Abstract
The number of overweight people across the world has been a growing for the last three decades. This paper will examine the factors that contribute to high obesity rate among people who are 20 years and above in the United States. The trend is attributed to among other things: sedentary living, poverty, age, and the increase in consumption of unhealthy diets. In addition, in the US and Canada, food deserts are many, particularly in poor neighborhoods. Additionally, the paper will examine potential outcomes and implications before proposing potential solutions to the challenge of obesity to the above-20 population.
From the findings, it emerges that a strong relationship exists between the efficiency of healthcare systems and the health status of the public. Therefore, inefficiency in the healthcare system of a country facilitates the increase in obesity rates. This finding explains why a large number of the uninsured US 20-and-above population is obese today when compared to the people with similar income status and age in Canada. Canadians, whether poor or rich, can access the advice of a doctor on how to deal with their obesity.
The paper also finds a negative connection between earnings and obesity among females within this age bracket while the link is ambiguous in males. As a result, the study concludes that higher-income females have a minimal threat of becoming obese relative to their higher income male colleagues. Based on the effects that obesity has on the individuals and governments, the paper reveals that the solution to the menace of obesity lies in making certain adjustments both at the personal and national level, for instance, ensuring healthy eating and offering equitable access to health care for all citizens.
Introduction
The rising incidence of obesity among people of different ages and socio-economic status (SES) has become a major health concern world over. This lifestyle condition is attributed to various causes, including poor diet, sedentary living, poverty, and genetics. Generally, obesity refers to the state of a person being overweight to the extent that his or her health is impaired. Determining obesity requires a comparison of an individual’s weight versus height.
The main reason for a growing interest in obesity in the healthcare world is that it is a predisposing condition for other diseases such as diabetes, heart attack, and joint pains. This paper seeks to examine and hence determine the causes of obesity in the 20-years-and-above population in the United States. Unlike underage people, individuals in the above population are in control of their health status, both economically and physically. This study will rely on the Grossman model, which posits that individuals determine their level of health based on the investments (financial, diet, and exercise) they make.
Literature Review
Despite a remarkable decrease in obesity rates in the United States, the general trend has been a sharp increase over the last three decades across the world. Overall, obesity rates more than doubled in the three decades between 1980 and 2014 (Ogden, Carroll, Kit, & Flegal, 2014). In 2014 alone, about 1.9 billion adults aged 20 years and above were overweight. This figure translates to 13 percent of the world’s adult population.
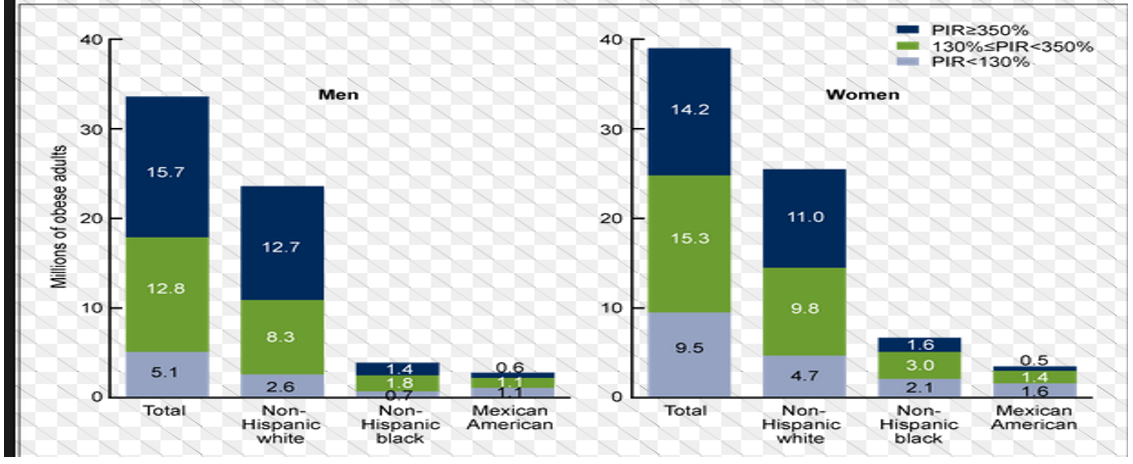
Of this population, men constituted 11% while 15% represented women, an indication that the condition is more prevalent in women relative to men. Poor and developing nations post the highest rates of obesity in the world. In developed nations, obesity is highest in the poorer populations such as those living in the inner cities (Stevens et al., 2012). In the United States, 1 in every 3 adults is considered overweight while 1 in every 20 adults has extreme obesity (Ogden et al., 2014).
According to Stevens et al. (2012), the percentage of the US population (20 years and above) with obesity is about 37.9 in at least four states. The proportion of Americans with obesity continues to increase in some states (Kentucky and Kansas) while others have posted a decline on the same, for instance, Minnesota, New York, Montana, and Ohio. In 2016, Louisiana had the highest rate of obesity by adults at 36.2 percent while Colorado indicated the lowest rate for the same population at 20.2 percent (Flegal, Kruszon-Moran, Carroll, Fryar, & Ogden, 2016). Interestingly, the states with the highest incidence of obesity (most of them are in the south) also rank highest regarding the rates of diabetes. They include Mississippi, West Virginia, Kentucky, and Louisiana. Similarly, Colorado, with the lowest obesity rates, also has the lowest diabetes rates.
According to Sturm and Hattori (2013), the highest incidences of obesity are recorded among the poor populations. Here, healthy food is difficult to obtain, a situation that causes people to depend on ‘junk’ diet. Stevens et al. (2012) explain that obesity occurs when a person consumes more calories than are needed by the body, resulting in energy imbalance. Highly refined (junk) foods are known to be energy dense, meaning that people who consume them take in more calories than their body needs. Incidentally, energy-dense foods also contain high levels of fats, which are not needed by the body (Cole & Lobstein, 2012). The increase in the intake of refined foods across the world relative to healthy natural foods means that obesity may continue to increase in the future. Further, an increase in refined food options implies that they (processed foods) become cheaper while natural ones become more expensive. As a result, people of low SES who cannot eat healthily have to depend on refined foods.
In North America, the term “food desert” has been coined to describe locations where there is no immediate access to healthy food stores. Most of these areas are found in the inner cities where the poorer populations live. According to Cole and Lobstein (2012), food deserts are the leading causes of obesity in low-income communities in the United States. All urban food deserts have similar characteristics: fast-food restaurants and convenience shops that stock only unhealthy processed foods.
While fast food would do no harm if consumed only occasionally, it becomes the daily diet for people in the food deserts because they cannot access healthy food grocery stores, which are often located miles away in the suburbs or downtown areas (Cummins, 2014). The US Department of Agriculture (USDA) classifies food deserts as poor neighborhoods that do not have grocery stores and supermarkets within a radius of at least one-mile (Cummins, 2014). Incidentally, poverty means that people in the inner cities do not own cars, which would otherwise allow them to drive up to the healthy food stores.
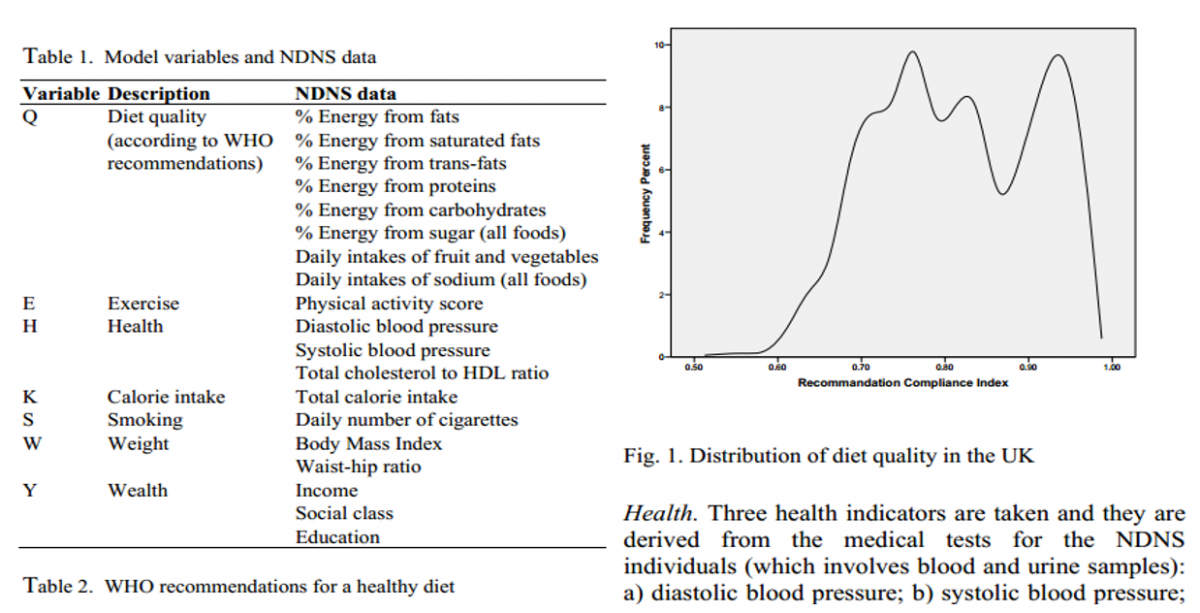
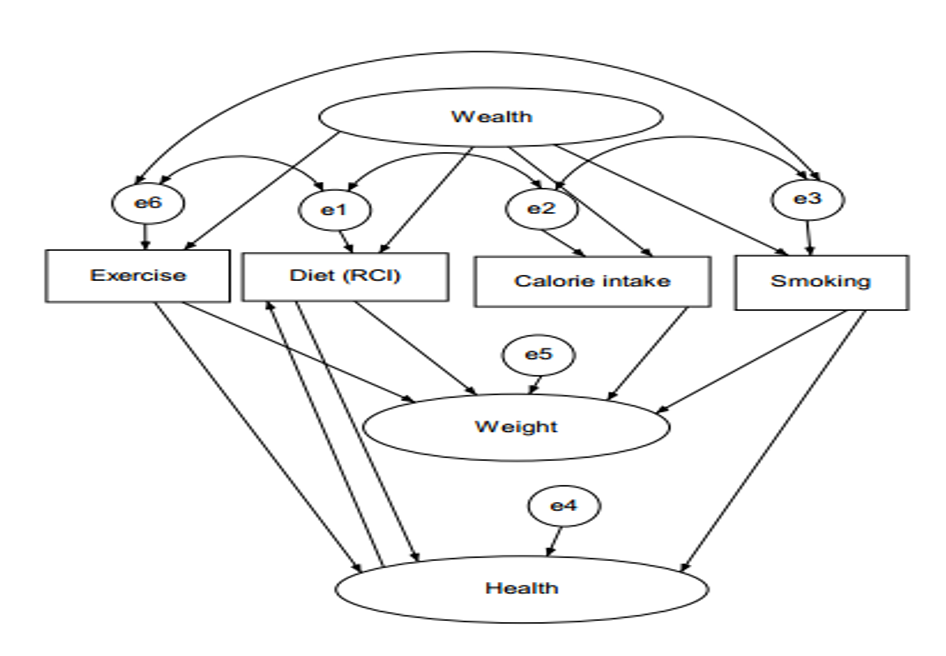
The Grossman model, developed by Michael Grossman has been used to relate certain variables with obesity (Daouli, Davillas, Demoussis, & Giannakopoulos, 2014). These variables/health inputs include health care, diet, exercise, income, environment, and time. Grossman argued that health care is not simply bought at the market, but instead depends on a combination of time and resources. Further, according to Grossman, healthcare should be approached as both a consumption product and an investment good.
Health is a consumption item in the sense that excellent health makes the owner feel good about him or herself. At the same time, health is an investment since a vigorous person remains productive at work, hence earning a reasonable income (Daouli et al., 2014). Grossman model has been employed in an attempt to explain obesity in adults, who unlike children, are people in control of their financial and life choices.
The Grossman model of healthcare links the amount that people invest in healthcare to their level of health. In other words, a person who invests enough in Medicare will generally be healthy (Grossman, Tekin, & Wada, 2014). Hence, SES plays a great role in influencing obesity among individuals. As Daouli et al. (2014) point out, without an adequate income, individuals cannot afford to buy good food, enlist at a gym, or live in safe areas. As the amount of income increases, the health status of the respective person also continues to improve. Another aspect of the Grossman model relates education and health status. As individuals acquire better education, they tend to understand obesity and hence attempt to avoid it (Stevens et al., 2012).
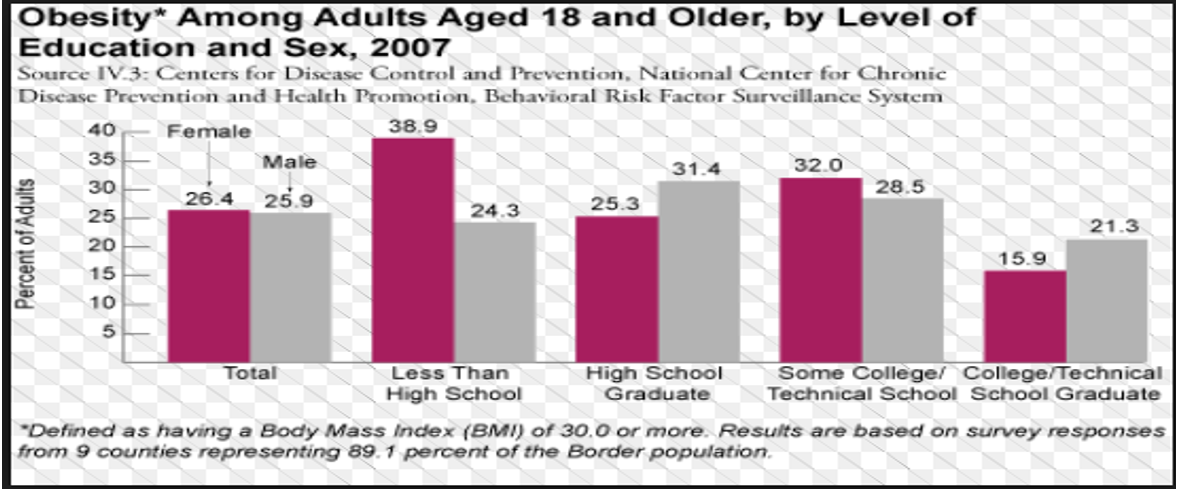
This view is backed by statistics, which show that people with college and university education register lower rates of obesity relative to those who have only attained high school education (Daouli et al., 2014). Education enlightens people on healthy life choices, which can then cause then to eat right and work out. Incidentally, in the US, college and university education is often available to people who come from middle and upper classes (Sturm & Hattori, 2013). Subsequently, these people also move on to make better health choices later in life, thus guaranteeing their continued enjoyment of good health. However, according to Sturm and Hattori (2013), some studies have failed to establish a relationship between education and obesity or have indicated “mixed results.”
The American Diabetes Association (2014) uses the Grossman model to relate socio-economic status and healthcare infrastructure. According to Saffer, Dave, Grossman, and Leung (2013), inner cities and rural areas have poor healthcare infrastructure. As such, people with low SES have limited access to healthcare facilities such as hospitals. Hence, they cannot receive useful information on aspects, including healthy eating and diet. In contrast, people in suburbs and rich neighborhoods have ready access to healthcare facilities within their residence (Sturm & Hattori, 2013). In some cases, rich families have family doctors who offer them useful information about ways of avoiding obesity.
The American Diabetes Association (2014) agrees with the view that healthy lifestyle investments will result in a low incidence of obesity. There is a negative relationship between access to quality healthcare and obesity (Saffer et al., 2014). Notwithstanding, some researchers failed to observe any causal relationship between access to quality care and obesity.
The healthcare system of a nation has a profound impact on the level of health of the people. Access to care varies widely from country to country in terms of efficiency. As such, the cost of accessing quality care seems to have a direct impact on obesity levels (Cole & Lobstein, 2012). Grossman et al. (2014) reveal that the annual medical expenditures for treating obesity-related complications have gone up in the recent times. Further, Stevens et al. (2012) attribute the annual increase in the cost of healthcare, partly to the rising incidence of obesity. These costs include both the government spending in trying to curb the trend and individual expenditures in obtaining treatment for obesity and its opportunistic diseases.
The Grossman model has also been used in an attempt to explain why the incidence of obesity is higher in women relative to men. The society endows men with more income than women, hence allowing them (men) access to better health care. Additionally, obese women are more likely to be discriminated in the job market. In contrast, Goldstone (2015) found a negative correlation between income and obesity among women while the relationship is unclear in men. In other words, higher-income women were at a lower risk of becoming obese relative to their higher income male counterparts. For men, increased income did not necessarily lead to a reduction in obesity rates.
Data Analysis
The Grossman model suggests the following variables as key in determining the health of an individual: healthcare, diet, exercise, income, environment, and time. This part will analyze data obtained from the literature review above based on these variables. The aim is to establish the reasons why there is a high incidence of obesity (35%) among the US adult population (20 years and above) by answering all or some of the following research questions:
- Is there a relationship between the SES of an individual and the likelihood of being obese?
- Does diet or exercise have a relationship with obesity?
- Does the environment/access to healthcare have a relationship with obesity?
- Does the level of education have a direct relationship with obesity?
Obesity and SES/Access to Healthcare
Obesity and Level of Education
Diet and/or Exercise
To determine whether a relationship exists between the SES of an individual and obesity, it is crucial to appreciate the numerous factors that determine an individual’s ability to access quality care. In the United States, patients usually have to pay some amount to obtain consultation or treatment from healthcare facilities. Additionally, premium care, which is mainly offered by private hospitals, is usually unaffordable for low SES individuals.
As such, there seems to be a direct relationship between people’s income and the quality of care available to them. Low SES individuals would not receive adequate information or treatment in ordinary circumstances regarding their risk of becoming obese. Thus, without this medical assistance, such individuals become overweight without realizing the full danger that they are exposed to by the condition. The Grossman model suggests that while healthcare is a resource that is subject to depletion over time, it can be replenished through obtaining the appropriate Medicare. Unfortunately, this option does not seem available to low SES individuals.
Among the US states that post the highest rates of obesity, 12 of them are in the southern region. Interestingly, the southern states are poorer relative to their northern counterparts. For instance, Mississippi that has the second highest incidence of obesity, is the leading state regarding poverty rates, at 22.6 percent (Sturm & Harroti, 2013). Of this percentage, the majority are individuals of the African-American and Latino origins.
Such people also happen to constitute the poorest population in the state. The same trend is repeated across the country even in the northern states. For instance, in New York, African-Americans lead in obesity rates, with the majority of them living in the housing projects.
Poor transport infrastructures, as well as the lack of transport means, facilitate the emergence of food deserts in central cities. According to Yoon (2012), families that do not own cars have limited access to grocery stores, most of which are located several miles from the residence. Additionally, infrastructures such as roads that connect these projects to the supermarkets are often in poor condition, thus limiting access.
As a result, housing project dwellers have to obtain (fast) food from the nearby convenience shops that do not require them to drive far from their homes. Conversely, the infrastructure in suburban areas is usually in good condition, meaning that people who live there can access grocery stores with ease. The stark difference between infrastructure in the central cities and the suburbs indicates clearly that the existence of food deserts within the minority establishments has been occasioned by poverty. It follows that poor eating habits in these housing projects culminate in high obesity rates for the dwellers of the inner cities.
Most of the housing projects are located in food deserts. Despite efforts to avail food in these food deserts, it is expensive to procure healthy diet using public funds, which are limited in nature. Thus, people here end up consuming fast foods, which are not only cheaper but also readily available. The price of refined foods continues to drop while at the same time healthy natural diet becomes costly to maintain.
For instance, a bottle of clean drinking water often costs more than a similar amount of cola soda. Consequently, those who cannot afford the healthy diet are left with no choice but to survive on fast foods, which predisposes them to abnormal weight gain. Conversely, people whose incomes allow them discretion to purchase healthy foods can escape obesity altogether. It is for this reason that people with high income are less obese because they eat right. It would seem that diet is a stronger determining factor for obesity than the other variables, perhaps with the exception of exercise.
To determine whether diet and/or exercise have a relationship with obesity, it is important to point out that exercise refers to the state of being active such as engaging in sports or going to the gym. Interestingly, people with low income engage less in physical activities relative to their richer counterparts. This observation could be caused by several factors. First, low SES individuals do not have the money to pay for the membership of a gym or to hire a personal trainer. In addition, low-income individuals are likely to work in more than one job, a situation that leaves them with little time for physical training. Lack of physical exercise causes energy imbalance, particularly where a person consumes more food than the body requires. The excess food is stored in the body as fat, leading to obesity. Specifically, energy dense foods release a large amount of “empty calories”, which are then immediately converted to fat for storage (Saffer et al., 2013).
Physical exercise may help to reduce this fat, which slows down the process of becoming obese. People who are 20 years or older may be burning fewer calories compared to their younger counterparts. This finding may partly be the reason for gaining weight, as one grows older, because as people continue to age, their body metabolism tends to slow, causing the number of calories being turned into energy to reduce. The difference then accumulates around the body, especially around the abdomen area. Statistical figures indicate that physical activity is declining across the world, including in the US (Saffer et al., 2013).
This case may be attributed to in-door jobs that do not require people to step out of their houses or offices frequently. As a result, sedentary living has become the norm, yet people continue to consume copious amounts of food. Besides, activities such as watching television and playing video games may cause people to consume large amounts of food. At the same time, such people do not move around to burn the excess calories. Incidentally, watching television and playing video games become the main preoccupation of young people in their early 20s, especially those who are yet to secure a job (Saffer et al., 2013).
The environment or access to healthcare has a bearing when it comes to determining the SES of an individual. The latter determines where people lives or the quality of care they can access. Governments strive to facilitate affordable healthcare to their citizens. The facilitation is done through healthcare insurance to enable greater access to treatment. However, availing healthcare insurance does not always imply that healthcare is accessible to all citizens because efficiency (i.e. the cost) also determines whether healthcare is available to all people, or is limited to only a few who can afford it. Take the example of two nations that provide universal health coverage for their citizens. However, in the first country, the population will need to purchase additional private insurance to attain the same level of access to healthcare, as the population of the second nation. In this case, the second nation has a more efficient healthcare system because its citizens incur fewer costs to get healthcare.
Limited studies have explored the relationship between access to health care and obesity. As seen previously, most studies focus on other socio-economic variables and their relationship with the health outcomes of individuals. The available studies point to the existence of a negative relationship between obesity and the access to healthcare. In other words, the more income an individual possesses, the less likely he or she is to become obese.
To this end, Ogden et al. (2014) have found that in healthcare systems that lack universal coverage, citizens are at a high likelihood of becoming obese. In the US, access to health care varies from state to state, despite efforts by the federal government to provide universal care. This observation can be illustrated by the fact that obesity levels vary from one region to another. Additionally, states with weak health infrastructure also have the highest obesity rates.
Goldstone (2015) demonstrates how access to healthcare may influence obesity by comparing the 20-and-above populations of Canada and the US. Whereas Canada has a public healthcare that focuses on universal coverage, the US healthcare system is individualized. By analyzing the each country’s healthcare system based on access, quality and patient satisfaction, Goldstone (2015) found that Americans in the specified age had a lower likelihood of having a personal doctor compared to Canadians. Further, it emerged that Americans had higher chances of having unmet needs relative to Canadians. While disparities in terms of income, race, and immigrant status existed in both countries, they were more emphasized in the US relative to Canada (Cole & Lobstein, 2012).
On the other hand, there are those who believe that health insurance encourages people to live less healthily since their healthcare is well catered for. Goldstone (2015) argues that as long as an individual’s insurance premiums are not risk rated against their being obesity, the said insurance only encourages them to overeat and ignore physical activity. They understand that any health risks they undergo will be taken out on the insurance cover. The rationale of this argument is that the existence of a safety net in the form of an insurance cover may only serve to cause people to live recklessly. While Goldstone’s (2015) hypothesis is not backed by any previous research, it may explain why people with high income, and hence access to healthcare, also tend to become obese.
Improvement in education is viewed as a way of countering the impact of the external influences that facilitate growth in obesity. The spread of obesity has been disproportional based on the level of education among other variables contained in the Grossman model. Stevens et al. (2012) believe that education presents a positive impact on the wellbeing of individuals, especially in poorer countries, where income disparity is prominent.
The assertion that education affects obesity offers a rationale for the government to intervene by increasing access to the same need. However, the mechanism by which the level of education influences obesity remains unclear. Education informs people’s lifestyles, including diet and exercise. In turn, it influences the chances of becoming obesity. Similarly, obesity is associated with labor market outcomes such as unemployment, which are also affected by education (Ogden et al., 2014).
Further, people who have studied for long are less likely to drink a lot or smoke. These two activities contribute to obesity. Besides, educated people are likely to exercise and/or seek preventive care such as vaccinations. This difference is more pronounced among women relative to men, with educated women being less likely to become obese compared to their educated male counterparts.
The Implications of the Problem for Health Services and Health Economics
Obesity is a chronic disease that has the potential to impair how a person’s body functions. However, the greatest concern with this condition is that it exposes an individual to other dangerous conditions such as heart diseases, Type II diabetes, and bone and joint pain. As the number of the 20-years-and-above individuals with obesity continues to increase across the world, people are forced to spend more on health care. Goldstone (2015) found that the medical expenditure for individuals with obesity was almost $750 more compared to those of people with average weight in the US.
Additionally, Daouli et al. (2014) argue that obesity was responsible for about a quarter of the total increase in healthcare costs in the US between 1987 and 2003. Additionally, the UK spends nearly £6 annually to combat diseases that are linked to obesity. This amount equals to about 7% of the UK’s total expenditure on health care. As the percentage of the GDP spent on healthcare continues to increase, other essential services such as education and research become deprived of funding. This situation may cause these services to stall or cause their delivery to become inefficient.
At the individual level, the increase in the cost of healthcare can lead to poverty. As stated earlier, the healthcare system in the US is private, meaning that patients have to pay from the pocket. If obese people pay more for healthcare relative to their average-weight counterparts, there is the likelihood that they will be unable to afford other basic services such as school fees for their children. Additionally, various social costs are associated with obesity.
They include poor workplace relationships due to low self-esteem and low earnings due to reduced morale to work (Stevens et al., 2012). Obese people may be frequently absent from their places of work due to the disease.
Further, employers face the increased burden of including a disability pension for their obese employees, owing to their frequent disease attack. The companies and the obese persons will suffer loss if such an individual dies prematurely of diseases such as heart attack. Additionally, job discrimination based on body weight is a common vice in the workplace. It may cause obese people to earn less relative to their counterparts. In addition, insurance companies charge higher premiums for health insurance for people who are overweight since (fat individuals) they are seen as being at a greater risk of becoming ill. Hence, obese persons have to spend an extra amount of money on health insurance compared to their healthier counterparts.
Another problem associated with obesity is that it causes the population of a country to become less healthy, hence leading to reduced productivity. As more people are booked in hospitals, healthcare facilities become strained. Obesity among the 20-and-above population can affect the funds that are set aside for research and treatment of more serious diseases such as cancer. This situation results in the disruption of the normal cause of operations in healthcare facilities due to the occurrence of a new disturbing trend. Besides, it takes time for the government to increase funding for healthcare to accommodate new diseases because passing legislations to authorize extra expenditure takes long to pass. During such period, the healthcare systems must adjust their budgets to accommodate the new trend of obesity, including the other diseases it causes.
Potential Outcomes, Solutions, and Policy Implications
Obesity affects almost all aspects of an individual’s life, as well as government policies. It is a major challenge in modern society, particularly because it has a possible positive impact. In addition to causing premature deaths, obesity may lead to decreased productivity in the workplace. This situation causes people to earn a low income. It is also a major cause of stigma and discrimination since obese people are viewed as unhealthy, hence undeserving of respect.
At the institutional level, employers and the government suffer the loss of income due to obesity. In the case of the employer, he or she has to include disability pension for his or her obese employees, a move that drives up the organization’s cost of operations. Additionally, employers must live under constant worry that they will lose their employees to premature death or impairment caused by obesity-related diseases. In the case of the government, policies must be enacted and extra funding set aside to cater for the treatment of obesity and related diseases.
The government benefits most from a healthy and hence a productive nation. As such, the government should come up with policies that seek to minimize the rates of obesity in the country. While increasing healthcare funding to accommodate the obesity has already occurred, there is a need to increase efforts to counter the disease that is killing the 20-and-above population. It is worth commenting that in some states such as Montana and New York, the rate of obesity has been experiencing a gradual decline in the recent times. Thus, the federal government must seek ways to enforce this trend across the country to ensure an overall reduction in obesity rates.
One way would be for the federal government to create an effective healthcare system care based on universal coverage. The private nature of healthcare in the US limits low SES people from accessing quality care and important advice on obesity. In contrast, Canada’s health care fosters universal coverage, which has enabled low SES individuals to attain proper information on how to avoid and/or manage obesity. The US government and other countries around the globe should also pay attention to the primary cause of obesity, namely, fast foods. In this respect, companies dealing in these types of foods should be held partly accountable for the high indigence of obesity. Secondly, the governments should promote education on the importance of healthy eating and exercise.
Conclusion
The last three decades have witnessed an increase in the proportion of the adult population (20 years and above) with obesity. Today, it is estimated that 1.9 billion adults are overweight. In the US, about 35 percent of the adult population is obese, a situation that has caused a strain on the country’s healthcare system. Particularly worrying is the fact that obesity leads to other often more serious diseases. Many factors are believed to contribute to obesity, among them, SES status, access to healthcare, the level of education, and gender. The Grossman model explores how these factors relate to the demand for healthcare to result in the various outcomes. These factors are interdependent on one another. The implications of obesity include increased costs of healthcare at the individual and institutional level, stigma, low productivity at the workplace, and importantly, the risk of premature death.
Recommendations
At the individual level, the solution involves healthy living by eating right and exercising. On the other hand, the government has the greater responsibility of ensuring that people live healthily. The first step is to ensure all citizens have access to health care with universal coverage. This plan will have the impact of making healthcare efficient to all people, regardless of their SES. Secondly, as stated earlier, the manufacturers of fast foods should be held more accountable for contributing to obesity rates. To begin with, the wrappers they use may include a warning that energy-dense foods pose a danger to the consumer’s body. Further, the taxes on energy-dense foods should be raised to cater for the extra healthcare costs that result from high obesity rates. Finally, nutrition education should be made compulsory at the elementary and high school levels to equip Americans with knowledge on the need for healthy eating.
References
Cole, T. J., & Lobstein, T. (2012). Extended international (IOTF) body mass index cut‐offs for thinness, overweight and obesity. Pediatric Obesity, 7(4), 284-294.
Cummins, S. (2014). Food deserts. Web.
Daouli, J., Davillas, A., Demoussis, M., & Giannakopoulos, N. (2014). Obesity persistence and duration dependence: evidence from a cohort of US adults (1985–2010). Economics & Human Biology, 12(1), 30-44.
Flegal, K. M., Kruszon-Moran, D., Carroll, M. D., Fryar, C. D., & Ogden, C. L. (2016). Trends in obesity among adults in the United States, 2005 to 2014. JAMA, 315(21), 2284-2291.
Goldstone, M. (2015). Access to healthcare and obesity: An international investigation of healthcare systems. Web.
Grossman, M., Tekin, E., & Wada, R. (2014). Food prices and body fatness among youths. Economics & Human Biology, 12(1), 4-19.
Ogden, C. L., Carroll, M. D., Kit, B. K., & Flegal, K. M. (2014). Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA, 311(8), 806-814.
Saffer, H., Dave, D., Grossman, M., & Leung, L. (2013). Racial, ethnic, and gender differences in physical activity. Journal of Human Capital, 7(4), 378-410.
Stevens, G. A., Singh, G. M., Lu, Y., Danaei, G., Lin, J. K., Finucane, M. M.,… Paciorek, C. J. (2012). National, regional, and global trends in adult overweight and obesity prevalences. Web.
Sturm, R., & Hattori, A. (2013). Morbid obesity rates continue to rise rapidly in the United States. International Journal of Obesity, 37(6), 889-891.
The American Diabetes Association. (2014). Standards of medical care in diabetes—2014. Diabetes Care, 37(1), 14-80.
Yoon, S. (2012). Finding food deserts based on food access index and transportation modes: Case study of Sarasota County, FL. Tallahassee, FL: University of Florida.