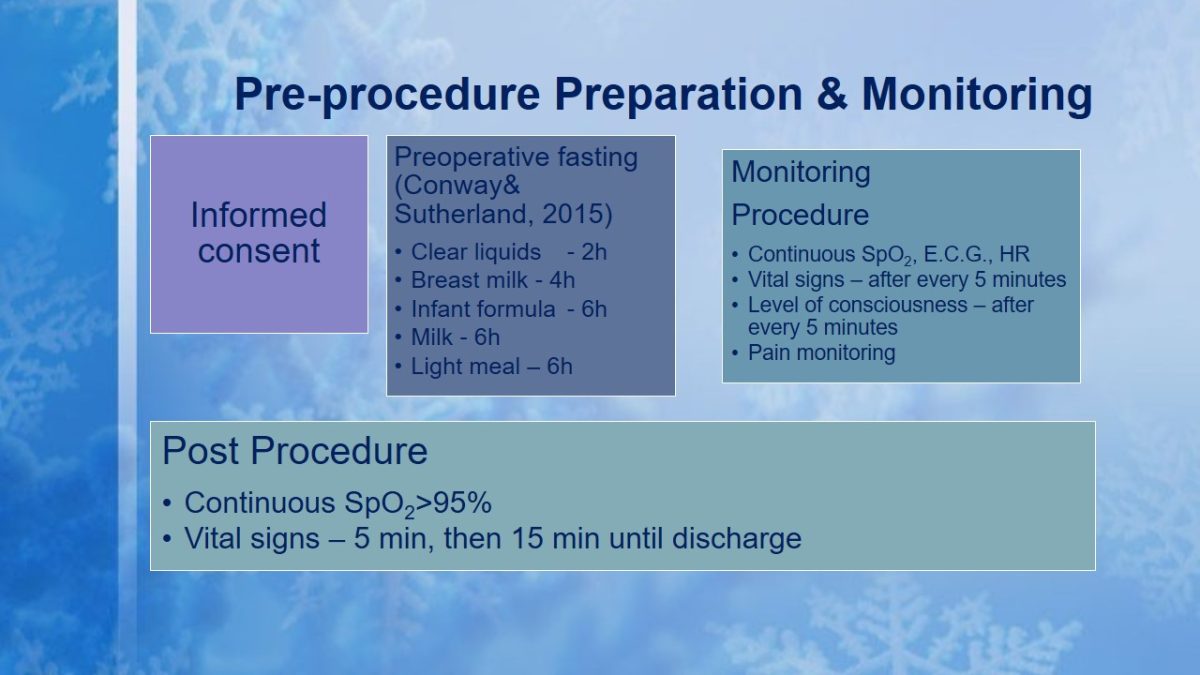
- Informed consent:
- Preoperative fasting (Conway& Sutherland, 2015):
- Clear liquids – 2h;
- Breast milk – 4h;
- Infant formula – 6h;
- Milk – 6h;
- Light meal – 6h.
- Monitoring Procedure:
- Continuous SpO2, E.C.G., HR;
- Vital signs – after every 5 minutes;
- Level of consciousness – after every 5 minutes;
- Pain monitoring.
- Post Procedure:
- Continuous SpO2>95%;
- Vital signs – 5 min, then 15 min until discharge.
- Preoperative fasting (Conway& Sutherland, 2015):
Adequate information at an early stage regarding conscious sedation should be provided when seeking patient consent. All patients, except infants, should be fasted prior to conscious sedation. The fasting guidelines vary depending on the type of food ingested, e.g., clear liquids would require a 2-hour fasting before a radiological procedure. Pre-, intra-, and post-procedure patient monitoring and documentation is vital. Baseline data on vital signs, SPO2, and pain are obtained before the procedure. The intra-procedure stage involves monitoring the vital signs, HR, SPO2, and CO2 (capnometry) after every five minutes. The post-procedure monitoring of these parameters is done after every 15 minutes until the patient meets the discharge criteria.
Equipment Required
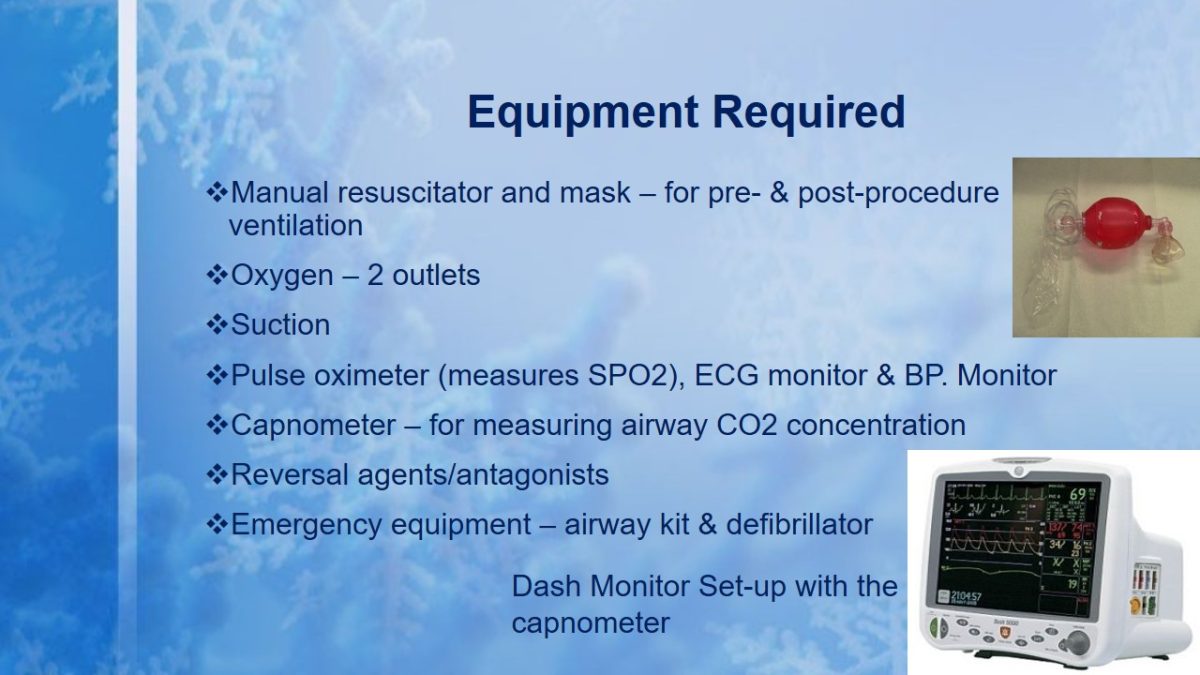
- Manual resuscitator and mask – for pre- & post-procedure ventilation.
- Oxygen – 2 outlets.
- Suction.
- Pulse oximeter (measures SPO2), ECG monitor & BP. Monitor.
- Capnometer – for measuring airway CO2 concentration.
- Reversal agents/antagonists.
- Emergency equipment – airway kit & defibrillator.
The equipment is required for monitoring of the vital signs, SPO2, level of consciousness etc. and for resuscitation. Only MRI-compatible monitoring equipment can be used in a radiology department to avoid MRI machine malfunction. The nurse practitioner must understand the monitoring equipment and parameters.
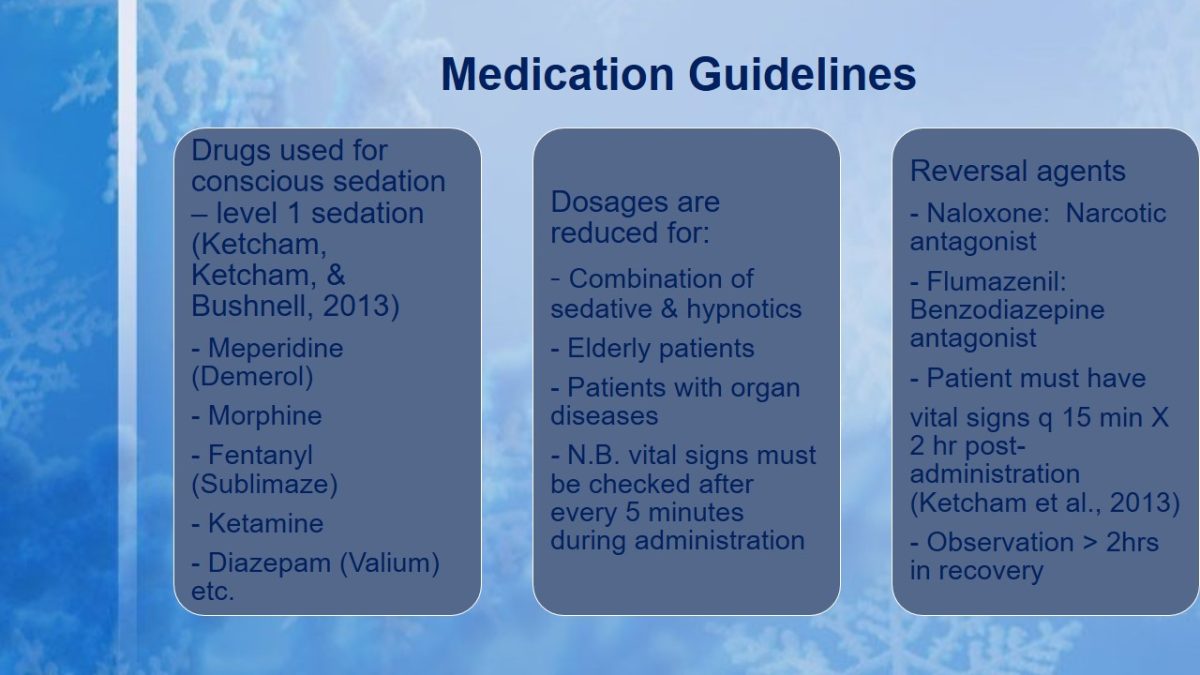
Medication Guidelines
- Drugs used for conscious sedation – level 1 sedation (Ketcham, Ketcham, & Bushnell, 2013):
- Meperidine (Demerol).
- Morphine.
- Fentanyl (Sublimaze).
- Ketamine.
- Diazepam (Valium) etc.
- Dosages are reduced for:
- Combination of sedative & hypnotics;
- Elderly patients;
- Patients with organ diseases;
- N.B. vital signs must be checked after every 5 minutes during administration.
- Reversal agents:
- Naloxone: Narcotic antagonist;
- Flumazenil: Benzodiazepine antagonist;
- Patient must have vital signs q 15 min X 2 hr post-administration (Ketcham et al., 2013);
- Observation > 2hrs in recovery.
A number of drugs are recommended for level one sedation (minimum to conscious sedation). Examples include meperidine, morphine, and diazepam. The dosages are reduced when the sedatives are combined with hypnotics and in cases involving elderly patients or those with debilitating illnesses. Antagonistic agents, such as naloxone and flumazenil, are recommended for reversing over-sedation. However, the patient must be observed for over 2 hours after taking the last dose.
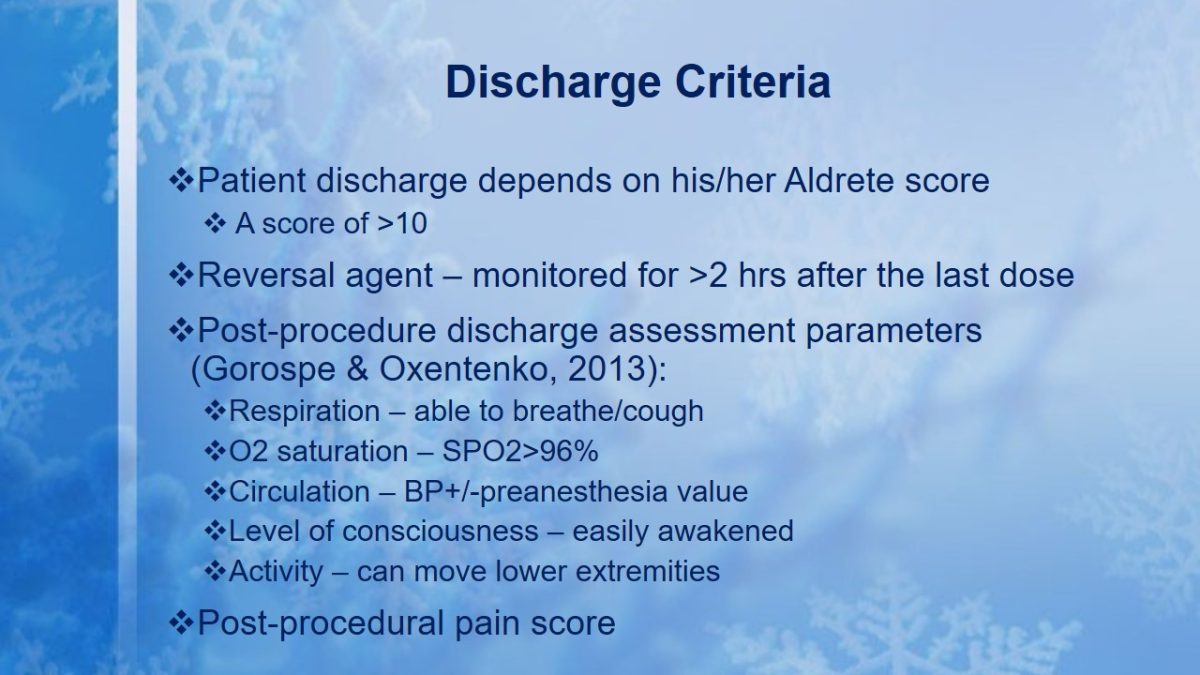
Discharge Criteria
- Patient discharge depends on his/her Aldrete score
- A score of >10
- Reversal agent – monitored for >2 hrs after the last dose;
- Post-procedure discharge assessment parameters (Gorospe & Oxentenko, 2013):
- Respiration – able to breathe/cough;
- O2 saturation – SPO2>96%;
- Circulation – BP+/-preanesthesia value;
- Level of consciousness – easily awakened;
- Activity – can move lower extremities.
- Post-procedural pain score.
The post-procedure discharge criteria for the patient considers his/her Aldrete score in four parameters, namely, respiration, oxygen saturation, circulation, level of consciousness and activity. Only patients with a score of more than 10 and low pain levels should be discharged.
References
Bui, A., & Urman, D. (2013). Clinical and safety considerations for moderate and deep sedation. Journal of Medical Practice Management, 29(1), 35-41.
Conway, A., & Sutherland, J. (2015). Depth of anesthesia monitoring during procedural sedation and analgesia: A systemic review protocol. Systematic Reviews, 4, 70-81.
Fencl, J. (2016). Guideline implementation: Moderate sedation/analgesia. Association of Peri-operative Registered Nurses Journal, 103(5), 501-511.
Gorospe, E., & Oxentenko, A. (2013). Preprocedural considerations in gastro-intestinal endoscopy. Mayo Clinic Proceedings, 88(9), 1010-1016.
Ketcham, E., Ketcham, C., & Bushnell, F. (2013). Patient safety and nurses’ role in procedural sedation. Emergency Nurse, 21(6), 20-24.