Abstract
The COVID-19 pandemic, caused by a previously unknown virus of Chinese origin, significantly changed the traditional order of life. The effect of the pandemic is particularly felt in patients with kidney disease. Treatment for such patients is known to require dialysis — however, dialysis practice is more difficult in highly contagious environments. In particular, if the procedure is usually performed by filtering the patient’s blood in an office with other patients and nurses, there is a risk of mass infection if the virus is present. To eliminate the undesirable effects of coronavirus in dialysis wards, prevention protocols are used. This includes temperature control, wearing personal protective equipment, disinfection, and isolation of coronavirus patients from healthy patients with kidney disease.
An effective healthcare system is an essential criterion for maintaining national health. In particular, the overall health and mortality rates depend on how smoothly and uninterruptedly the links in the health system function. There is no doubt that all branches of modern medicine are vital to society, but while some areas are aimed at helping patients with milder diseases, others support patients with serious and critical clinical cases. In the second case, there is a significant need to create an environment in which potentially emerging external factors do not negatively impact the industry in general or medical staff and patients in particular.
In fact, many generations of politicians, decision-makers, and officials have made specific arrangements to help create a highly effective healthcare system. In the context of the United States, the most significant circumstances were the introduction of Obamacare — the nationwide citizen insurance — which was President Obama’s response to the poor performance of two programs, Medicare and Medicaid, which were established back in the twentieth century. Nevertheless, it is difficult to predict how coherent the system will be or what the result of reform will be: theoretically, politicians should always take the best possible action, but in practice, the situation may be different. Ironically, exposing all existing shortcomings in the healthcare system can be a severe threat that has gone out of control. For example, pandemics often show a lack of regular clinical outreach at the municipal level, a lack of clear instructions for emergencies, and a lack of access to timely information, that is to say, counseling and care. In general, this is only a small list of problems that exist in modern medicine that can be detected when a detailed review of the current situation is undertaken.
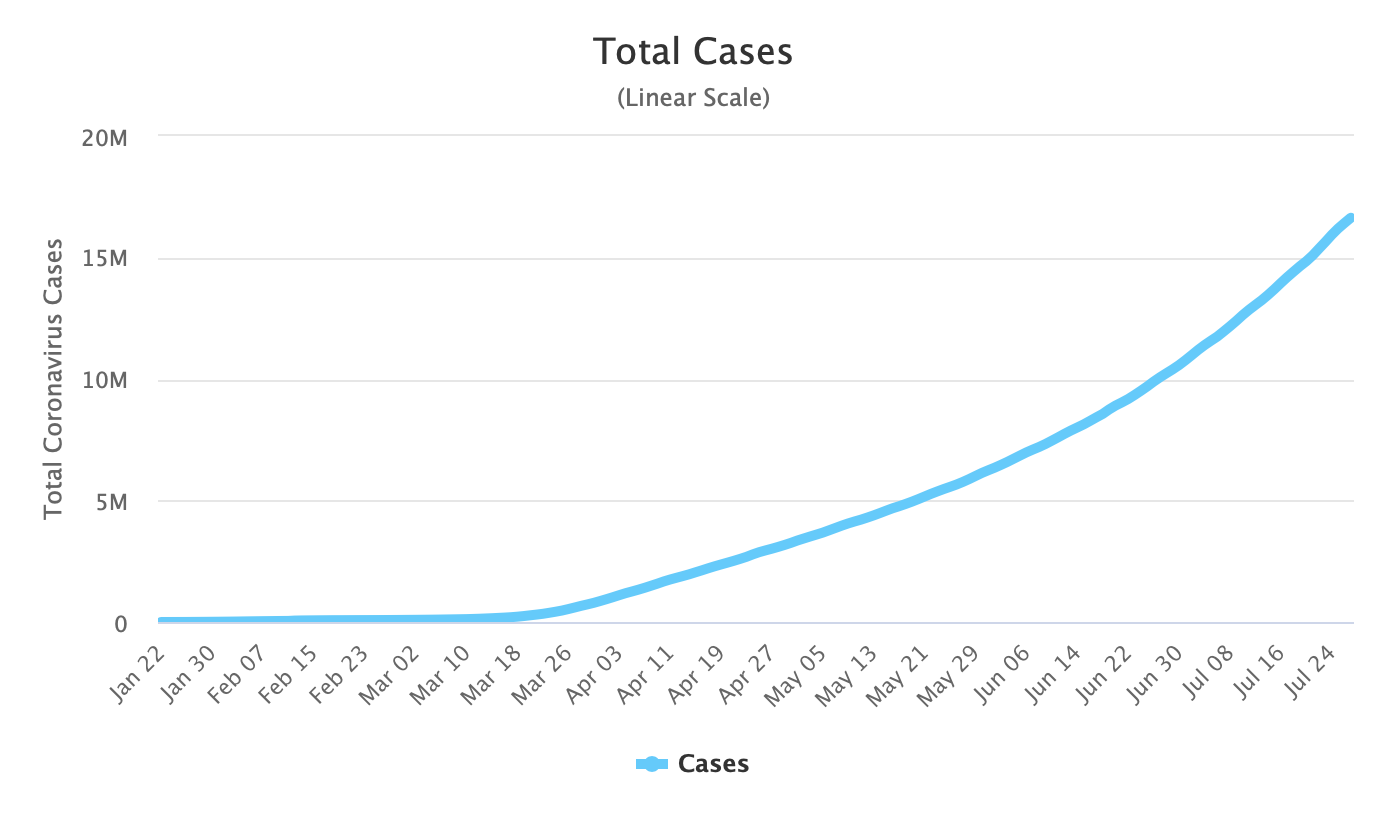
Medicine is currently experiencing serious difficulties due to pressure from a new virus. In December 2019, the first reports of a previously unknown form of coronavirus infection that mainly affected the respiratory system began to appear in a major Chinese city, Wuhan. Already in early January, the World Health Organization took over control of the situation, but even with the authority to conduct global monitoring, the organization was unable to track the movement of human flows, which led to a rapid and rapid spread of the epidemic. It is fair to say that, due to the lack of operational action and systematic observation, the World Health Organization was extremely skeptical about the new virus. However, timely recognition of the infection as a pandemic could have given the disease the necessary status and added discussability it needed. Instead, the coronavirus remained under questionable control for more than two months, although the media in almost all countries reported that new cases were being detected on their territory. The result of this policy has been an almost exponential increase in the number of new cases detected, as illustrated in Figure 1.
The infection caused by a previously unknown form of the virus was scientifically named COVID-19. Since the virus was discovered, all the forces of the world’s research laboratories have been focused on sequencing and analyzing genetic material, classification, determining how and when it can be stored on surfaces, and developing a universal vaccine. From the material collected, it is safe to say that the virus has the potential to form a severe stage of respiratory distress, suffocation, and, unfortunately, death. As of July 31, 2020, the number of deaths caused by COVID-19 had exceeded 678,957, which is 4% of the total number of infections (“Coronavirus cases,” 2020). By comparison, the number of deaths as of July 28, 2020, was 656,852, which means that more than 22,000 patients died in four days, equivalent to a 0.75% increase in one day. Without a doubt, this is a rather high figure, which, as practice shows, continues to increase with each new week. The virus is known to spread between people by inhaling the smallest liquid droplets containing the virus when a sick person coughs or sneezes. Moreover, scientists believe that the virus is also transmitted by infecting the mucous membranes. In other words, if a healthy person touches the dirty surface, such as handrails in public transport, cutlery in restaurants, or even money, and then touches the eyes, nose, or mouth with infected hands, then they have a high probability of infection. Therefore, a program aimed at promoting hygiene among the population — the wearing of disposable gloves and medical masks in public places — is a highly effective measure to contain the amount of contamination.
It should be noted that all spheres of human life have undergone severe changes due to the development of COVID-19. While healthy patients, in order to prevent the spread of coronavirus, treat their health more carefully, use personal protection measures and prefer to be at home, patients who have already been infected, feel the new rules of clinical practice. This is particularly true in the dialysis department, where it is essential to keep the premises clean and sterile. It seems necessary to recall that dialysis clinical practice focuses on medical care for patients suffering from acute and chronic renal failure. In natural conditions, a renal structural unit called nephron performs the function of filtering blood from metabolic products.
As it is known, kidneys are the paired organs of the human body that filter blood from the end products of metabolism, as well as toxic substances that have entered the body from the outside. Under natural conditions, during the filtration process, urine is formed from the blood, which is extracted from the body along with harmful substances. Moreover, the kidneys are an essential part of the endocrine system, taking part in the synthesis of certain hormones: renin, erythropoietin, calcitriol, and prostaglandins. Finally, the kidneys are involved in protein and carbohydrate metabolism.
If the natural activity of the kidneys is severely impaired, a disease called renal failure may occur. In this case, renal tissue loses the ability to perform its function sufficiently. The result of this condition is uremia — the poisoning of humans with toxic products of metabolism, failure of the acid-alkaline and water-salt balance, and as a result, disruption of all systems. In general, the causes of renal failure may be a number of factors. The most common are traumatic shock, substantial blood loss, poisoning with poisons or medical drugs, infectious diseases, and thrombosis. Moreover, failure may be caused by burns of large areas of the body, blood transfusions (if inconsistent), continuous vomiting, and myocardial infarction. Cancer formations are also known to become a factor in renal failure.
If the doctor has suspicions that the patient has renal failure, treatment should be started only after full confirmation of the diagnosis. Diagnosis usually consists of a general blood biochemical analysis, a particular study for electrolytes, creatinine, urea. In addition, it is necessary to analyze the urine and diagnostic sonography of the bladder and kidneys. It is worth recalling that this condition is a dangerous multistage disease with a high risk of lethality, which requires immediate medical intervention and strict control. Treatment of acute form requires surgical therapy by taking medication or patient’s blood dialysis. Hemodialysis practice is aimed at the filtration of the patient’s blood outside the body, in which the division of blood fractions performs a selective semi-permeable membrane. Thus, the patient’s blood, which has been purified of excess substances, is returned to the patient’s body.
The relevance and importance of this research work are dictated by the existing conditions in both the global and strictly medical environments. Hemodialysis practice dramatically simplifies the life of patients, but it is essential to remember that this area is distinguished by the need for increased sterility, as the work is done on the blood of the patient. The new coronavirus infection has the potential to significantly change the traditional activities of medical professionals since, even in such sterile rooms, there is a risk of blood infection with the virus. The aim of this work is to investigate in detail the extent to which COVID-19 infection affects conventional clinical hemodialysis practices through the lens of introduced changes in the instrumental and theoretical part of the study.
Definition of the Problem
The Link Between Coronavirus and Kidney Disease Forms
It worth noting that patients suffering from chronic kidney disease are the most vulnerable groups to COVID-19 coronavirus infection. These populations are known to have reduced immunity, so the penetration of the virus into the bloodstream can cause severe disruption of life up to death. On the other hand, according to Sperati (2020), there is also an alternative type of link: Doctor of Medicine believes that infection can cause damage to renal tissue. In other words, patients are primarily infected with the SARS-CoV-2 virus, which is the source of kidney disease. There are several possible mechanisms of this phenomenon: Sperati speaks about the direct impact of the virus on tissue, damage caused by low oxygen levels in the blood, inadequate action of the immune system, and the formation of blood clots. In general, without focusing on the causal links between renal dysfunction and coronavirus, it is particularly worth noting that the health of such patients is deteriorating in such a way that they need help from the hemodialysis department. For this reason, healthcare organizations in particular and the US Department of Health and Human Services in general need to take extraordinary measures to prevent the spread of infection among patients. However, this does not mean that the patient should postpone treatment for fear of being infected — on the contrary, a visit to a doctor is a critical factor in the likelihood of a successful outcome in therapy (Ng & Li, 2018). For this reason, in order to preserve sanitary conditions and sterility of premises, clinical organizations are introducing additional preventive measures. These include physical and social distancing, continuous temperature screening, and wearing personal protective equipment.
The Practice of the Dialysis Department
It should be further recognized that preventive measures related to the prevention of proliferation cannot be absolutely organic to the structure of the clinical organization. In particular, hemodialysis rooms traditionally have five chairs for patients, which promotes active communication and contact among patients. At the same time, the blood filtration procedure implies that the patient is helpless, chained to the chair – active contact is realized through the nurse. Nurses touch the surface of the patient’s clothes or body while the patient is connected to the device and communicates with it. It is not difficult to understand that such conditions contribute to the transmission of high contagious coronavirus infection, so hemodialysis in the clinical department needs a particularly careful approach to the organization of activities.
Lack of Employment Opportunities
Taking into account the extent of the coronavirus’s influence on the medical and economic spheres of life, it should be additionally noted that the lack of jobs is an important issue raised in this research work. As it is known, the infection affects all categories of the population, therefore, the probability of infection of nurses is present. At the same time, nurses are more likely to interact with sick patients who have a potentially viral disease but are asymptomatic. In other words, healthcare workers are a kind of risk group (Burgner, Ikizler, & Dwyer, 2020). In the case of hemodialysis workers, a collapse of the clinical system may occur when demand exceeds real supply. Absence of even a few employees, caused either by well-being or by quarantine, may lead to suspension of the department’s activity. Unfortunately, this outcome will be unfavorable for patients undergoing long-term renal replacement therapy.
PICOT Question
One of the critical skills for good clinical practice in evidence-based medicine is the ability to formulate clinical questions. Such questions are usually extremely verbose, but their proper structure allows them to be useful for health professionals. In the first place, such questions should be directly related to the relevant clinical case. Secondly, the questions should be structured so that the medical professional can find the answer to them. Thus, the correct PICOT question is a question statement that is directly related to the problem. It is different from questions asked by inexperienced specialists when the goal is to know any secondary characteristics.
For this case, standard preventative measures were established by best practices to prevent spread of COVID-19 by identifying the elements of PICOT. Then PICOT question is designed to determine if temperature assessment, symptoms of sickness, being around positive corona virus patients, and wearing a mask diminish transmission of COVID-19 between patients and staff.
Project description
- P – Dialysis center patients
- I – Assessing patient’s temperature and symptoms before contact with other patients
- C – Mask wearing, checking temps, social distancing, and performing COVID-19 screening of symptoms compared to taking no precautions.
- O – No transmission of virus between patients
- T – Immediate assessment allows for infected to be isolated from noninfected patients between every treatment.
Literary Review
The Importance of a Rapid Response by the Healthcare System for Pandemic
There is no doubt that the public healthcare system is the most critical area of public policy. By stimulating and financing the qualitative growth of scientific medical research, and investing in maintaining health indicators, the authorities are improving the domestic medical climate and making the population healthier and calmer. However, the healthcare system does not always demonstrate preparedness for non-standard situations, which becomes especially important in acute crisis conditions. It is not difficult to turn to well-known historical cases when medical organizations all over the world had difficulties in doing their work due to the global threat. For example, this is the H1N1 Swine influenza crisis, which, as far back as 2009, demonstrated little effectiveness of healthcare structures (Ungchusak et al., 2012; Stavroulopoulos, Stamogiannos, & Aresti, 2010). Eleven years later, it would seem that officials and policymakers would have had to develop prevention algorithms and stock the necessary materials for future pathogen outbreaks. Nevertheless, even with the bad experience and concrete conclusions, humanity still faces the same health problems as it did eleven years ago.
Public Healthcare Problems
An extensive segment of scientific literature is devoted to the study of modern health systems in the context of preventive measures taken to prepare for outbreaks of infectious diseases and emergency events. Burgner et al. (2020) particularly emphasize that current models show preparedness for natural and human-made crisis conditions, but are inappropriate for the development of pathogenic diseases. The reasons are a lack of regular and transparent funding, a lack of stockpiles of medical consumables, and a lack of established links between the health system. This problem is reflected in the reflections of Braithwaite (2018), which is developing the theme of radical change in the system. The author points to the non-linearity of existing models, which causes heterogeneity and unpredictability of the consequences of the measures taken. Thus, even if some reforms show effectiveness within one state, it may be unsuccessful in the territory of another one. Finally, Aye (2020), in a journalistic article, links weaknesses in public health systems and coronavirus pandemics: it points to inadequate funding and a lack of commitment among WHO leaders as factors in poor health outcomes. According to the author, if the organization had investigated the December outbreak of an unknown virus of Chinese origin more quickly, it would have been possible to contain the pandemic.
Defining a Pandemic
It is worth mentioning that a pandemic is an intensive long-term process, in which the pathogenic disease spreads over vast areas. It also means that large numbers of people are being infected within several countries, a continent, or even a planet. It is fair to say that, according to WHO (2020), there is no unambiguous and unique terminology, so it is possible to interpret this definition. In any case, it is essential to understand that this is a rather large event that has a global impact on all industries and activities, so those responsible are required to implement proportionate measures actively.
Vaccination as the Best Prevention Measure
Preventive programs are what must be implemented in crisis situations. Modern medicine claims that the most effective measure to prevent the spread of infection is vaccination. With this in mind, according to Cortese et al. (2020), vaccination traditionally refers to the introduction of a weakened pathogen into a healthy patient to stimulate the development of acquired immunity. This approach is particularly valuable in situations where seasonal outbreaks of infectious diseases can be predicted. Thus, according to Yong (2017), in the near future, humankind will learn to forecast the development of pandemics based on statistical models, but today quite often, there are epidemiological expectations, some of which become facts of actual reality. In the case of unexpected pathogens, it takes time for biotechnologists to analyze the genetic code of the virus, classify it, identify inhibiting mechanisms, and develop a vaccine. Moreover, the mass market entry of a drug also requires significant time resources (Rappuoli, Black, & Bloom, 2019). Traditionally, the full cycle of vaccine development, from the stages of academic research to mass supplies to health care organizations, takes over a year. Realizing the criticality of the coronavirus pandemic situation, the leading financial and research flows are aimed at finding a formula, but even with this effort, humanity will not get a vaccine. It is worth admitting that opinions on the end of the waiting period are highly divided. Based on scientific forecasts, Thompson (2020) writes that it will take about 18 months to get the finished drug. On the other hand, Oxford University admits that it plans to release the first developments in September 2020 (Smith, 2020). Russian researchers are trying to register the vaccine even faster – according to the news agency, by the end of August 2020, the first batch will be sold (“Russia may register coronavirus vaccine,” 2020). Taking into account the fact that the first vaccines will most likely not be universal. Most likely, the vaccine will be available to everyone and will be supplied either at the expense of the federal budget or at a small price, but one should expect that the total vaccine will not be available until 2021. In other words, in a state of COVID-19 pandemic, patients and clinics cannot count on the vaccine but must use existing prevention guidelines.
Other Prophylactic Measures
As a general rule, in the case of particularly contagious infectious epidemics or pandemics, the population is encouraged to follow some necessary measures to prevent coronavirus infection. Today, of all modern information agencies, requirements to wear disposable masks and gloves, to use antiseptic drugs, and to control their health are being implemented. In addition, in order to reduce the spread of new coronavirus infections, people are advised to wash their hands with soap for twenty seconds, avoid touching open facial surfaces with dirty hands and avoid social contact through distance. The quarantine of urban areas is an effective measure to be introduced by states in crisis situations. Researchers from Cochrane, a UK-based non-profit organization, have argued on models that quarantine significantly reduces the total number of diseases, especially if applied in conjunction with other restrictive measures – the closure of schools, kindergartens, public spaces and shopping centers (Nussbaumer-Streit et al., 2020). The past months have shown that many policymakers have listened to health experts and introduced quarantine, thereby reducing potentially high infection rates.
Dialysis Department
In this work, it was repeatedly noted that patients with chronic kidney disease are more likely to be infected with SARS-CoV-2 coronavirus. This is primarily due to the fact that kidney disease is a widespread disease that is highly correlated with diseases such as diabetes mellitus, hypertension, obesity, and atherosclerosis. These diseases are treatable in their own right at the mild stage, but failure to comply with medical prescriptions exposes the patient to the risk of complications, especially in a pandemic. Apicella et al. (2020) indicate that coronavirus causes complications in the metabolic processes of cells, which are also detrimental to the kidneys. For example, beta cells have disorders that lead to ketoacidosis: given that the kidneys are a blood filter, high levels of glucose and ketone bodies can form deposits in nephrons.
A negative factor in the association between coronavirus infection and kidney disease is the probable absence of visible signs of the disease. Zhang et al. (2020) suggest that the course of an infectious respiratory disease may be asymptomatic, meaning that a person may have a pathogen without even knowing it. This phenomenon significantly complicates the treatment of dialysis patients, as patients may be infected but not know it, and continue to attend hemodialysis sessions. As a result, the entire group of patients and nurses who have contact with the vector become potential targets for infection. This explains the difficulty in containing the spread of the pandemic and the high mortality rate among patients with kidney problems.
The fundamental dialysis practice is based on metabolism through a semi-permeable membrane washed with constant blood flow on one side and a dialysis solution on the other. This solution, additionally called dialysate, is one of the essential components of systemic hemodialysis, with which the blood is purified of uremic toxins. According to McGill & Weiner (2018), it contains sodium chloride, potassium chloride, calcium chloride, magnesium chloride, and buffer compounds to maintain the required pH level. By diffusion and ultrafiltration, dialysis removes harmful substances from the blood and delivers the right substances. Meanwhile, by adjusting the composition of the dialysis solution, the type of dialyzer, including the method and pace of blood supply and dialysis solution, specialists can replace the function of the kidneys and maintain a satisfactory condition of patients.
Traditionally, dialysis machines have three components: a blood supply device, a device for preparing and delivering a dialysis solution, and a dialyzer. The patient’s blood, which contains toxic substances, is pumped into the dialyzer via small tubes. Blood flow and pressure measuring devices are connected to this system to control the procedure. According to Burgner et al. (2020), blood flow rates of up to 450 ml/min are considered optimal. Water removal from the blood can be adjusted by changing the negative hydrostatic pressure on the dialysis solution. In addition, the intensity of water removal depends on the type of membrane.
Kidney Failure and COVID-19
Pandemic morbidity causes acute renal failure. Current medical reports indicate that 20% of patients with coronavirus infection develop acute renal failure syndrome (“Kidney disease & COVID-19,” 2020). Prevention of Acute Kidney Failure includes restoration of blood circulation, adequate analgesia, correction of acid-base and water-electrolyte balance, as well as an increase of myocardial contractility. In other words, the disease increases the patient’s need for hemodialysis, so it is crucial to create favorable conditions for medical work. However, re-profiling a number of hospitals to care for patients with COVID-19 may seriously disrupt the provision of chronic kidney diseases with systemic dialysis.
Statistics on dialysis unit attendance, procedures, and consultation suggest that coronavirus has had a severe impact on patients with non-communicable kidney diseases. According to information provided by Prasad et al. (2020), the total number of visits to Indian clinics decreased from 2,517 to 2,404. Other data also do not suggest a favorable environment – the COVID-19 pandemic did shift attention away from patients with other diseases. This effect is illustrated in Table 1.
Table 1. Statistical data on the impact of the COVID-19 pandemic on clinical practice in the dialysis ward. Relevant for India.
Evidence-Based Solution
Threat Background
There is no doubt that the current situation is unacceptable both for patients wishing to maintain their health and for workers in the medical industry who are unwittingly at serious risk of disease. In this regard, there is a clear need to change current policies and clinical practices so as to ensure safety for all parties. Patients with non-communicable kidney diseases who wish to receive dialysis services must be able to do so without falling into critical conditions of the high probability of contracting the SARS-CoV-2 virus. The fact that there is a close correlation between COVID-19 and the development of renal failure should be the basis for adequate public health policy.
On the other hand, health workers become a group of vulnerable citizens. Even if a health worker, when infected with coronavirus, carries the disease in a mild form, they still interact with family members, their parents, so that they can infect them. It is known that the mildness of COVID-19 of one person does not impose restrictions on the development of severe stages, up to Severe Acute Respiratory Syndrome in those who were infected. It is essential to clarify that it is not only the hemodialysis nurses who are at risk. A standard practice of dialysis services is accompanied by communication of the patient with the administrator at the reception, accompaniment to the procedure room, communication with other patients and nurses during hemodialysis. In addition, the room must be in sterile conditions, so clinical organizations hire staff to clean the room. As can be seen from this reasoning, at least four categories of people are at risk if a patient with asymptomatic form COVID-19 comes to the dialysis room – the administrator, other patients, nurses and cleaning staff. In practice, the situation turns out to be more multifactorial, as it is not ruled out that the patient can interact with people at the entrance to the clinic, wardrobe staff where things can be left, or relatives of elderly patients undergoing the procedure. It should be kept in mind that according to Burgner et al. (2020), a patient with renal failure visits the dialysis ward at least three times. Given the above, there is an urgent need to develop scientifically sound measures to prevent the spread of viral infection.
Description of Specific Measures to Address the Problem
The adequate solution to this problem has the property of complexity and multifactoriality. The measures taken should not target only one category of patients, but instead, focus on the equal rights of all stakeholders. Only by using the cause and effect principle can absolute health security be achieved. In the first place, this requires an understanding of the symptoms of coronavirus infection. According to the CDC, most often, the disease starts with weakness and ailments, fever, and dry cough (“Symptoms of Coronavirus,” 2020). Some people may have muscle and joint pains, stuffy and runny nose, pharyngitis, or diarrhea. Often, these symptoms develop gradually and appear rather poorly. It is worth noting that the majority of cases occur easily, with only mild sickness and low fever. Some infected people do not develop any symptoms or ill health at all. Nevertheless, unlike many other respiratory viruses, coronavirus attacks the lower respiratory tract — that is bronchi and lungs — more often, causing pneumonia and respiratory failure, which is the cause of death in at-risk patients. That is why the fever is the primary marker for determining the presence of the virus in the body. For this reason, regular temperature screening of patients at the entrance to the dialysis ward should be the primary preventive measure.
Implementation
Temperature Control
The implementation of temperature control should be carried out in such a way that it does not cause significant discomfort to patients and healthcare professionals. The use of mercury or electronic thermometers does not seem appropriate due to long waiting times, physical contact with the skin surface, and contact when transferring the device from patient to clinic employee. For this reason, the use of pyrometers – contactless thermometers — becomes a real solution, the main advantage of which is quick results. The principle of operation of the device is based on measuring the thermal radiation power of the body, mainly in the ranges of infrared radiation and visible light (“What is pyrometer,” 2020). This approach to prevention will isolate patients suspected of coronavirus from healthy patients and prevent mass contamination among clients and healthcare workers.
Personal Protective Equipment
However, this is not the only solution to this problem. In the dialysis ward, all employees and patients should wear personal protective equipment — one-time masks and gloves. If all persons involved are protected, relatively close, physical contact will be acceptable: as in the case of a nurse touching a patient while they are connected to a hemodialysis machine. When the patient comes to the registration site to sign up for a procedure or receive a referral, they must be interviewed about the health status and cases of contact with infected people. In addition, all accessible areas of the facility — the lobby, reception, toilet, and treatment room — must be equipped with antiseptic liquids. Meanwhile, according to Gharpure (2020), hand sanitizers are an effective measure to prevent infection. However, it should be remembered that excessive use of alcohol-containing antiseptics leads to the development of resistance in the virus and also has a negative effect on hand skin (Mahmood et al., 2020). At the same time, dialysis nurses should be adequately sanitized, wear protective equipment, and dispose of them in a timely and appropriate manner.
A Stock of Food Helps to Reduce Overcrowding in Supermarkets
In addition, if an outbreak of the virus is detected in an area where a dialysis patient lives, the risk of infection must be reduced first. In order to achieve this goal, it is incredibly important to reduce the number of social contacts with people and to limit visits to shops and public places. It is, therefore, extremely important that the patient has at home a stock of food and drinks that will not spoil for a long time. In the context of a pandemic, it is crucial to prepare in advance and stock up for a few weeks of healthy and suitable diets, food, clean water, and medicines. This will help reduce the risk of infection as the patient avoids overcrowded grocery stores and pharmacies. “Kidney disease” (2020) recommends that a patient with kidney or mild renal failure has the right amount of the following foods. These include low-fat fruits, vegetables, large quantities of protein that can be found in salmon, meat, beans and tofu, dairy products, grains, and unhealthy fats.
Changes in Standard Dialysis Practices
In the context of the pandemic, the limited availability of medical supplies — dialysis membranes, sterile materials, and fluids — is a significant challenge. To preserve available materials, it is possible to reduce dosages without harming the patient. For example, Burgner et al. (2020) write about the possibility of reducing dialysis treatment time to three hours twice a week, which will also significantly relieve the workload of medical staff. Further, the researchers write that even if they run out of dialysis fluid, medical workers can prepare it using known prescriptions by pharmacy materials. Certainly, a fantastic solution for achieving the conditions of social distance can be an extension tube of dialysis length. This becomes especially important if hemodialysis is necessary for a patient infected with COVID-19: a nurse connects the patient and then moves away from him at a safe distance.
Training Program for Nurses and Dialysis Patients Recommendation
A training program is not insignificant for patients who know little about the pathways and forms of the disease. It is fair to say that some citizens do not take great responsibility for their own and public health by ignoring prescribed measures or by not studying additional information which is available to all. The categories of citizens who may not be aware of the threat of COVID-19 include older persons primarily. Due to financial security, grandparents may not have a TV, computer, or access to the Internet, may not read newspapers due to vision problems, and may not communicate with friends or relatives. This creates conditions for complete information isolation, which is reflected in a lack of awareness of the pandemic in general. The other category includes migrants from low-income countries where clinical medicine is not widely available. Nearly half of registered migrants who left in search of better wages or a political climate do not know about the pandemic (Handley, 2020). In other words, there is a problem with the spread of the pandemic because of a lack of knowledge of the theoretical foundations.
A preventive measure against ignorance should be a curriculum. In fact, implementing patient education policy in a clinical organization could address two factors simultaneously: increasing the level of knowledge among health professionals and promoting more rational behavior among citizens. In particular, responsible persons conduct a training program for health care workers on the safest type of communication — through virtual communication. The healthcare provider must be able to get answers to all the questions that they have. By doing so, in the framework of the dialysis department, the medical staff should be able to tell clients about health threats, preventive measures, and the importance of social distance.
The Importance of Isolation of Infected Patients
The coronavirus pandemic shows the need to isolate COVID-19-positive patients from those who are not infected. By isolation of infectious patients, one mean an anti-epidemic medical intervention aimed at separating patients, as well as those with suspected infectious disease, from those around them in order to prevent further spread of infection. In the case of quarantine of infectious diseases, persons in contact with patients are also isolated. With this approach, health facilities deal with the transmission of the virus between dialysis patients. In particular, by means of isolation, no infectious patients or other patients will be present in the general procedure room.
The main rule to be followed by medical staff is the importance of systematic dialysis treatment. It is unacceptable that an infected patient is denied a procedure (Ikizler & Kliger, 2020). At the same time, all measures introduced must be aimed at ensuring an absolutely healthy atmosphere in the office. This means that if an infected patient requires dialysis, they must be placed either at home or in the hospital. In the case of outpatient dialysis, a protected and healthy medical officer comes to the patient to perform the procedure. More severe forms may require clinical treatment, especially if perineal dialysis is needed. In this case, the infected patient should be placed in a separate room for combined treatment.
It should be recognized that patients are isolated for the entire period of infection, and those who have communicated with them for maximum incubation duration. It is known that for coronavirus infection, such a period is up to 14 days. If a patient is isolated in an inpatient setting, the patient gains a number of significant advantages. This refers to the fact that the patient is under 24-hour supervision of medical staff, which is challenging to implement as part of outpatient treatment. Thus, if the health condition of an isolated patient starts to deteriorate, the medical staff will be able to take prompt action even in the first stages. Moreover, in hospital isolation, the patient is provided with nursing care and support, as well as free food and drinks.
However, the advantages of inpatient treatment do not detract from the advantages of outpatient treatment as well. Traditionally, outpatient treatment is a medical care system in which the patient receives almost all the necessary therapeutic measures at home or in the clinic. Outpatient treatment gives the patient more freedom of action, as they can move around in their own home and work if their health allows. In addition, the risk of infection with bacterial, viral, and fungal diseases that may have reached the hospital ward is reduced. This fact is especially important for patients with kidney failure due to the phenomenon of immunodeficiency.
Evaluation and Results
Methods of Efficiency Evaluation
Post facto evaluation plays a vital role in determining the effectiveness of proposed prevention measures. Evaluation should be based on the detection of new infections in the dialysis area. If no cases of infection have been registered within the period as the preventive policy has been introduced, it means that the measures can be conditionally considered adequate. It should be recognized that this is only a formal, simplified model of results evaluation, which is due to the complexity of the proven evaluation of results. It would be unethical to conduct a real study in which two samples of patients had dialysis practice with the difference in the application of the proposed measures. Of course, such an experiment would be incredibly valuable in the context of scientific discoveries, but totally unacceptable in modern society.
However, the effectiveness of the measures taken can also be assessed by interviewing patients and health professionals about their well-being and health. The objectives of such a survey are to obtain information about the patient’s state of health during and before dialysis, to establish a trusting relationship and cooperation between the patient and medical staff, as well as to support the patient and their family, and to increase their knowledge of health. It is worth recalling that one of the proposed measures is educational practice: therefore, if the results of social surveys of patients at the beginning and after training are compared, there is likely to be a marked difference in awareness.
The key question in the context of this section is how to conduct the surveys. The problem is that dialysis patients tend to pass through the administration desk rather quickly and go to the dialysis room in an effort to save time. Questions from the nurse during the procedures are acceptable, but as a rule, they should be limited by the desire to know the state of health right now, because blood filtration can take much effort from the patient. In order for the survey to be successful, the following factors must be observed to increase effectiveness: an accessible environment, detailed explanations, enough time to establish trusting contact, and patients’ reflections on the answers. In particular, if a medical organization’s client is a migrant from another country with a different cultural background, the organization’s staff must responsibly address the language and cultural barriers.
The most appropriate scenario is to conduct the interview before the dialysis procedure when the patient still has the capacity to answer questions. The proposed model consists of asking the patient to fill out a questionnaire with several questions and pass it to the administrator. Taking into account that the questions concern potential cases of contact with infected people, the questionnaire should not be anonymous and requires filling in a personal data field — the patient’s name and surname, as well as a telephone number for communication. Only after the patient fills in the form will they be given a referral for dialysis. Indeed, this measure may seem rather conservative and restrictive for patients – some of them may be irritated by the need to fill out the paperwork. However, in the context of a pandemic, where social contacts need to be significantly reduced and the spread of the virus prevented, completing the form is a good option.
Results Achieved in Implementation of Protocols
Reliability is of paramount importance in ensuring public health and safety for patients and medical staff in the dialysis department. A number of mild measures could undoubtedly be introduced, but they are likely to have no effect. On the contrary, a proactive official may restrict the activities of clinical organizations too much, which would be detrimental to patient health and nursing jobs. A compromise is needed in this situation — this is precisely what has been suggested as a solution.
These preventive measures have been implemented in the local clinic in order to verify its validity and to achieve safety in the ward. It is worth admitting that regular temperature screening, interviewing, and training of patients, along with wearing personal protective equipment and distancing, showed excellent results for the clinic – not a single case of infection was found on the premises of the clinic. Although it is difficult to judge mathematical correlations and statistical results, the absence of infection is quite simple to say that the proposed measures are effective.
This conclusion demonstrates the high effectiveness of the proposed measures. While this practice has shown success in one dialysis clinic, it is recommended to extend safety standards for all other health facilities at the state level. With the necessary authority, officials can provide medical organizations with the necessary materials for temperature control and respiratory protection. Looking ahead, this approach means a rapid decline in the number of diseases among both at-risk patients and health professionals. If prevention protocols are extended to the territory of the state, minimum case of infection and death rates can be achieved.
Conclusion
To sum up, the COVID-19 pandemic, caused by a previously unknown coronavirus virus, has become the most pressing problem of 2020. There is no doubt that the pandemic has caused damage to all familiar sectors of human activity, including the economic and health systems. The lack of a stock of personal protective equipment and medical consumables, reflected in high rates of infection among the population, indicates the ineffectiveness of the current public health system. Politicians should review the financing of the medical sector, encourage the development of scientific research, and provide clinics with the necessary materials to achieve positive recovery results.
The pandemic has exposed a number of significant challenges that are relevant for clinics treating non-communicable diseases, including renal diseases. First and foremost, several clinics have found a decrease in the number of cases in which health workers have sought assistance. This phenomenon can be justified either by patients’ fear of getting infected when leaving home or by financial problems caused by quarantine. One way or another, the refusal of procedures is not allowed, since the therapy is essential to be systematic and orderly. On the other hand, due to a large number of infections, many clinics have been re-qualified to care for COVID-19 patients. This led to a situation where nurses could temporarily lose their jobs. At the same time, the work showed a pattern in which employers were not interested in hiring nurses who were not competent to fight infections in crisis conditions.
Patients with non-communicable kidney diseases are among the risk groups for COVID-19 infection. It should be recalled that patients with kidney disease have immune deficiency, which is particularly essential when a timely immune response to coronavirus is required. Little research has been done to determine the relationship between kidney disease and viral infection, but there is no universal scheme. While some authors point to high exposure among patients with kidney disease, others write that COVID-19 may cause renal failure. The mechanisms of this phenomenon may be a reduced amount of elementary oxygen in the blood, direct damage to kidney tissue or autoimmune response of the body. In either case, this situation is critical, so such patients need to be treated by blood filtration.
It is known that the human urinary system does the removal of toxins and products of metabolism from the body by blood filtration. If, for some reason, the kidneys do not cope with their functions, toxins accumulating in the body, lead to intoxication, which is fraught with a lethal outcome. The procedure of kidney dialysis is a known replacement method of artificial cleaning of the body: during the procedure, the body is freed from the products of decay. In the process of hemodialysis, there is a filtration of colloidal substances, which are not dissolved but only clogged vessels and streams.
It is known that the standard practice of dialysis includes finding the patient in the medical room, together with other patients and nurses. If one of the patients has a coronavirus infection, especially in asymptomatic form, there is a risk of mass infection. A system of preventive practices and protocols should be developed to eliminate negative consequences. In this research work, it was shown that such preventive measures include regular monitoring of temperature and patients at the entrance, the mandatory wearing of personal protective equipment, disinfection of the room, and the installation of hand sanitizers. In addition, participants must maintain social distance in order to reduce the likelihood of infection. Finally, adequate education of patients about modes of transmission, personal hygiene, and preventive measures is the resultant factor in reducing the spread of the pandemic.
Evaluation of results plays an essential role in determining the impact of measures taken. However, it is worth saying that it seems challenging to conduct evaluations in the dialysis section. Ethical considerations do not allow trials to be conducted with a control group, and effectiveness can only be measured by tracking cases of infection. However, interviewing patients is a good strategy when trying to measure policy effectiveness. This paper discussed the challenges that arise when attempting to introduce survey practice. In particular, patients may not be willing to talk about their health status. However, it is important to recognize that it is possible to achieve a real reduction in epidemiological indicators through questionnaires. To avoid social contact between the administrator and the patient, it is recommended that the customer be asked to fill out a small questionnaire about well-being, general health, and awareness, and provide the name and telephone number to contact them.
The protocols mentioned above were applied in a local small clinic setting to get preliminary results. It is worth noting that the experiment was highly effective — no cases of infection were found on hospital premises. However, it must be recognized that this model requires further development and more detailed performance evaluation. It can already be stated that the systematic introduction of practices in other medical organizations and public places has a positive impact on reducing the overall infection rate.
References
Apicella, M., Campopiano, M. C., Mantuano, M., Mazoni, L., Coppelli, A., & Del Prato, S. (2020). COVID-19 in people with diabetes: Understanding the reasons for worse outcomes [PDF document]. Web.
Aye, B. (2020.) The new coronavirus: Crisis preparedness requires improved public funding of health. Web.
Braithwaite, J. (2018). Changing how we think about healthcare improvement [Podcast]. Web.
Burgner, A., Ikizler, T. A., & Dwyer, J. P. (2020). COVID-19 and the inpatient dialysis unit: Managing resources during contingency planning pre-crisis. Clinical Journal of the American Society of Nephrology, 15(5), 720-722.
Coronavirus cases. (2020). Web.
Coronavirus worldwide graphs. (2020). Web.
Cortese, M., Sherman, A. C., Rouphael, N. G., & Pulendran, B. (2020). Systems biological analysis of immune response to influenza vaccination. Cold Spring Harbor Perspectives in Medicine, 10(7), 1-10.
Gharpure, R., Hunter, C. M., Schnall, A. H., Barrett, C. E., Kirby, A. E., Kunz, J.,… & Garcia-Williams, A. G. (2020). Knowledge and practices regarding safe household cleaning and disinfection for COVID-19 prevention. Morbidity and Mortality Weekly Report, 69(23), 705-719.
Handley, E. (2020). Coronavirus has killed more than 500,000 people. But some still don’t know the pandemic exists. ABC News. Web.
Ikizler, T. A., & Kliger, A. S. (2020). Minimizing the risk of COVID-19 among patients on dialysis. Nature Reviews Nephrology, 16, 311-313.
Kidney disease & COVID-19. (2020). Web.
Mahmood, A., Eqan, M., Pervez, S., Tabinda, A. B., Yasar, A., Brindhadevi, K., & Pugazhendhi, A. (2020). COVID-19 and frequent use of hand sanitizers; human health and environmental hazards by exposure pathways. Science of The Total Environment, 742(10), 1-7.
McGill, R. L., & Weiner, D. E. (2017). Dialysate composition for hemodialysis: changes and changing risk. Seminars in Dialysis, 30(2), 112-120.
Ng, J. K. C., & Li, P. K. T. (2018). Chronic kidney disease epidemic: How do we deal with it? Nephrology, 23, 116-120.
Nussbaumer–Streit, B., Mayr, V., Dobrescu, A. I., Chapman, A., Persad, E., Klerings, I.,… & Gartlehner, G. (2020). Quarantine alone or in combination with other public health measures to control COVID‐19: A rapid review. Cochrane Database of Systematic Reviews, 4, 1-47.
Prasad, N., Agarwal, S. K., Kohli, H. S., Gopalakrishnan, N., Fernando, E., Sahay, M.,… & Lobo, V. (2020). The adverse effect of COVID pandemic on the care of patients with kidney diseases in India [PDF document]. Web.
Rappuoli, R., Black, S., & Bloom, D. E. (2019). Vaccines and global health: In search of a sustainable model for vaccine development and delivery. Science Translational Medicine, 11(497), 1-8.
Russia might register coronavirus vaccine by end of summer – expert. (2020). Tass. Web.
Smith, D. (2020). When will COVID end? The update on the race for a vaccine. CNet. Web.
Sperati, J.C. (2020). Coronavirus: Kidney damage caused by COVID-19. Web.
Stavroulopoulos, A., Stamogiannos, G., & Aresti, V. (2010). Pandemic 2009 influenza H1N1 virus vaccination: Compliance and safety in a single hemodialysis center. Renal Failure, 32(9), 1044-1048.
Symptoms of Coronavirus. (2020). Web.
Thompson, S. A. (2020). How long will a vaccine really take?The New York Times. Web.
Ungchusak, K., Sawanpanyalert, P., Hanchoworakul, W., Sawanpanyalert, N., Maloney, S. A., Brown, R. C.,… & Chusuttiwat, S. (2012). Lessons learned from influenza A (H1N1) pdm09 pandemic response in Thailand. Emerging Infectious Diseases, 18(7), 1058.
What is pyrometer: Working principle and its types. (2020). Web.
WHO. (2020). The classical definition of a pandemic is not elusive. Web.
Yong, E. (2017). Is it possible to predict the next pandemic?Web.
Zhang, J., Du, Y., Bai, L., Pu, J., Jin, C., Yang, J., & Guo, Y. (2020). An Asymptomatic patient infected with coronavirus disease 2019. American Journal of Respiratory and Critical Care Medicine, 201(11), 1428-1429.