Introduction
Offering quality services in the health care system goes a long way in improving the overall wellness of a population. The Australian healthcare system seeks to promote the delivery of high-standard services amid the presence of various challenges. The issue of hospital readmissions is one of the notable challenges that are undermining the efficiency of the Australian healthcare system (AIHW 2017b). Particularly, readmissions infer to the scenario where patients are admitted once more after being discharged from the health facility within a given time (Zhou et al. 2016). The different literature materials available identify the triggers of hospital readmissions that range from poor patient engagement to the weak communication between the outpatient and inpatient health experts (Schairer et al. 2014). This study is based on the question, “Can addressing the main causes of high readmission rates and the establishment of relevant mechanisms improve this outcome in Australia?” In this concern, this paper discusses the need for identifying the causes of hospital readmissions in Australia as a strategy towards improving the outcomes of the issue in the country’s healthcare system.
Data Acquisition
The study analyses de-identified data acquired from the Australian Institute of Health and Welfare (AIHW) since this source bears updated, credible, and reliable information concerning health in Australia. The study upholds ethical guidelines that safeguard the improper retrieval of such data by ensuring that the source is well-acknowledged, as opposed to taking materials directly from AIHW and presenting them as part of this presentation’s research. As such, permission is sought from the AIHW to have the data collected. However, the only information related to hospital readmissions, including the causes, is retrieved since it is in line with the study question and hence it will help to answer it.
The results of the data will help in understanding the hospital readmissions issue in Australia before identifying the strategies that can be adopted to improve the health outcome. Moreover, discussing the strategies for change implementation is relevant in the context of improving the prevailing health system issue experienced in Australia. For instance, ensuring that health experts observe the safety precautions to avoid the spread of hospital-acquired infections (HAIs) is one of the strategies geared towards the minimization of hospital readmissions in Australia. Besides, assessing the degree to which patients observe the required practices after getting out of the hospital facility is also necessary towards fostering an understanding of the unplanned readmission cases reported in Australia. The results are generalizable of the patient population being investigated.
Data Presentation
In Australia, ineffective surgical operations account for the leading causes of hospital readmissions. Such unexpected or unplanned readmissions offer an indication of the performance of healthcare providers in offering appropriate, high standard, and affordable hospital atmosphere, as well as hospital-related care (Wimmer et al. 2014). During the 2013-2014 period, surgical operations associated with high cases of unplanned readmissions included cataract extraction, appendectomy, hip replacement, knee replacement, prostatectomy, hysterectomy, tonsillectomy, and adenoidectomy (AIHW 2016). AIHW mainly considered unexpected readmissions to the same public hospital that occurred within one month after the discharge of the patient receiving surgical operation. Figure 1 below shows hospital readmissions within one month after a patient is released from the same health facility.
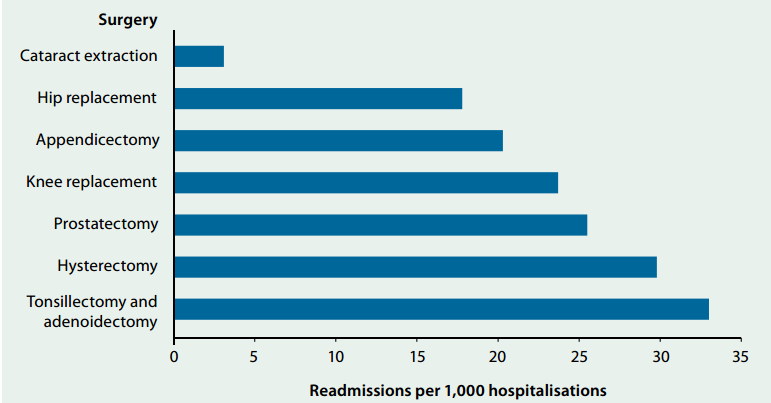
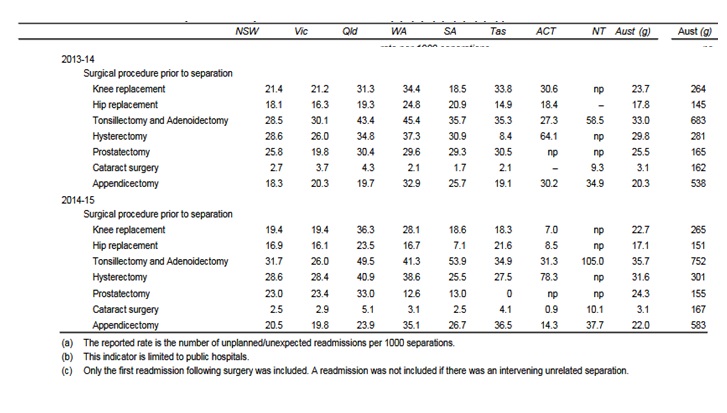
The graph above indicates the type of surgeries, which are associated with the leading causes of hospital readmissions in Australia. Notably, the top surgical operations associated with greater chances of unplanned readmissions include tonsillectomy and adenoidectomy, hysterectomy, prostatectomy, and prostatectomy recording 3.3%, 3%, and 2.6% readmissions within a month respectively. Cataract extraction procedures reported only 0.3% readmissions in the same hospital between 2013 and 2014. The period between 2014 and 2015 also witnessed considerable cases of hospital readmissions that showed small variations with the rates recorded during the 2013-2014 period. Figure 2 below shows the unplanned readmission figures for different separation procedures.
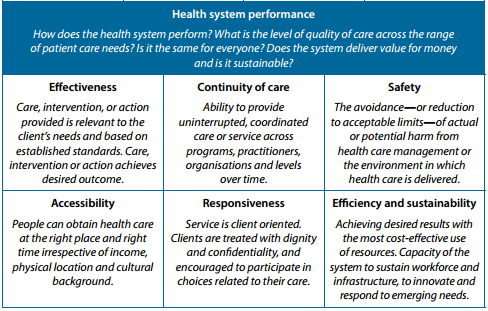
The data denotes that various inefficiencies occur in the operating room since surgeries contribute to the top health procedures reporting unplanned readmissions. Undoubtedly, it is necessary to investigate the causes of the considerable rates of unexpected readmissions in various public hospitals in Australia. In this respect, gaining an understanding of the hospital system performance indicators in Australia is crucial towards facilitating the identification of the factors contributing to unplanned hospital readmissions. Figure 3 shows the performance indicators in Australia’s health system.
The analysis of data regarding the factors associated with the delivery of quality services, including patient engagement, upholding respect, and spending adequate time with the patient, is necessary. The failure of health experts to observe the identified care delivery practices leads to poor performance as indicated by outcomes such as improved interaction between the specialist and the patient. As such, the performance indicators include the willingness of the specialist to address the patients’ needs effectively, the level of respect, and the adequacy of time spent between the patient and the client. Figure 4 below shows the data of patients’ perceptions regarding the willingness of doctors or specialists to listen carefully to the issues raised by patients regarding their health needs.
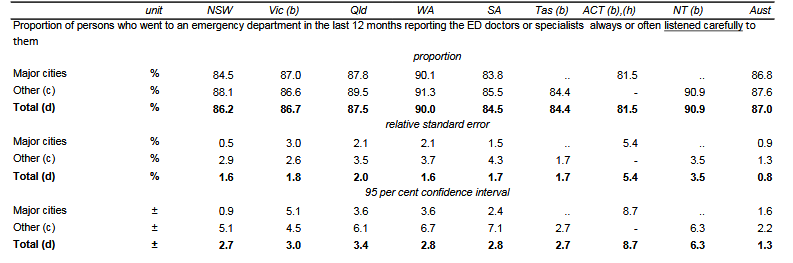
The data shows that 87% of patients re-admitted in different public hospitals within Australia interacted with health professionals who listened carefully to their health concerns. On the other hand, 13% of the patients reported dissatisfaction with the communication approach of the health expert. Therefore, the lack of effective communication between the health expert and the patient is a considerable factor that causes hospital readmissions in the different states within Australia.
Besides, engaging in effective communication, spending enough time with the patient is crucial towards fostering the physician’s understanding of the patient’s health needs. This observation is founded on the awareness that therapeutic relationships can have a significant influence on not only communication but also trust and respect between the patient and health professional. On the other hand, a bad relationship can influence the subjective data provided by patients. The data presented in Figure 5 below reveals the perceptions of patients regarding the adequacy of the time they spend with the health professional.
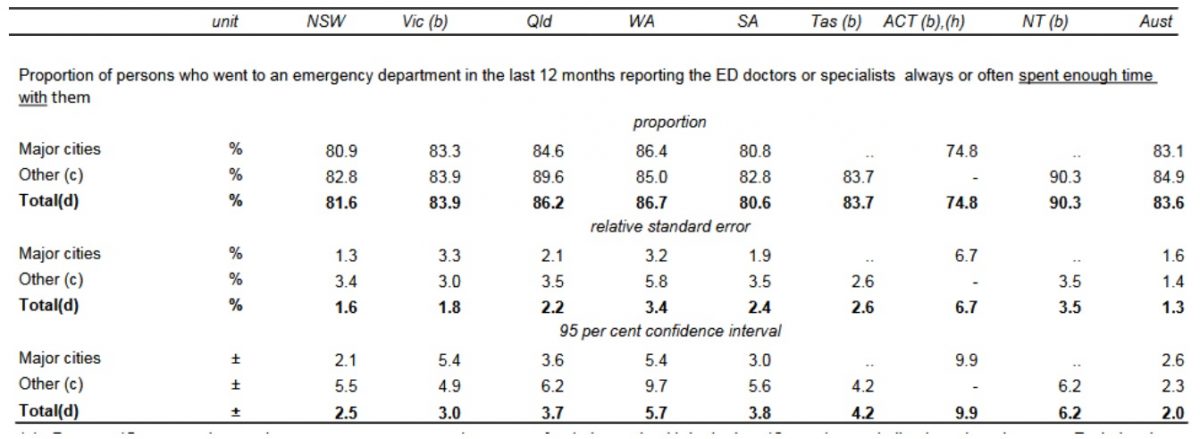
Surprisingly, a considerable 16.4% of health professionals do not uphold the essence of spending enough time with patients in different care delivery processes. The limited-time spent between the patient and the health expert shows some lack of interest in improving their wellbeing. For this reason, more patients continue undergoing hospital readmissions as an adverse outcome of healthcare delivery in Australia.
Showing the client respect is also part of the process of improving their health position. Nonetheless, some health experts overlook the relevance of respect in the course of offering healthcare services in a way that undermines the efficiency of the entire healthcare system. The data in Figure 6 below uncovers the figures relating to the level of respect showed by health professionals as they attend to admitted and re-admitted patients in the various public hospitals in Australia.
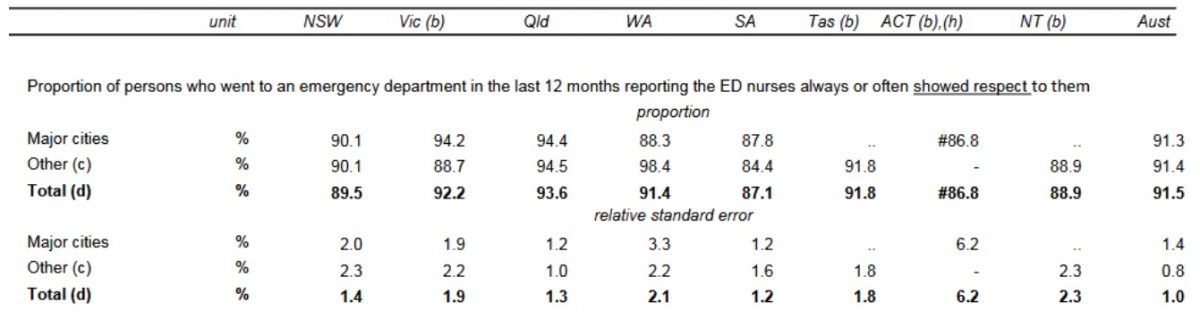
The data reveals that 91.5% of the persons seeking healthcare services in the Australian public hospitals interacted with specialists and doctors who showed desirable extents of respect. In this light, the data shows that Australian health professionals, especially nurses handling ED admissions still treat customers with some lack of respect. The issue can be one of the considerable factors that lead to medical errors that undermine the safety of patients. Besides, other non-medical errors may arise from the failure to observe the recommended safety procedures at home, for instance, establishing the necessary precautions to avoid falls. Such precautions may include the elimination of clutter and ensuring that all walking areas in and outside the house are perfectly illuminated, the use of well-serviced beds and seats, removing any slippery substances in the house, and the availability of grab rails.
Meaning of the Data
The data collected is in line with the research question since it captures issues concerning readmission cases in Australia, including the underlying causes, which will help answer the question. Particular health conditions expose people to higher chances of unplanned hospital readmissions compared to other health issues. In the Australian context, patients who undergo separation procedures, including cataract extraction, appendectomy, hip replacement, knee replacement, prostatectomy, hysterectomy, and tonsillectomy and adenoidectomy, have a high probability of readmission (AIHW 2016). In this regard, people in the Australian population who experience problems with their tonsils and adenoids should expect to have a 3.3% risk of going through hospital readmission after going through a tonsillectomy. However, this change is triggered by an array of factors related to the treatment process, as well as the patient’s recovery process after discharge. The same trends apply to other conditions, including cataract, appendicitis, and prostate cancer, among other conditions (AIHW 2016).
Congestive heart failure is one of the leading health conditions associated with unplanned hospital readmissions among patients under the Medicare health program. The other health issues related to high instances of readmissions include cardiac dysrhythmias, septicemia, pneumonia, and chronic obstructive pulmonary disease (COPD) (van Walraven, Jennings & Forster 2012). Since some health conditions have a higher probability of prompting the patient to be readmitted to the same hospital within one month after discharge, health providers must observe measures that improve the standard of services. Some of the measures include observing the required safety precautions and educating the patient about the importance of leading a healthy lifestyle.
Undoubtedly, aspects of safety and quality in the area of healthcare attract scrutiny from different parties. Safety here refers to the alleviation and reduction of considerable limits of potential or actual harm emanating from healthcare management or the setting in which health care is offered. On the other hand, the aspect of quality in health care infers to a wide concept concerning whether the delivery of services realizes the intended outcomes for the patient and/or whether the offering coincides with the set standards and procedures (AIHW2017a). For this reason, the National Health Performance Framework (NHPF) underlines the significance of engaging in professional practices that bolster the provision of safe and quality healthcare interventions (Braet, Weltens & Sermeus 2016). Nonetheless, the rate of hospital readmissions associated with individuals who underwent a surgical operation in the last one month in the same public hospital refers to the failure of health experts to observe measures that promote safety and quality (Braet, Weltens & Sermeus 2016).
The failure to observe safety measures in health care provision exposes patients to the risk of developing complications. In most readmissions after surgeries that involve the extraction of cataract, patients portray symptoms of infection, thereby raising questions regarding the observance of safety standards when performing such procedures (AIHW 2017a). For instance, health professionals involved in surgical processes can observe safety measures such as the disinfection of surfaces to curb the emergence of HAIs. Nonetheless, patients can also play their role in upholding safety measures after being discharged from the hospital.
The data obtained from AIHW (2016) reveals that, on average, 10% of the identified staff members attending to patients are less engaging. Offering patient-centered services goes a long way in fostering the quality of health care (AIHW 2016). Notably, the data indicates that some doctors show little respect to patients besides not listening to their opinions, which can improve the quality of the medical intervention. In other cases, healthcare providers overlook the importance of spending enough time with patients as a way of collaboratively working together in facilitating the improvement of their (patients) wellness. Therefore, the absence of patient engagement is a factor that may be associated with instances of hospital readmissions in different Australian hospitals. For instance, failing to listen to patient care can make the health professional miss important information about the uniqueness of the patient’s condition, thus leading to the administration of ineffective treatment.
The data acquired unearths the inadequacy of time spent between the patient and the caregiver. Medical professionals should invest adequate time with the patient to foster communication about important details of the health improvement process (van Walraven, Jennings & Forster 2012). The scenarios of specialists failing to allocate time to listen to patients, as well as engaging them in making decisions that promote the desired health outcomes, is a likely trigger of hospital readmissions reported in Australian hospitals. This situation may arise following the failure of health officers to listen to patients, including the subjective data they offer. Important to note, poor communication with the patient undermines the establishment of a suitable transition care intervention after discharge (Feltner et al. 2014). The need for streamlining the communication between the inpatient and outpatient healthcare providers is important towards fostering the effectiveness of the transition care offered to the patient after discharge. Poor transition care intervention has the potential of weakening the quality of care provision, thus resulting in cases of hospital readmissions.
Healthcare Improvement
The Identification of High-Risk Patients
The integration of necessary measures that address the causes of high readmission rates is crucial in facilitating the reduction of the situation experienced in the Australian health system. The identification of high-risk patients is one such measure. Predicting patients who have greater risks of hospital readmission is one of the crucial steps for managing the health outcome in Australia. Notably, some health conditions, including prostate cancer, expose the patient to increased chances of rehospitalization. In this respect, the incorporation of transitional interventions for high-risk patients is necessary for improving the health outcome in Australian public hospitals. Studies reveal that transition care intervention reduces the risk of readmission by a considerable 20% within 30 days after discharge (Feltner et al. 2014). Therefore, Australian health care professionals need to consider different high-risk conditions that require transitional care intervention to cut the risk of readmissions. Particularly, the Australian hospitals can improve transitional care intervention by ensuring that professionals acquire and review patients’ discharge information, review the essence of follow-up, and offer education to the patient and/or caregiver.
Besides the application of effective transition care interventions, health care experts may also use readmission risk prediction models to single out high-risk patients. The risk that prediction models have is their capability of stratifying high-risk and low-risk patients, thus influencing the approaches embraced by the caregiver. However, health professionals need to take into consideration various aspects of such models, including their availability, complexity, and performance. Therefore, the concerned parties seeking to improve the readmission issue in various hospitals in Australia may incorporate a compatible readmission risk prediction model to improve the health outcome (Kelly et al. 2012). One of the considerable risk prediction models for hospital readmissions is the LACE model. The model focuses on the length of stay, acuity of the admission, comorbidity of the patient, and emergency department used in the last 6 months.
Upholding Patient Safety
Patient safety is a significant factor in the delivery of healthcare. Medication errors expose the health of patients to risks that can trigger adverse outcomes. In most instances, medication errors take place at the transition points. In this concern, the hospital can apply systems such as the Computerised Physician Order Entry (CPOE) to facilitate the reduction of medication errors as the patient undergoes a transition from inpatient to outpatient services (Donzé et al. 2013).
The need to communicate with the discharged person about the safety measures they need to observe is also important. Importantly, hospitals in Australia can implement multimodal and comprehensive interventions that promote the safety of the patient even after leaving the hospital environment. Health experts can also give instructions to patients, as well as their families, on the necessary self-care methods (Braet, Weltens & Sermeus 2016). Additionally, fostering communication with outpatient physicians reduces the development of safety risks after the discharge of a patient. The hospital can arrange with the outpatient health expert to share a copy of the patient’s file ethically to streamline the medical processes from the inpatient and outpatient settings. This strategy ensures that the outpatient professional gains an understanding of patients’ history regarding their health.
Fostering Patient Engagement
The engagement of patients in the process of providing health care goes a long way in influencing their readmission levels. Importantly, engaging the patient ensures that they take part in the decision-making process to facilitate the improvement of their health status. In this light, engaging patients facilitates the creation of a better understanding of their health needs. Notably, the study reveals that some doctors and specialists spend a limited time with patients, thus engaging them inadequately. The situation undermines the efficiency of the clinical interventions while at the hospital during the recovery phase after discharge. Patient engagement is integral in streamlining communication regarding the discharge instructions. Following discharge instructions reduces the chances of complications that arise from poor dosage or the lack of adherence to safety precautions (Kilkenny et al. 2013).Additionally, communicating about the possible side effects of a medical procedure raises patients’ awareness of the expected experiences. Effective communication is also significant for scheduling a follow-up appointment that seeks to improve the recovery process. Additionally, active communication among the patients, caregivers, and families is also necessary towards improving the healthcare outcomes (Leppin et al. 2014).
Streamlining the Follow-up Process after Discharge
Importantly, healthcare staff members need to demonstrate awareness regarding the discharge of different patients. After identifying the discharged patients, the hospital needs to establish structures that facilitate a streamlined follow-up system. In this view, Australian hospitals need to underscore the essence of early follow-ups to manage the prevailing health outcome. Important to note, early follow-up reduces the rate of readmissions among high-risk patients by 19.1% (Kilkenny et al. 2013). Such follow-up should commence 14 days after discharge to attain the desired results. The hospitals can implement the follow-up strategy by ensuring that patients are contacted 14 days after discharge to gain information about their progress. Therefore, outpatient health specialists in the Australian health system need to spend enough time with the discharged patients to monitor their recovery process keenly.
Change Management
The Establishment of the Change Implementation Team
Identifying the membership for the change team is important. The key team members facilitate the change process to attain the sought-after outcomes (Kash et al. 2014). In the context of the prevailing Australian health issue of high readmission levels, the change team should include the medical and non-medical staff officials who need to ensure the delivery of quality and safe services to patients. Importantly, leaders of the change team should include specialists and doctors, as well as nurses, especially those working in the area of surgical operations.
The membership of the change team should be comprised of clinical leadership responsible for testing and implementing the change besides solving problems that may arise in the process. Additionally, the implementation team should consist of experts who know the dynamics of the health outcome that requires improvement (Curran et al. 2012). The presence of day-to-day leadership is also crucial in ensuring the completion of the teams’ tasks.
The Establishment of a Quality Improvement Plan
The quality improvement team needs to identify goals that the improvement process should attain. The naming of performance metrics is also crucial for monitoring and assessing the extent to which the change process facilitates the attainment of desired outcomes (Feltneret al. 2014). In this view, the implementation team needs to establish the standards of practice that would facilitate the attainment of improved outcomes. The quality improvement plan facilitates the development of the vision for change in a particular system. By so doing, members who are associated with the change process may establish the values and practices that drive positive change in the organization (Morello et al. 2013). Therefore, the improvement plan incorporates the strategy for realizing the vision of the change initiative. Although no template is currently available, the plan may include the ways of fostering the interaction between the specialist and the patient to create a collaborative approach towards the delivery of quality care, thus minimizing readmissions. Members of the team may include physicians and nurses affiliated to the departments reporting the considerable cases of hospital readmissions. In this respect, senior physicians, as well as surgeons, can play the lead roles in the team by communicating the vision, encouraging nurses to uphold safety, and offering creative ways of handling issues in the hospital setting. Nurses can also play the role of enhancing the awareness of patients on the importance of continuing with the recommended medication even after discharge.
Communicating the Vision
The stakeholders need to understand the vision that represents a positive change in an organization. Since the change message competes with other day-to-day messages in the institution, it needs to be clear and concise to be embraced by the entire members of the institution (Kash et al. 2014). The communication aspect is crucial for addressing the concerns of the shareholders. As such, the change team may direct all energies to the change process collectively.
The Removal of Obstacles
The existence of obstacles in a change process is inevitable in most cases. In this concern, the change team needs to incorporate measures that remove the obstacles, which undermine the realization of a positive change. Resistance to change is one of the factors that require keen consideration by the change team (Curran et al. 2012).In the context of readmission cases in Australian hospitals, doctors, specialists, and nurses’ willingness to embrace positive change is important for fostering the success of the change process.
Additionally, the change process needs to take note of the processes that interfere with the successfully implemented change. In this light, there is a need to implement a change system that is compatible with the structures and processes of the organization (Kash et al. 2014). Therefore, the change team needs to take note of the change barriers and remove them to achieve the desired vision. Furthermore, the removal of obstacles facilitates the empowerment of the team to execute the mission.
Building on the Change
The need to attain long-term transformation necessitates the team to build on the change. Thus, the change process should not only celebrate small wins but also incorporate practices that foster the attainment of a positive change in the organization (Curran et al. 2012). Positive change is important since it leaves all parties motivated and willing to work extra hard in their respective lines of operations to their benefit and that of the organization. In this regard, there is a need for the integration of mechanisms that promote continuous change in the organization. The change strategy should also concentrate on undertaking contentious monitoring and evaluation. The approach facilitates the identification of the strengths and weaknesses associated with the change process.
Conclusion
The issue of hospital readmissions reveals the level of inefficiency in the Australian health system. The leading medical procedures associated with hospital readmissions include cataract extraction, appendectomy, hip replacement, knee replacement, prostatectomy, hysterectomy, and tonsillectomy and adenoidectomy. The triggers of the healthcare outcome include risks associated with the health condition, poor patient engagement, ineffective transition care intervention processes, and poor communication between the inpatient and outpatient health professionals. Therefore, there is a need for the Australian health system to integrate strategies such as the identification of high-risk patients, upholding patient safety, fostering patient engagement, and streamlining the follow-up process after discharge. The effectiveness of the process of change should observe key strategies, including the establishment of a competitive change team, the creation of a comprehensive implementation plan, communicating the vision, removing any obstacles, and building on the change.
Reference List
AIHW 2017a, Admitted patient care 2015-2016. Web.
AIHW 2017b, National healthcare agreement: PI 23-unplanned hospital readmission rates. Web.
AIHW 2016, Australia’s health 2016. Web.
Braet, A, Weltens, C & Sermeus, W 2016, ‘Effectiveness of discharge interventions from hospital to home on hospital readmissions: a systematic review’, JBI Database of Systematic Reviews and Implementation Reports, vol. 14, no. 2, pp.106-173.
Curran, G, Bauer, M, Mittman, B, Pyne, J & Stetler, C 2012, ‘Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact’, Medical Care, vol. 50, no. 3, pp. 217-217.
Donzé, J, Aujesky, D, Williams, D & Schnipper, J 2013, ‘Potentially avoidable 30-day hospital readmissions in medical patients: derivation and validation of a prediction model’, JAMA Internal Medicine, vol. 173, no. 8, pp. 632-638.
Feltner, C, Jones, C, Cené, C, Zheng, Z, Sueta, C, Coker-Schwimmer, E, Arvanitis, M, Lohr, K, Middleton, J & Jonas, D 2014, ‘Transitional care interventions to prevent readmissions for persons with heart failure: a systematic review and meta-analysis of transitional care for persons with heart failure’, Annals of Internal Medicine, vol. 160, no. 11, pp. 774-784.
Kash, B, Spaulding, A, Johnson, C & Gamm, L 2014, ‘Success factors for strategic change initiatives: a qualitative study of healthcare administrators’ perspectives’, Journal of Healthcare Management, vol. 59, no. 1, pp. 65-82.
Kelly, M, Sharp, L, Dwane, F, Kelleher, T & Comber, H 2012, ‘Factors predicting hospital length-of-stay and readmission after colorectal resection: a population-based study of elective and emergency admissions’, BMC Health Services Research, vol. 12, no. 1, pp. 77-77.
Kilkenny, M, Longworth, M, Pollack, M, Levi, C & Cadilhac, D 2013, ‘Factors associated with 28-day hospital readmission after stroke in Australia’, Stroke, vol. 44, no. 8, pp. 2260-2268.
Leppin, A, Gionfriddo, M, Kessler, M, Brito, J, Mair, F, Gallacher, K, Wang, Z, Erwin, P, Sylvester, T, Boehmer, K & Ting, H 2014, ‘Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials’, JAMA Internal Medicine, vol. 174, no. 7, pp. 1095-1107.
Morello, R, Lowthian, J, Barker, A, McGinnes, R, Dunt, D & Brand, C 2013, ‘Strategies for improving patient safety culture in hospitals: a systematic review’, BMJ, vol. 22, no. 1, pp. 11-18.
Schairer, W, Sing, D, Vail, T & Bozic, K 2014, ‘Causes and frequency of unplanned hospital readmission after total hip arthroplasty’, Clinical Orthopaedics and Related Research, vol. 472, no. 2, pp. 464-470.
van Walraven, C, Jennings, A & Forster, A 2012, ‘A meta‐analysis of hospital 30‐day avoidable readmission rates’, Journal of Evaluation in Clinical Practice, vol. 18, no. 6, pp. 1211-1218.
Wimmer, B, Dent, E, Bell, J, Wiese, M, Chapman, I, Johnell, K & Visvanathan, R 2014, ‘Medication regimen complexity and unplanned hospital readmissions in older people’, Annals of Pharmacotherapy, vol. 48, no. 9, pp. 1120-1128.
Zhou, H, Della, P, Roberts, P, Goh, L & Dhaliwal, S 2016, ‘Utility of models to predict 28-day or 30-day unplanned hospital readmissions: an updated systematic review’, BMJ, vol. 6, no. 6, pp. 11060-11060.