Introduction
In a normal marketplace, there is always a supplier and buyer. The buyer creates demand, and the supply creates the supply. Therefore, I will define demand and supply in relation to the services offered by non-profit.
Demand means the willingness and ability of buyers to pay for different services at different fees during a specific period.
Determinants of Demand for nursing services
There are a number of factors that affect the demand for nursing services and nursing aides, in turn affecting nursing homes. This includes
- salaries, wages, benefits, including starting salaries and trends in salaries in a particular nursing home or those offered by the government.
- Job vacancies in other institutions other than nursing homes.
- job turnover rates in a particular nursing home.
- Information on staffing patterns in nursing homes.
- staff workload in nursing homes.
- number of patients who visit nursing homes.
- functional characteristics in nursing homes.
- More information on how employers meet minimum direct care staffing requirements in terms of the mix of staff providing direct care.
- Information on direct care staffing and patient acuity mix.
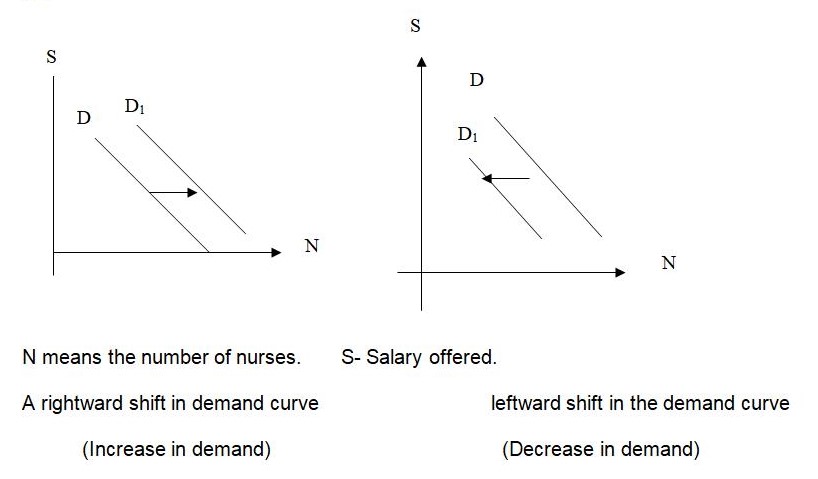
Changes in Demand, Shifts in demand curves
The demand for nurses can increase or decrease. The demand for nurses increases if more patients are visiting health facilities and able to meet the set requirements. The demand for nurses decreases if patients are few. The number of nurses will increase as the salary increases. The demand curve for the nurses will shift to the right. If the salary of nurses comes down, then the demand curve will shift to the left.
Supply means the willingness and ability of the nurses and public to train and work at nursing homes at different salaries during a specific time.
Determinants of Supply of nursing staff
- Information about characteristics of training programs thus type of program, location of the program, cost of the program, trends in the number of training programs, trends in student applications, enrollments to these programs, trends in student dropouts/reasons for dropout, how many students complete programs, how many apply for certification, how many are certified, where students are placed
- Information about the characteristics of students in training programs, i.e., age, race/ethnicity, gender, primary language, interest in entering a program, special interests, and residence
- Information about the characteristics of the workforce.
- Information about the characteristics of the actively employed workforce, i.e., number in the workforce, age, race/ethnicity, gender, primary language, nursing home setting, work history, how long workers stay in one position, reasons for leaving, where do they go if they leave position.
- Policies from various government departments.
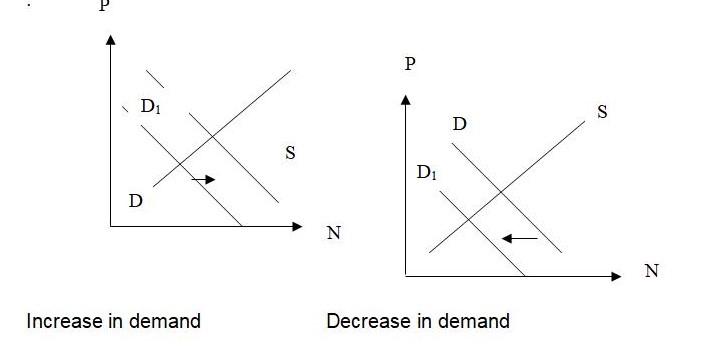
Equilibrium
Equilibrium is a situation where supply and demand are in balance. The point where the supply curve and demand curve intersect is the market’s equilibrium. The salary at this point is the equilibrium salary, and the number of nurses working for the homes is the equilibrium number of nurses. Equilibrium salary is the relative salary at which the nurses required equals the nurses working.
Equilibrium can only change if there is a change in one of the demand or supply conditions or both.
- An increase in demand will raise the Pay for nurses and increase the number of nurses training and working.
- A decrease in demand will lower the price and reduce the number of nurses training and working.
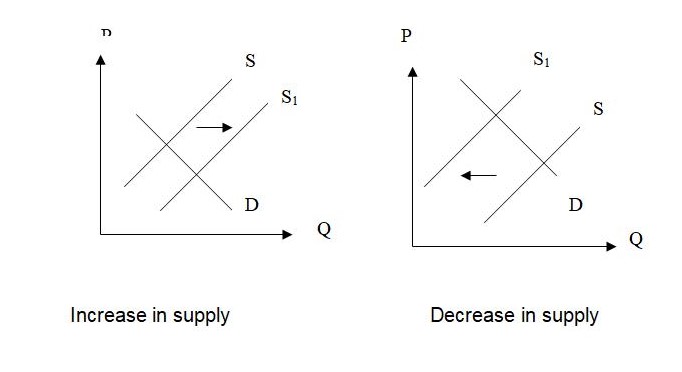
A Change in Supply with demand held constant
- An increase in a number of the number of nurses will lower the pay.
- A decrease in the number of nurses training and working will increase the pay and attract people from other parts of the world.
Market forces
Non-profit nursing homes are facing challenges from profit-making institutions that are coming up. The role and the determinants for these homes in the changing market are consumer expectations, and the government’s ability to pay for this level of care will be discussed in this section.
‘’To some extent, market forces have been brought to bear on long-term care facilities. While no one ever looked forward to moving into a nursing home, for decades, it was the only alternative to receiving support from family in the person’s own home. That scene has changed drastically over the past 20 years. A full spectrum of supportive community-based care is now a part of today’s long-term care system. Well, almost. The array of services still varies from one part of the state to another, and access to those services is not uniform. In addition, those who will rely upon public payment for care remain disadvantaged. Even access to nursing home care (certainly the choice of the facility) is not always readily available for the poorer consumer.
Private enterprise has responded to this shift towards community care and away from institutions by building and developing other living arrangements, including assisted living group homes and apartments with available support services. This explains the willingness of nursing home operators to close their doors as their attention is directed elsewhere. Even county governments are moving away from their 150-year history of providing institutional care.
The state government is deeply in debt. The Medicaid program is one of the state’s largest expenditures, and nursing home care is the largest obligation within this part of the state budget. Very modest inflationary adjustments in payment to homes translate to annual multi-million dollar budget increases. To slow those rising costs government began investing in community-based systems some 20 years ago. Consumers and their advocates are pleased. The market has shifted gears and now embraces assisted living.
Consumers’ expectations
Residents and prospective residents of today’s nursing homes expect, first, a safe place in which they can receive expert, competent medical and nursing services. It is anticipated that the care available in these settings will be superior to that available through in-home providers and will have the widest variety of possible alternatives.
Notwithstanding the expectation of many in the consuming public, the last twenty years have seen a remarkable improvement in the overall quality and availability of community-based services. Although the quality of community-based services in many regions has improved, there remains no guarantee of service variety and quality between the different types of providers. Further, regulation of in-home and other community services is minimal by comparison to nursing homes.
In nursing homes, there is a pronounced gap between the rate of payment by residents who finance their care privately and those who rely on government sources. Residents and their families are frequently completely unaware that this disparity exists, due in large part to the requirement by regulation that there be no differential in the quality and availability of basic services. The difference in reimbursement has required facilities to engage in “cost-shifting,” which adds to the cost to private pay residents to make up for the lack of complete reimbursement by the government for the care of residents using Medical Assistance. This necessarily leads to the question of whether, as the proportion of private pay residents decreases in relation to the MA residents, there will be a “critical point” at which no facility can remain fiscally sound.
Consumers tend to exercise only minimal choice in the selection of the details of their care. The choice of a long-term care provider and of particular services, therapeutics, and procedures remains most frequently influenced by families, guardians, and physicians. This results largely from the consumer’s (and, often, the family’s or surrogate’s) lack of understanding of the services offered and lack of sufficient time to choose from the available options. Concerns about quality and safety are often ignored or unnoticed. A substantial weakness is obvious in the case of residents who are summarily discharged from acute care settings with minimal discharge planning.
The lack of effective intervention and information at the time of discharge can result in inappropriate or even dangerous long-term care placements. As a rule, it can be said that homes do meet the expectations of most consumers. This is primarily a factor of the lack of awareness by the consumers of the alternatives available to the care that is offered and to the quality of services that ought to be expected care’’ Potarake, (2003).
From the above quote, the market forces for nursing homes have been identified as the government, the home’s responsibilities, and the consumer needs, i.e., the aging public.
Professionalism
From this case study adapted from the AMERICAN College of Physicians, “Increasingly, physicians are complaining that the systems in which they work do not best serve patients’ interests. Particularly when it comes to caring for patients in nursing homes, many say, the incentives seem to run counter to good medical care. As physicians, we sometimes see the shortcomings all too clearly. Although the doctor in this case study is functioning in a deficient system whose failures are self-perpetuating, a good physician must do something to try to improve such a situation. It may be difficult to decide exactly what to do, but that should not obscure the physician’s obligation to speak up and try to improve a flawed system.
To define what the physician should do to effect change, it is helpful to consider what a good system of care would look like. For one, it would be able to care for many acutely ill nursing home residents on-site, and it would encourage residents to make hospitalization and resuscitation plans. In addition, hospital care for this population would cause fewer iatrogenic complications, and the payment system would not punish nursing homes for providing acute care for their patients.
With that in mind, there are several steps the physician can take when faced with this kind of situation:
- One possible approach would be to go to nursing home administrators and explore the idea of caring for a few of the frailest patients at the nursing home, without transfer. Physicians could use such an opportunity to see if it is possible to provide adequate care in these instances in the nursing home without running up too much of a bill.
- Another avenue is to explore having a local hospice provide on-site care. Though changes in Medicare regulations may soon alter the situation, Medicare hospice can usually be made available to nursing home residents. The hospice is paid almost the same daily rate as for patients at home, though for patients who are also relying upon Medicaid, that payment is routed through the hospice program, which then pays the nursing facility. The hospice benefit is only available when the two programs have a written agreement that meets certain requirements, so coordination and advance planning are essential.
- Talking to the emergency room medical staff and hospital administration may also yield fruitful suggestions on how to improve the care of nursing home patients. For example, the emergency room staff might welcome clarifications to routine advance directives so they can more easily understand and trust the written forms that the patient brings. The hospital might also be willing to move a nursing home resident to a regular hospital bed more quickly to limit the hazards of falls and skin breakdowns that so often occur in the emergency room. Perhaps hospital physicians could also take the lead in talking to a patient’s family about re-hospitalization for long-term chronic problems.
- Physicians could also collect data on the frequency and outcomes of situations where nursing home residents are transferred to hospital emergency rooms. It might turn out, for example, that the problem transfers are mostly confined to one nursing home or involve patients with a particular set of conditions, and responses could be tailored to those situations. Measuring the frequency of transfers may help galvanize nursing home leadership into taking these situations seriously.
- Playing an active role in advance, care planning in the nursing home for hospitalization and resuscitation could also help to ameliorate the problem. Many patients this frail—or their families—are willing to take their chances with the treatments they can get in their nursing facility, and they should have the opportunity to make that desire known. Even those who want more aggressive treatment often have limits that they can articulate: a time-limited trial on a respirator, for example. Knowing about such considerations in advance would be helpful and would allow physicians to tailor care to the patient and family in an efficient and sensitive way.
- An even more direct tactic would be to approach the local Medicaid carrier to find out what accommodations it might be able to provide. For example, the carrier might be willing to subsidize advance care planning or care management. Physicians could also ask the local quality review organization to study the practices and possible opportunities for improvement.
Compensation and reimbursement schemes
From the information available, the workers working with nursing homes have not properly compensated. That is why they opt-out to another working environment where they are properly compensated. There should be proper compensation for Mandatory overtime.
Lack of assurance of full-time pay, Long shifts, increased patient acuity levels.
Conclusion
Concisely, in order to maintain an equilibrium level of demand and supply of workers of nursing homes, those services adequately. There should be a proper prediction of the number of health care workers required in these homes and address workplace issues such as mandatory overtime, patient and staff safety, staffing, and quality care. We also need to develop a recruitment plan for securing an adequate number of future health care professionals and enhance the image of health care careers. We should not forget the issue of compensation and another benefit for the nursing home workers. Lastly, there should be an improvement in the facilities.this will keep the nursing homes in competition with the coming up of profit-oriented.
References
Administration Bureau of Health Professions National Center for Health Workforce Analysis: Projected Supply, Demand and Shortages of Registered Nurses: 2000-2020.
American Association of Colleges of Nursing; Hallmarks of the Professional Nursing Practice Environment; Washington, D.C., 2002.
American College of Physicians Ethics Manual, 4th ed. Ann Intern Med. 1998;
American College of Physicians, (1999) Ethics case study: when it comes to nursing home dumps, should you just go along or speak up? Web.
American Hospital Association, Commission on Workforce for Hospitals and Health Systems: In Our Hands: How Hospital Leaders Can Build a Thriving Workforce, 2002.
George Potaracke, 2003 Nursing Homes and Public Policy.
Joint Commission on Accreditation of Healthcare Organizations; Health Care at the Crossroads: Strategies for Addressing the Evolving Nursing Crisis, 2002.
Povar G, Moreno J. Hippocrates and the health maintenance organization: A discussion of ethical issues. Ann Intern Med. 1988;109:419-24.
Robert Wood Johnson Foundation; Health Care’s Human Crisis: The American Nursing Shortage, Princeton, New Jersey, 2002.