Introduction
With the increase in preterm birth and the high survival rate of infants with neuro-developmental impairment, the doctors have to provide parents with prognostic information for their infants. This is done with the help of neuro imaging or medical imaging (Horsch et al., 2010, p.1).
Medical Imaging has become an integral part of modern medicine. One can understand its huge benefits after he has experienced it and then analyzed it, whether it is a patient or a physician or a professional organization (Technology and Innovation, 2011, Para1). Medical imaging technology is used to take images of the inside of the body. “It is sometimes also referred as diagnostic imaging as it helps doctors to arrive at a diagnosis” (Smith, 2011, Page 1). Medical Imaging helps in detecting and diagnosing diseases at its earliest and treatable stage and helps in determining most appropriate and effective care for the patient (Technology and Innovation, 2011, Para 4).
“Medical imaging provides a picture of the inside of the body in a non-invasive way. These pictures can be used to identify unusual things inside the body, like tumors, broken bones, leaking blood vessels, etc. X- Ray is one of the most famous types of diagnostic imaging, it uses radiation to take a static image of a specific area” (Smith, 2011, Para 1).
Smith (2010, Para 1) states if we separate ultrasound from the technologies like X-Rays and CT that is computed tomography, it also aids in sensing body from inside. This is done with the help of bouncing sound waves and MRI, which is magnetic resonance imaging, shake the cells that helps in getting a picture of the inside of the body (Smith, 2011, Para 1). Medical imaging helps in creating dynamic images in motion that can be used in diagnosing such cases where static imaging cannot be used for any visualization (Smith, 2011, Para 1).
Research confirms that medical imaging not only improves health and save lives but also reduce health care costs and spending. Medical Imaging helps in diagnosing different internal organs of the body without the help of an invasive and risky surgical process, thus improving the chances of survival (Technology and Innovation, 2011, Para 5).
The power of medical imaging can be understood more clearly by the following research finding: (Technology and Innovation, 2011, Para 7).
- “Increased regular mammography screening rave resulted in a 24 percent decrease in the death rate from breast cancer from 1990-2004” (Technology and Innovation, 2011, Para 8).
- “Physicians have reported that for all cancers, PET scanning allowed them to avoid additional tests or procedures 77 percent of the times” (Technology and Innovation, 2011, Para10).
- “Increased utilization of advanced medical imaging, such as CT and MRI, between 1991 and 2004 improved life expectancy by 0.62 to 0.71 years. This effect was greater than the increase in mortality caused by obesity” (Technology and Innovation, 2011, Para11).
- “Imaging procedures such as CT, MRI, ultrasound, etc. diagnose and treat a wide range of diseases from cancer and appendicitis to stroke and heart disease and also looks for any signs of diseases or abnormalities in the fetus” (Technology and Innovation, 2011, para12).
The aim of the current study is to compare MRI and Ultrasound for determining abnormalities in preterm infants. For this purpose lots of surveys have been done and the findings prove the importance of both the methods of imaging.
Methods
MRI and Ultrasound
MRI refers to Magnetic Resonance Imaging; in the past years it was called Nuclear Magnetic Resonance Imaging (Ballinger, 2008, Para 1). Around 15 years ago ‘Nuclear’ was dropped off to avoid any confusion of its involvement with radioactivity (Ballinger, 2008, Para 1).
Unlike regular X- rays and CAT scans, MRI takes pictures of various parts of body without the use of x-rays. “The patient lies in the MRI scanner that consists of a large and very strong magnet. Signals are sent and received from the body with the help of radio wave antenna. The computer attached to the scanner converts the returning signals into pictures” (Ballinger, 2008, Para 2). MRI can take pictures of any part of the body at almost any angle (Ballinger, 2008, Para 2).
High frequency sound waves are used in ultrasound to create visual images of tissues, organs or blood flow inside the body (What is Ultrasound (Sonography), 2011, p.1). “Similar to MRI it is non-invasive, involves no radiation (like x-ray) and avoids other hazards like bleeding, infections or reactions to chemicals of other diagnostic methods” (What is Ultrasound (Sonography), 2011, p.1)
Findings
Abnormal Neonatal Course
Perinatal Asphyxia that has been severe to cause neurologic deficits can be detected by an abnormal neonatal course. These symptoms could be in the form of delayed or impaired respiration requiring resuscitative measures like intubation or ventilation. Also delayed Apgar scores, is 3 or less for more than 10 minutes, can develop neurologic complications, like neonatal seizures, and finally evolution of cerebral palsy. However, perinatal asphyxia cannot be solely indicated by a low Apgar score as there could be other factors for low score like brain malformation, maternal drugs or anesthesia (Menkes et al, 2006, p 405).
During the neonatal period other visible abnormalities include seizures, hypotonia and a bulging fontanel. Irritability, feeding difficulties, excessive jitters or abnormal cry is some less obvious abnormalities (Menkes et al, 2006, p 405).
Neonatal cranial ultrasound has become the first choice for detecting brain injury especially in such preterm infants those who have high chances of it. Through this method the examinations can be repeated as much time as we want without affecting weak infants. Since the last few years, MRI has been providing high resolution for imaging of the brain as all the parts are easily visible through it. But simultaneously it has also been observed that this method of imaging is time consuming and most of the time it is not available repetitively (Rademaker et al., 2005, p. 489).
Medical imaging studies suggesting Prenatal Asphyxia
Prenatal Asphyxia can be detected to some extent by the examination of CSF, but a normal CSF does not exclude the possibility of prenatal asphyxia (Menkes et al, 2006, p 405).
Ultrasound scans are most commonly used to determine the extent of an intracranial hemorrhage. These scans can be done at the bed side without any harmful effects to the infant. “These scans provide excellent visualization of the ventricular system, basal ganglia, choroid plexus and corpus callosum” (Menkes et al, 2006, p 406).
In the preterm infants ultrasound is useful in providing prognostic information during the neonatal period. Horsch et al (2010, p.1) states that “It helps in detecting major intracranial wound, like intraventricular hemorrhage, parenchymal hemorrhagic infractions or cystic periventricular leukomalacia all indicating the development of cerebral palsy and severe cognitive impairment” (Horsch et al, 2010, para.1).The main advantage of Ultrasound is that it is fast and inexpensive and can be done at the bedside without any side effects (Horsch et al, 2010, para.1).
Horsch et al (2010, p.1) mentions that Conventional MRI and cUS (cranial ultrasound) were previously compared in preterm infants. Horsch et al (2010, p.1) further states “Woodward, in a recent study, demonstrated that abnormal findings on cerebral MRI at term equivalent age predict adverse neuro-developmental outcome at 2 years of age significantly better than cUS” (Horsch et al, 2010, para.1).
This type of finding insists us to mull over whether MRI can be used as a screening tool for all preterm infants. “However, the information generated from cUS at term age, in the studies of Woodward, was not taken into account as cUS scans were done only in the first 6 weeks of life and not in parallel to the MRI at term” (Horsch et al, 2010para.1). Also, MRI is an expensive, time consuming and resource consuming technique is not available in all hospitals and, where available, the waiting list is very long (Horsch et al, 2010para.1).
MRI versus Ultrasound in preterm infants
Conventional MRI is supposed to be superior to cranial ultrasound that is helpful in identifying white matter abnormalities and then analyzing effects in preterm infants (Horsch et al, 2010, 2010, para.1)
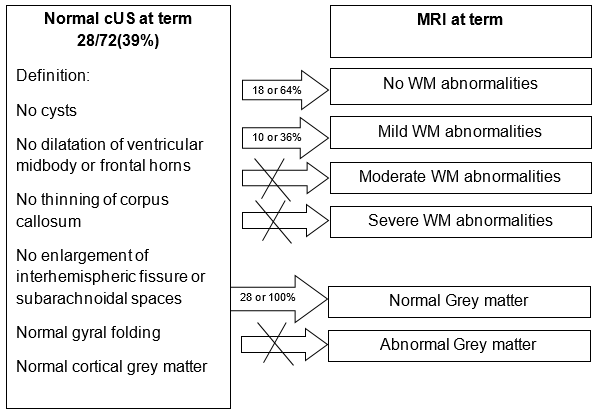
Based on the study done in Stockholm from August 2004 to November 2006 on all infants born with GA below 27 weeks, “all infants with severe abnormalities (n=3) were scored as severely abnormal on cUS and MRI” ” (Horsch et al, 2010, Para 3). Horsch et al (2010, p.3) discovers that out of 28 infants with normal ultrasound at term age, 18 had a completely normal MRI and 10 had only mild WM abnormalities on MRI. Thus, none of the infants who went through normal cUS had any severe WM abnormalities or abnormal grey matter (shown in Table 1). “In all, 10 infants who were scored as normal on MRI were scored as mild to moderate in cUS” (Horsch et al, 2010, Para 3).
“In four infants small punctuate cerebellar hemorrhage was diagnosed using MRI while no hemorrhage were diagnosed using cUS” (Horsch et al, 2010, p.3).
Earlier also there had been systematic comparison between cUS and MRI. Horsch et al (2010, p.4) further mentions that Woodward feels that MRI could predict better results of adverse neurodevelopment and cerebral palsy at 2 years than ultrasound. Still, in Woodward’s studies the sensitivity of cUS was inferior compared to results published by other groups, possibly, due to a major difference in both study patterns.
“Woodward did only 3 ultrasounds within the first 6 weeks of life while the other group by De Vries scanned weekly from birth until term age” (Horsch et al, 2010, p.4). “Information about impaired brain growth, diffuse grey and WM loss can be detected by late cUS, as it is proven that signs of poor brain growth are related to adverse neuro-developmental outcome at 3 years” (Horsch et al, 2010, p.4). Hence it is difficult to establish the superiority of MRI at term to sequential cUS from birth to term (Horsch et al, 2010, p.4).
MRI and cUS both methods showed similar severe abnormalities. “Moreover, cUS’s at term age was normal for approximately 40% of extremely low gestation age infants and also MRI did not show moderate or severe WM abnormalities or abnormal grey matter” (Horsch et al, 2010, p.4). As a result, “all infants with normal cUS have either normal MRI which was 64% or only mild which was 36% WM abnormalities on MRI” (Horsch et al, 2010, p.4).
There had been many studies to identify and compare the cUS and MRI in determining abnormalities in preterm infants. Inder et al (2003, p.1) states that one such study, whose purpose was to assess the sensitivity and specificity of cUS during the first 6 weeks of life in comparison with MRI at term, was done, in describing the presence of WM injury in a group of 96 very low birth infants (Inder et al, May 2003, p.1).The results of this study are defined in the Table 6; Table 7 and Table 8. The study concluded that though “neonatal cUS of the VLBW infants showed high reliability in detecting cystic WM injury but has limitations in showing of non-cystic WM injuries”. As non-cystic WM injury is more common than cystic WM injury, this deficiency of neonatal cUS is important (Inder et al, May 2003, p.1).
The study was done on a large unselected group of VLBW infants. It shows that the “finding of cUS WM echo densities lacks sensitivity and positive prognostic assessment for the existence of WM injury but was clearly highlighted by MRI at term” (Inder et al, May 2003, p.1). Here a clinician has restrictions to exactly diagnose this common cerebral disease in premature infants who suffer severely (Inder et al, May 2003, p.1).
Discussion
“Hence it can be stated that conventional MRI adds marginally clinically relevant information to the infants with normal cUS at term age” (Horsch et al, 2010, p.4).This means that for identifying low risk of severe disabilities in infant ultrasound can be equally beneficial and cost effective than conventional MRI. Also, MRI is an expensive, time consuming and resource consuming technique, is not available in all hospitals. The study is based on the results of cUS and conventional MRI. The results of much advanced MRI methods such as diffusion tensor imaging, volumetry, tractography, spectroscopy and functional MRI will definitely be more precise and accurate in diagnosing the symptoms at an earlier stage in infants (Horsch et al, 2010, p.4).
A series of studies which have been done within the span of 30 years have proved that a normal ultrasound scan can be very effective in establishing the outcome of a normal neuromotor development in an infant (Nongena et al., 2010, p.1). Nongena et al (2010, p.1) further mentions that “the accuracy is high: in one typical study the PPV was 99% (95% CI 98% to 99%); combining suitable studies, the pooled probability for normal outcome was 94% (95% CI 92% to 96%), though heterogeneity between studies was high at 88%” (Nongena et al., 2010, p.1).
“Normal cognitive function was predicted by a normal ultrasound with a PPV of 77% (95 CI 74%to 80%) in another typically large study” (Nongena et al., 2010, p.1). “The pooled probability was 82% (95% CI79% to 85%) of a normal cognitive outcome of a normal ultrasound scan” (Nongena et al., 2010, p.1)
In different studies using Grade 1 or 2 IVH, Grade 3 IVH, Grade 4 IVH, cystic PVL, Ventricular dilatation, post hemorrhagic hydrocephalus, etc. showed varied results confirming the accuracy of diagnosis done by normal ultrasound. Shown below, in Table 2, prediction of abnormal neuromotor function by cranial ultrasound (Nongena et al., 2010, p.2)
Table 2 : Prediction of abnormal neuromotor function by cranial ultrasound (Nongena et al., 2010, p.2)
MRI or Magnetic Resonance Imaging
Comparatively fewer studies have tried to assess the value of MRI for predicting abnormal motor development or cognitive impairment. Here also different imaging and outcome criteria are used which is similar to ultrasound studies. Below defined are the results of studies using widely available MRI techniques (Nongena et al., 2010, p.2).
White Matter Abnormalities
Woodword premeditated the existence of white matter abnormalities to tell long term neurodevelopment consequences. This he did after using a blend of imaging appearances. “Using a white matter grading score ranging from normal to moderate to severe, the PPV of moderate to severe white matter abnormalities for abnormal motor development was 31% (95% CI17% to 49%) and for cognitive impairment was 34% (95% CI 20% to 52%)” (Nongena et al., 2010, p.2). “Combined studies suggested that moderate to severe white matter abnormalities predicted abnormal neuromotor development with a pooled probability of 35% (95% CI 19% to 55%) and cognitive impairments with a pooled probability of 52% (95% CI 36% to 67%)” (Nongena et al., 2010, p.2).
Ventricular Enlargement
“In one study, ventricular enlargement with a ventricular diameter >8mm predicted long-term neurodevelopmental impairment with a PPV of 86% (95% CI 42% to 99%)” (Nongena et al., 2010, p.2). “Another study found that a combination of ventriculomegaly and white matter abnormality predicted abnormal motor development with a PPV of 55% (95% CI 23% to 85%)” (Nongena et al., 2010, p.2).
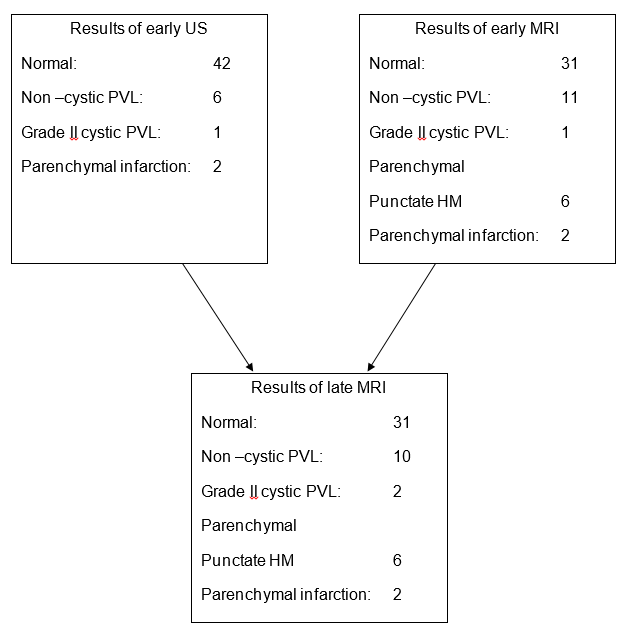
Another study done by T. Debillion, S N’Guyen, A Muet, J C Roze, of Neonatal Intensive care unit, University Hospital, Nanates, France shows the result in the below mentioned table 3, 4 and 5. The main objective was “to compare the accuracy of US and MRI in diagnosing white matter abnormalities in preterm infants and to determine the specific indications for MRI” (Debillon et al., 2003, p.1).“The early Us and MRI findings correlated closely for severe lesions but not for moderate lesions” (Debillon et al., 2003, p.1). “Overall, early MRI findings predicted late MRI findings in 98% of patients (95% CI89.5% to 99.9%) compared with only 68% for early US (95% CI 52.1% to 79.2%)” (Debillon et al., 2003, p.1).
Conclusion
Many different studies regarding both the methods sturdily favor Ultrasound which is highly effective in sensing severe abrasions of white matter in preterm infants, but such studies equally give weightage to MRI that is useful for the diagnosis of less severe damage (Debillon et al., 2003, p.1). If MRI is done within the three weeks of life, it is very effective of the final diagnosis at term (Debillon et al., 2003, p.1).
Though ultrasound seems to be preferred method of imaging for detecting CNS pathology in preterm infants as it is a sensitive matter to detect hemorrhagic lesions and ventriculomegaly, yet current reports support MRI since it can detect a great range of ‘white and gray matter abnormalities’ which are not possible through ultrasound scanning. Some suggest that MRI should be on a routine basis for preterm babies that helps in prognostication (Dunn, 2010, Para 5).
List of References
Bellinger, R. 2008. “What is MRI.” MRI Tutor. Web.
Debillion et al, 2003. “Limitations of ultrasonography for diagnosing white matter damage in preterm infants.” Arch Dis Fetal Neonatal Ed; 88:F275-F279.
Dunn, M. 2010. “Ultrasound versus MRI at term.” Neo Notes Journal Club. Web.
Horsch et al, 2010. “Cranial ultrasound and MRI at term age in extremely preterm infants.” Arch Dis Child Neonatal Ed; 95:F310-F314.
Inder, T E. 2003. “White Matter Injury in the Premature Infant: A Comparison Between Serial Cranial Sonographic and MR findings at Term.” AJNR Am J Neuroradiol 24:805-809.
Menkes, J H. et al. 2006. “Child Neurology.” Lippincott Williams & Wilkins. Philadelphia. P.1186.
Nongena et al. 2010. “Confidence in the prediction of neurodevelopmental outcome by cranial ultrasound and MRI in preterm infants.” Arch Dis Child Fetal Neonatal Ed. Vol 95. No. 6.
Rademaker et al, 2005. “Neonatal cranial ultrasound versus MRI and neurodevelopmental outcome at school age in children born preterm.” Arch Dis Child Neonatal Ed; 90:F489-F493.
Smith, S E 2011. “What is Medical Imaging.” WiseGeek. Web.
“Technology & Innovation.” 2011. MITA. Web.
“What is Ultrasound (Sonography).” 2011. ARDMS. Web.