Definition of MRSA
The Acronym MRSA stands for meticillin resistant staphylococcus aureus. This is a type of bacteria that is sensitive to antibiotic treatments that usually colonizes the nose, throat and the skin of a patient. This type of infection is resistant to antibiotics such as methicillin, amoxicillin and penicillin (Lonnen , 2010).
MRSA infections have been known to occur in hospitals amongst patients who have undergone surgery or are experiencing suppressed immunity. It also occurs in patients who have stayed in the hospital for an extended period of time.
MRSA hospitalization statistics
According to healthcare cost and utilization project (HCUP) statistics, MRSA hospitalizations were more than likely to occur in the ICU (57%), between hospital transfers (5.9%), or between transfers from long term care settings to normal hospital settings (4.4%).
The number of people who were discharged with MRSA infections in 2004 were 0.7% with people who were 65 years and over recording the highest prevalence rates of 44%.
The top two procedures that led to MRSA infections included surgical treatment of skin infections and skin grafting (Elixhauser & Steiner, 2007).
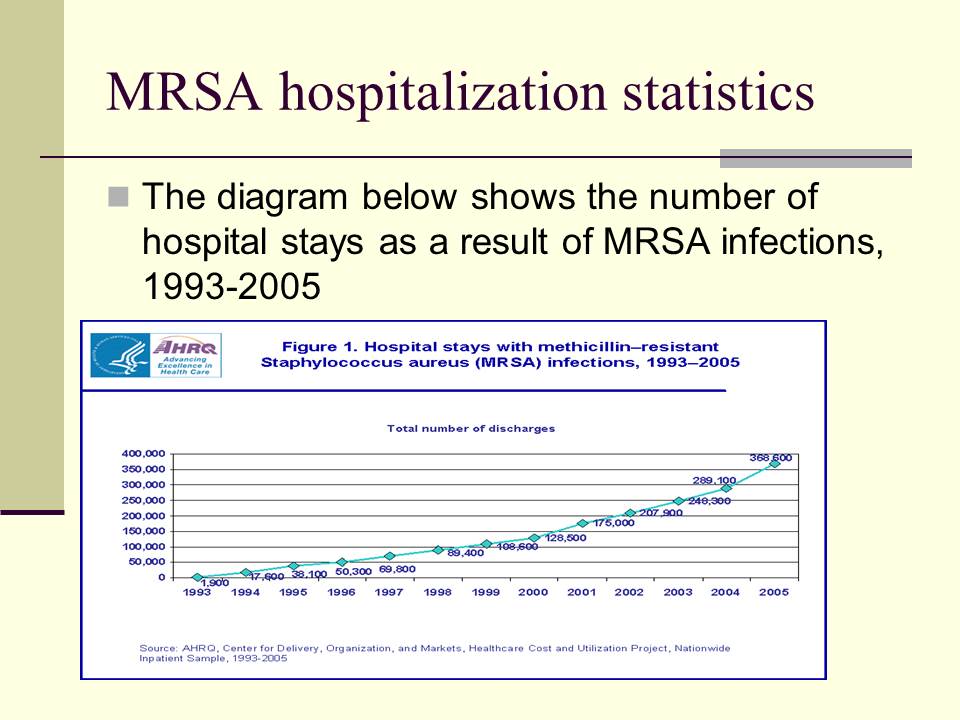
The diagram below shows the number of hospital stays as a result of MRSA infections, 1993-2005.
Identification of the Problem
Overcrowding and understaffing in hospitals has increased the level of MRSA infections. These have been identified to be the root causes of HA-MRSA (Hospital associated MRSA).
Overcrowding and understaffing increased the levels of HA-MRSA because of poor hand hygiene, isolation programs and poor patient screening.
Community associated MRSA (CA-MRSA) is also a major problem in the US where individuals are exposed to the predisposing factors of the disease outside the hospital setting (Li et al, 2009)
MRSA infections mostly occur in hospitals and health care facilities such as dialysis centers and nursing homes (Science Daily, 2008).
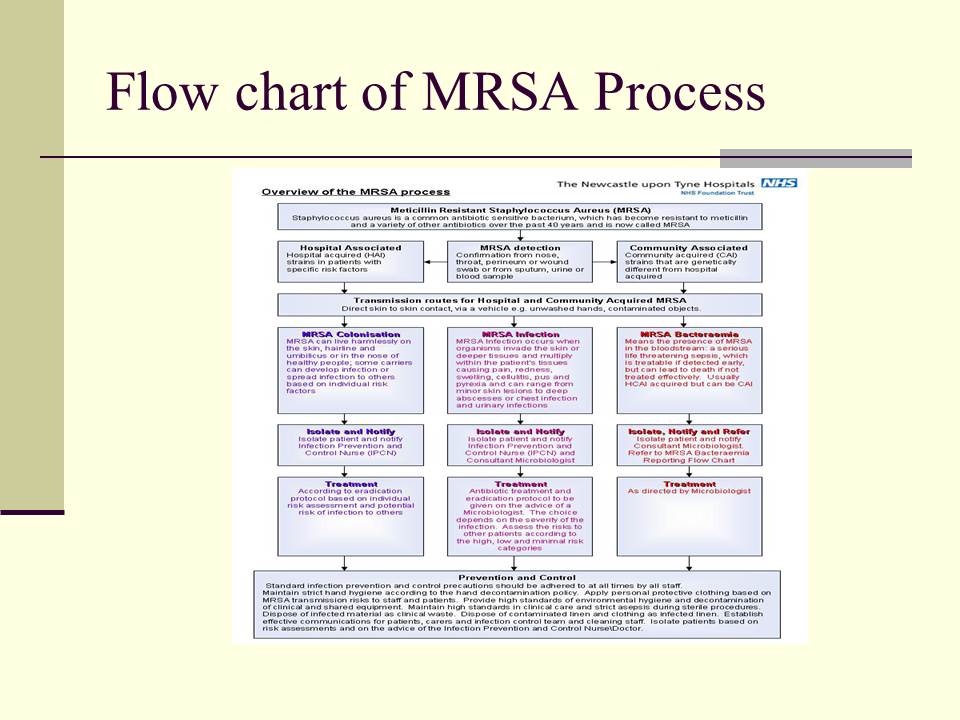
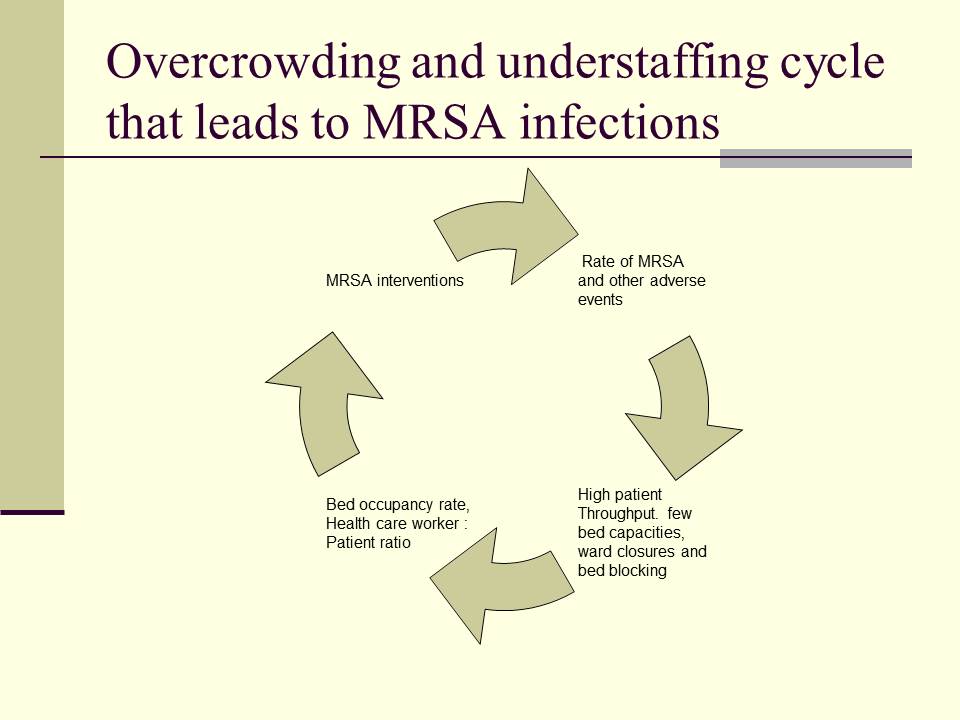
Flow chart of MRSA Process
Root Cause Analysis: What led to the increase in MRSA infections
The reasons for the increase in MRSA infections in hospitals has been attributed to overcrowding and understaffing in hospitals.
This has led to extended inpatient hospital stays, overcrowding in hospital wards and bed blocking which increases MRSA infections.
Overstaffing and overcrowding led to MRSA infections due to poor hand hygiene, number of contacts between healthcare workers and patients and staff burnouts (Science Daily, 2008).
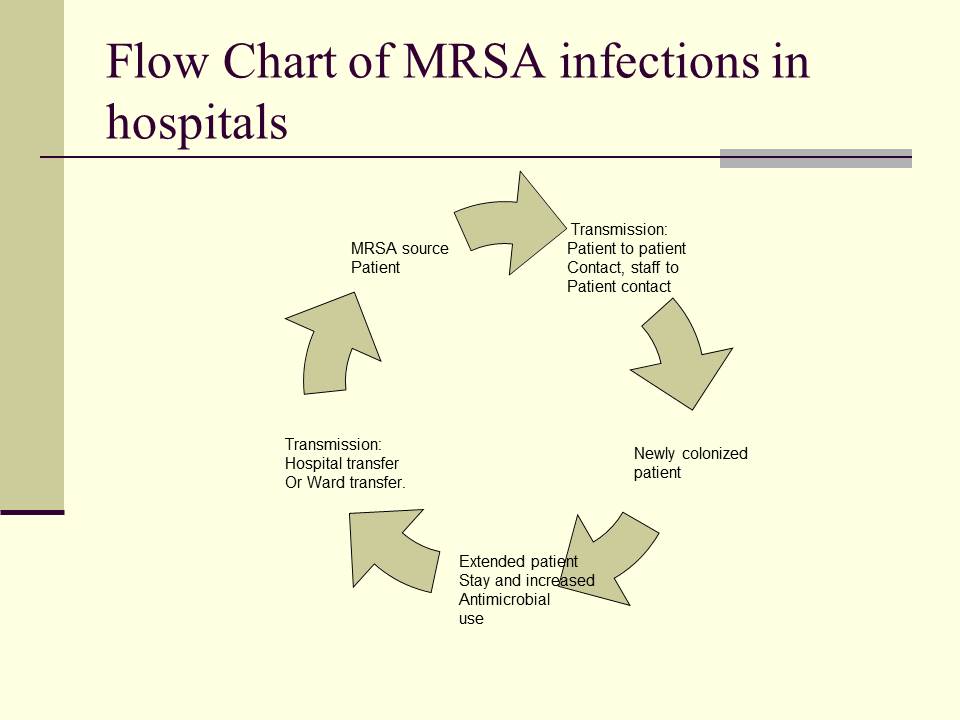
Flow Chart of MRSA infections in hospitals
Root Cause Analysis: What leads to the increase in MRSA infections
Overcrowding and understaffing in hospitals has been identified by most medical practitioners to be the root cause of MRSA infections.
These causes have mostly been related to policies that promote high patient throughput and a fewer bed capacities.
The increase of MRSA infections has also been attributed to a diminishing healthcare workforce in both hospital and healthcare facilities (Science Daily, 2008).
Overcrowding and understaffing cycle that leads to MRSA infections
Proximate Factors in MRSA infections
The proximate factors that lead to MRSA infections in hospitals include high bed occupancy rates which prevent MRSA control practices, rapid patient turnover in hospital wards or ward transfers
Periods of understaffing in hospitals have also contributed to the transmission of MRSA. The increased staff workloads increase the risks of transmitting the disease to other patients where one staff worker is allocated to a high number of patients. According to studies, the health care worker to patient ratio has a direct relationship to MRSA infection rates.
High nurse and patient interactions also contribute to MRSA infection rates in hospitals. Nurses who fail to practice safe hand washing are more than likely to increase the prevalence rate of MRSA in hospitals (Dailey et al, 2005).
The risk, human, external and equipment factors associated in acquiring MRSA infections
The factors that are most likely to increase risk of patients acquiring either HA-MRSA OR CA-MRSA include hospitalization in the past one year, a recent surgery or trauma, diabetes, kidney dialysis, frequent antibiotic use, incomplete antibiotic dosages, chronic wounds, skin diseases such as Dermatitis and Eczema and ulcers (Lonnen, 2010).
Equipment factors that increase the rate of MRSA in patients include percutaneous endoscopic gastrostomy (PEG) tubes which are used for gastric feeding, and long term urinary catheters, traction tubes and other body invasive devices that have been used for extended periods of time. These devices increase MRSA colonization in the patient increasing the rate of MRSA infections (Lonnen, 2010).
The human factors that led to MRSA infections include high hospital or ward transfers, poor hand washing practices in the hospital, poor health practices in the community, low HCW: Patient ratios, high health care worker to patient contact rates and cohorting with infected patients (Clements, 2008)
The external factors that increase MRSA infections in hospitals include the changing healthcare systems around the world, fluctuations in patient admission, low bed capacities in public hospitals, increasing healthcare costs, decrease in quality services and healthcare delivery as a result of MRSA root causes.
Systems and processes that underlie the proximate factors
The restructuring of the health system in the US has led to a decrease in the number of patients that are treated in one day. The changing structure of the US healthcare system has changed due to economic rationalization and increased efficiency (Klevens et al, 2007).
Such a situation has created a high throughput system that has resulted in high patient admission rates which have in turn led to periodic overcrowding and low health care worker to patient ratios. The throughput system has a limited capacity to deal with fluctuations in patient admissions and staff numbers (Clements et al, 2008).
The ageing trends in the US have also contributed to nursing shortages in nursing homes and other health care facilities around the country. The US and other high income countries face staffing shortages in the healthcare sector which affects the quality of healthcare and patient safety in hospitals (Klevens et al, 2007).
The number of same day separations have also gone down where the number of patients who leave the hospital the same day they have been admitted has gone down.
Controllable environmental factors
The controllable factors that directly lead to high incidences of MRSA in hospitals include, low healthcare worker to patient ratios, poor hand washing practices by health care workers, poor health care services as a result of understaffing and increased patient workloads, frequent staff rotations in hospital wards, poor nursing skills, and poor hand hygiene compliance by healthcare workers (Clements, 2008).
Areas that have been affected by MRSA infections
The areas that have been most affected by MRSA infections include hospitals, community facilities such as recreational facilities, gyms and sports centers, prisons, schools and colleges, animal shelters, cattle ranches, livestock farms and hospital nurseries.
Human Resource Issues that have led to MRSA prevalence rates
The composition of the nursing staff and their work skills has been associated with MRSA infections. Health care workers who do not usually work in a particular unit within the hospital are more than likely to increase MRSA prevalence rates among patients since they are not accustomed to the workings of the hospital ward (Clements et al, 2008).
Healthcare workers who are frequently moved between units or hospitals also increase MRSA infections.
Human resource issues that have emerged due to understaffing have resulted in nursing assistants replacing nurses in most hospitals. This has been done to decrease the rising healthcare costs in the US. This strategy has also reduced the proportion of full time staff in most public hospitals.
Poor hand washing practices by most nurses and healthcare workers in hospitals has also had an impact on the MRSA infection rates in hospitals and healthcare facilities (Clements et al, 2008).
How did authentic staffing measure up to with ultimate levels?
The understaffing in hospitals and healthcare facilities differed from the ideal levels of staffing where the healthcare worker to patient ratio was below 2:2.
Hugonnet et al (2007) note that a quarter of HA-MRSA infections can be avoided if the nurse to patient ratio is more than 2:2 especially in the intensive care units.
Such differences in the ideal staffing levels lead to increases in health care acquired infections (HAI) such as MRSA infections.
They further noted that there was growing evidence that low nurse staffing in hospitals and healthcare facilities led to poor quality in healthcare delivery and patient care (Hugonnet et al, 2007).
Plans for dealing with staff contingencies in hospitals
Nurses and other healthcare workers are in high demand in the US and they have become increasingly important in the provision of primary healthcare in hospitals and healthcare facilities.
Estimates have shown that there will be more than 110,000 clinically active nursing practitioners and physicians in the US in the next five years. This number will represent one-sixth of the total number of medical providers in the country.
The plans that have been developed to respond to the low staffing levels in hospitals include a reduction of tuition fees for people training in any healthcare profession, the use of foreign trained nurses in most public hospitals so as to reduce the understaffing pressure, and the development of computerized treatment protocols (Sultz & Young, 2010).
Level of analysis of the root causes of MRSA
Orientation and in-service training can be improved in hospitals and healthcare settings by training healthcare workers on MRSA transmission, infection rates and how they can prevent the transmission of the disease between patients. Every healthcare worker should be provided with basic information on MRSA and its causes in the hospital setting
There has been poor communication on MRSA and infection rates among healthcare workers in hospitals and healthcare facilities. The amount of information that is available on MRSA is also limited which leads to poor hand hygiene and healthcare practices.
There is also poor communication of MRSA aspects to patients who have been hospitalized or in healthcare facilities such as nursing homes. This creates a situation where patients who have MRSA interact with patients that don’t have MRSA increasing the prevalence rates of the disease.
The physical or external environment has also affected the infection rates of MRSA especially in the community setting where there are many drug users and there are many people who have skin infections in a certain location (Lonnen, 2010).
The infection rates in the community have also been increased amongst people who share clothing or personal equipment, people who have poor standards of hygiene and people who have been in close contact with an infected person.
There are systems that have been put in place to identify and respond to the environmental risks of MRSA. One system that has been identified is the serious untoward incident (SUI) that is used in reporting cases of MRSA in the community. Other systems that are in use in detecting environmental risks of MRSA include patient and staff screening, MRSA surveillance, risk assessment and root cause analysis of MRSA (Lonnen, 2010).
Leadership issues: Corporate culture and communication priorities
The corporate culture that exists in most hospitals in the US does not provide a conducive environment for the detection of MRSA or other HAI infections within the hospital. Management only becomes involved once the infection rates become too high and cannot be contained.
Healthcare providers such as doctors and physicians do not feel comfortable approaching hospital managers on health related matters because of their lack of expertise. This has created a barrier in communication especially when it comes to the potential risk factors of MRSA.
To deal with uncontrollable factors such as changing healthcare systems and increase in healthcare costs, hospitals and healthcare facilities should develop policies that will be able to adapt to these changes in both the present and future setting.
Action plan risk reduction strategies measures of effectiveness
Action item 1: To reduce the prevalence rates of MRSA in hospital, the following actions need to be taken:
- Rigorous screening of new admissions with particular focus on infected skin, nose and open sore wounds.
- Isolation of high risk patients or patients infected with MRSA
- Hand hygiene practices and training amongst healthcare providers.
- Creating awareness of MRSA and increasing information on personal hygiene
- Hand decontamination where staff and patients decontaminate their hands before they enter and leave a clinical area
- Proper waste and laundry disposal where contaminated hospital equipment and patient clothing is properly disposed off.
- The use of personal protective equipment.
The associated measure of effectiveness will be the number of people who are infected with MRSA before and after being admitted to any hospital or healthcare facility.
Action item 2: A decision to develop strategies for overcrowding and understaffing in hospitals will be impossible to make given the unpredictable nature of the healthcare system in America:
- The increasing insurance and healthcare costs will make it difficult for public hospitals to acquire more staff to deal with the increasing number of patients who cannot afford private health care and medical cover.
- The poor wages and benefits that are given to healthcare workers who are based in public hospitals is very low when compared to health care staff who work in private healthcare institutions and facilities.
Action item 3: The selected measure of effectiveness will be appropriate in measuring the prevalence rates of MSRA infections in hospitals and healthcare facilities as it will provide the appropriate statistics and number of people who have been infected with MRSA in both the hospital and community setting.
Action item 4: Pilot testing of planned improvements and reduction strategies should be conducted in the form of developing MRSA policies that will be communicated to healthcare staff and patients. Training programs will also be conducted with particular focus on hand hygiene practices. These programs and policies will be used in monitoring the MRSA prevalence rates within the hospital setting.
Action item 5: Improvements will be implemented in all private and public hospitals, health care facilities such as nursing homes, special care facilities and children’s homes, schools, prisons, athlete centers, livestock farms, community recreational centers and animal shelters.
Conclusion
It is important for all hospitals and healthcare providers to practice safe medical procedures to reduce the incidences of MRSA in hospitals.
Public healthcare hospitals need to work in conjunction with the government to deal with the issue of overcrowding and understaffing in these hospitals.
The root causes of overcrowding and understaffing in these hospitals need to be dealt with so as to develop strategies that will be used in managing MRSA infection rates.
The proponents that are used in changing healthcare systems need to consider quality healthcare and the burden of their actions to the healthcare workers.
References
Clements, A., Halton, K., Graves, N., Pettitt, A., Morton, A., Looke, D., & Whitby, M., (2008). Overcrowding and understaffing in modern health-care systems: key determinants in meticillin-resistant staphylococcus aureus transmission. Lancet Infectious Diseases, Vol., pp 427- 434
Dailey, L., Coombs, G.W., & O’Brien, F.G., (2005). Methicillin-resistant Staphylococcus aureus, western Australia. Emergency Infection Diseases, Vol.11, pp 1584-1590.
Elixhauser, A., & Steiner, C., (2007). Infections with methicillin-resistant staphylococcus aureus (MRSA) in U.S. hospitals, 1993-2005, Web.
Hugonnet, S., Chevrolet, J.C.,& Pittet, D., (2007). The effect of workload on infection risk in critically ill patients. Critical Care Med, Vol.35, No.1, pp76–81.
Klevens, R.M., Morrison, M.A., & Nadle, J.,(2007). Invasive methicillin-resistant Staphylococcus aureus infections in the United States. Journal of American Medical Association, Vol. 298, pp1763–71.
Li, M., Diep, B.A., Villaruz, A.E., Braughton, K.R., Jiang, X., DeLeo, F.R., Chambers, H.F., Lu, Y, & Otto M., (2009).Evolution of virulence in epidemic community-associated methicillin-resistant Staphylococcus aureus. PNAS, Vol.106, No.14, pp 5883-5888.
Lonnen, S., (2010). Policy for the prevention and control of meticillin resistant staphylococcus aureus (MRSA), Gloucestershire NHS Primary Care trust.
Science Daily (2008). Overcrowding And Understaffing In Hospitals Increases Levels Of MRSA Infections. Web.
Sultz, H.A. & Young, K.M., (2010). Healthcare USA: understanding its organization and delivery. Massachusetts, US: Jones & Bartlett Learning.