Introduction
Chronic kidney disease (CKD) is the impairment of renal function that has adverse outcomes for the overall health and leads to ESRD (end-stage renal disease). According to Kazley, Hund, Simpson, Chavin, and Baliga (2015), today, the disease affects “nearly 5.5 million Americans” (p. 85). The situation when the kidneys are functioning at their minimum capacity has two solutions – dialysis and kidney transplantation, neither of which is cheap or easy for the patient.
A kidney transplant is generally preferred over dialysis as it provides better health outcomes and longer life expectancy. However, transplantation is a lengthy and costly process that requires measuring and controlling a number of health parameters. Although quality of life improves significantly after transplantation, people still need to adhere to specific rules to prevent kidney rejection. As the immune system struggles to fight a new organ, people need to take immunosuppressive medication and follow a special diet. A well-designed nutrition plan is the best option to mitigate the side effects of immunosuppressant drugs.
Specific renal diets focus on the factors that reinforce kidneys’ well-being, manage microelements reduced or increased by medication, and control macronutrient intake. The overall nutrition level is the primary factor to consider, as both over- or undernutrition can worsen health outcomes. Meeting protein requirements is essential at all the stages of post-surgery treatments, as it helps to enhance wound healing and prevents muscle breakdown caused by prednisone. Management of sugar, sodium, and potassium intake is a typical characteristic of a renal diet. Moreover, kidney disease is often accompanied by different health conditions, such as diabetes or heart problems that put additional requirements on a diet.
Although renal diets are necessary components of the post-transplantation stage of treatment, they are often perceived as complicated and unclear for the patients resulting in non-adherence. The study of CKD patients conducted by Lambert et al. (2019) demonstrated critical rates of dietary non-adherence, finding that only 32% of the analyzed population follow their diet plans correctly. Scholars also suggest that post-transplantation patients have lower adherence due to the reduction in symptoms and improved quality of life (Lambert et al., 2019). People violate their diet plans due to multiple reasons.
They often cannot assess their health condition and what outcomes improper nutrition might have on their body. The problem of low levels of overall health literacy of the population significantly contributes to non-adherence. Thus, patient education before the discharge and subsequent long-term communication about a renal diet is a fundamental solution to enhance renal diet efficiency.
The primary step of patient education should address the way the organism functions after the transplantation and how different drugs affect it. Sharing such information is necessary to motivate people to follow their nutrition plans and prioritize their diets. The key goals of such an education are to develop lasting and strong knowledge and to provide the support that enhances adherence. The educational program based on visual aid can help to achieve the desired effect. Such resources can include the lists of foods that are to be eaten or excluded from the menu. Sharing the information in such a format is easy for comprehension and memorizing. Moreover, patients can take the schemes and lists home to consider them when choosing foods.
Problem Statement
Dietary non-adherence among post-transplantation patients compromises treatment efficiency and is often caused by limited knowledge and low overall health literacy. Moreover, patients often show a lack of motivation to follow a renal diet due to a misunderstanding of its necessity. Such factors cause adverse health outcomes for the patients who suffer from side-effects of immunosuppressive treatment along with diabetes or heart problems and even lead to organ rejection.
Current patient education programs are not enough to accomplish the tasks. That is why new approaches are needed to enhance patient knowledge and adherence. The problem is complicated by the fact that healthcare workers often feel resistant to changes because of the discomforts they add to the daily challenges (Ellis & Abbott, 2018). Lewin’s model that implies unfreeze-change-freeze stages will be applied for the introduction of new approaches. A visual aid, which patients find easy to interpret, can be used to explain what products have to be limited and what should be consumed.
Background
Following a prescribed nutrition plan reinforces one’s chances to have a successful post-transplantation therapy. However, a problem of dietary non-adherence among renal patients is clamant today, and it often compromises positive health outcomes. The scholars assume that there is a distinct connection between non-adherence and low health literacy of the population (Lambert et al., 2019). According to Escobedo and Weismuller (2013), almost 50% of Americans have difficulties with meaningful participation in making decisions about their healthcare. These problems mainly include the inability to “fully understand informed consent for procedures, and effectively follow health care recommendations and treatment” (Escobedo & Weismuller, 2013, p. 47). Many patients find the information given in their treatment centers overwhelming and need additional guidance to navigate through it.
Specific education interventions are designed to teach patients about renal diets before discharge from a medical institution. They receive the information about the products and nutrient levels they need to consume to mitigate side effects of immunosuppressive treatment and to “prevent obesity, hyperlipidemia, hypertension, diabetes, and osteoporosis” (Hong, Kim & Rha, 2019, p. 75). However, without proper knowledge about food, calories, protein, and micronutrients, people find it confusing to follow the prescriptions. Given the inability to interpret food labels and to assess food components and their quantity in a serving, the information shared in treatment centers should be simplified and visualized.
The problem of non-adherence has a number of severe implications that include potential kidney rejection, obesity, and illnesses related to the immunosuppressant regimen. The stress caused by the surgery and the need for recovery and healing increase the caloric requirements. Pedrollo et al. (2017) claim that the first year after the transplantation is often characterized by excessive weight gain that leads to health complications, including cardiovascular events and graft loss. According to Hasse (2001), “severe obesity may decrease graft function and survival in kidney transplant recipients” (p. 120). That is why weight management is a key component of the renal diet alongside with micro and macronutrient intake.
Currently, U.S. transplantation centers offer extensive education programs about nutrition after getting a new kidney. Such training focuses on the explanation of the therapeutic purpose of the diet, the recommended nutrient intake at each of the treatment stages, food restrictions, and glucose control. Nevertheless, the efficiency of this training is questioned regarding low diet adherence levels. Despite sharing useful information, modern renal diet education fails to increase patient engagement.
The knowledge of complicated processes is inaccessible for people with a limited understanding of basic concepts and low health literacy levels. Furthermore, patients find it challenging to communicate with medical staff about their care, as they have a limited understanding of what they might ask. Many of them report shame and confusion caused by insufficient knowledge, so it is difficult for them to engage in healthcare decisions (Lambert et al., 2019). Moreover, current education programs do not focus on empowerment and motivation, which might tackle the uncertainty and confusion.
The described above situation suggests that the current approach to patient education about the renal diet should be improved. Kazley et al. (2015) suggest that “clinicians should keep health literacy limitation in mind when presenting information to patients” (p. 89). Facing this problem is the first step to the development of an accessible education plan that would adapt to the needs of patients with limited health literacy. Moreover, group education should be combined with individual sessions where the patients would have the opportunity to ask questions regarding the personal details of their health. Lastly, motivation and empowerment should be integrated into the teaching process to encourage patients to seek information, ask questions, and make adequate health-related decisions.
The main concern of the recommendations for the quality improvement of patient education intervention is the adaptation of the material to patients’ health literacy levels. The use of visual aid can improve understanding of the provided information and enhance memorization. Escobedo and Weismuller (2013) state that visual aid is a helpful method to improve patient comprehension and communication. Moreover, patients can take home different schemes and checklists and consult every time before cooking, taking a serving of a meal, or going to shop for groceries. Sharing additional information sources, useful applications for tracking calories and nutrient intake can increase the likelihood of patient adherence to the diet.
Purpose
The project is conducted to promote a quality improvement intervention in a medical center that focuses on patient education after kidney transplantation. The main goal is to raise awareness of a dietary non-adherence problem and justify the need for change in the current education system. The goal will be achieved with the help of visual aid that teaches patients about food recommendations and restrictions before and after kidney transplant. As there is a connection between low health literacy and non-adherence to treatment and diet, simple graphs and images will provide concise and understandable information for patients with different educational opportunities. Moreover, they will suggest that diet management is not as overwhelming as it seems, and thus provide empowerment and motivation.
The project is essential for nursing as it advocates for improvements, facilitates progress, and promotes evidence-based transformation. According to Lewin’s unfreeze-change-freeze theory, the initial step implies the problem statement that aims at convincing the staff about the necessity of the change.
Analyzed evidence from the recent research provides justification for the project. The current education model should be adapted concerning the health literacy issue, and a visual aid is a recognized tool that allows this adaptation. According to Ellis and Abbot (2018), the ‘change’ stage of the model is when kidney center staff is likely to “feel resistant to adjustments” (p. 331). The reference to evidence is the tool that can motivate people to pursue the change. The final stage of the intervention implies collecting qualitative feedback from the patients.
The Nature of the Project
The project has an innovative nature, and it aims at bringing changes to the medical environment by introducing new ways of patient education about the renal diet. Transforming the existing processes is a challenging task that is often met with resistance, stress, and low support of healthcare workers. According to Lewin’s model, the changes have to be implemented in three stages, which are unfreezing of the old shape, the change itself, and freezing that fixes the new form (Ellis & Abbot, 2018).
That is why this project is going to consist of three steps. At the initial stage, it is necessary to ‘unfreeze’ the existing model, understand its drawbacks, develop a plan for the improvement, and convince the staff to support it. The second phase is crucial as it implies the change itself. Lastly, successful transformations should be consolidated to ensure that the improvement will not be abandoned.
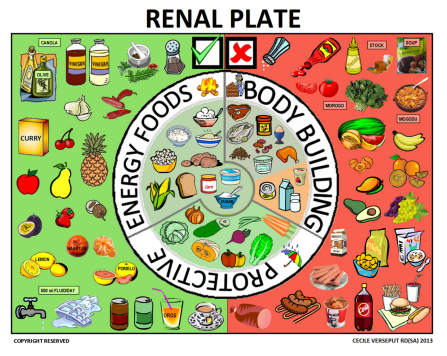
The design of the visual aid tool that addresses all the issues missing from the previous education program is a crucial element of the first stage. The fundamental requirement for a visual aid tool is to make the presented information clear, simple, and concise. Verseput and Piccoli (2017) suggest the use of the so-called ‘renal plate’ for the education of patients with CKD (Figure 1). The green side depicts the foods that can be eaten, while the restricted products are placed on the red side. The visual aid tool will be presented as relatively small 6x10in postcards with the renal plate on one side and a list of recommended foods organized according to different product groups on the other. The additional motivation aspect of the design is to include more products on the allowed list while keeping the restricted food count lower.
The idea is to make the postcard useful for patients in everyday life. While they can easily forget the information presented to them on the slides in the care unit, this simple solution will remind them what foods to pick. The size was chosen so that the images were comfortable for practical use by the patients. They can stick them on the fridge and consult the lists while cooking, or they can take them along when going to shop for food. Given the relatively low health literacy, it is better to provide patients with ready solutions that are always at hand, than to spend hours teaching complicated concepts to them.
At the second stage of the transformation process, the change takes place, which in the case of this project, implies the education procedure and the feedback collection among the education intervention participants. At this stage, it is necessary to gain the support of the staff. Although the changes seem burdensome and cause additional concerns to the daily tasks, testing the new model, and finding the meaning in it will result in the acceptance (Ellis & Abbot, 2018). For these purposes, the intervention itself will perform the role of a test, and the process of feedback collection will help to find a meaning of the improvement.
The visual aid will be presented and explained additionally to the routine education procedure, while the printed version of the scheme will be distributed among patients for further use. The patients who will consent to engage in the interviewing will be asked five questions regarding their experience with a visual aid. The extensive feedback and commentary will be encouraged. The main message of the questions will be to evaluate how visual aid contributed to a routine education procedure. These questions are listed below:
- Assess how the visual aid tool clarified your understanding of the renal diet.
- How do you see the further practical use of visual aid?
- How has the visual aid influenced your motivation to self-manage your nutrition?
- What details of the visual aid do you find the easiest to memorize?
- What information do you find missing from the scheme?
The ‘freezing’ stage is crucial for the improvement intervention as it helps to consolidate the success of the change process. In the case of this project, it has a double purpose. First, it is vital to motivate the nurses to include the new approach to the routine education program for all patients and will use it in the future. For this purpose, the nurses should be taught additionally on how to speak with the patients about their nutrition management with the help of the visual aid.
Secondly, the results of the intervention will be reinforced through the follow-up patient screening about the use of the visual aid. The future recommendation for the nurses is to provide reminders for the patients about the use of the tool, answer their questions, and monitor the adherence to the recommendations. This stage is necessary to prevent patient readmission and promote adherence. Moreover, the follow-up will help to detect the issues and the limitations of the intervention that will facilitate further improvements.
Research Question
The research question for the project is:
How will the implementation of visual aid in a routine patient education session improve the dietary adherence and understanding among the patients after kidney transplantation?
The question is derived from these hypotheses:
- The renal diet adherence depends on how well patients comprehend the prescriptions and how motivated they are to follow them.
- The use of visual aid simplifies the presented information and makes it easier to understand for the patients.
Summary
The problem of dietary non-adherence among patients who have undergone kidney transplantation is urgent and requires immediate attention. It poses a significant threat to patients’ health outcomes and bears an unnecessary burden for the healthcare system. The research background suggests that limited health literacy is the primary reason why people find it challenging to follow their diet. The project aims at the exploration of the potential influence of education interventions on the understanding of posttransplant nutrition and the ability of this change to improve adherence.
Literature review
Introduction
This chapter intends to review the literature that constitutes the evidence for the project. The section is designed to summarize the historical scope of the problem and synthesize recent findings. The current state of research provides evidence that supports the need for change in patient education about renal diet. The studies prove the connection between health literacy and patient outcomes, thus emphasizing the significance of the problem. Current findings suggest that dietary non-adherence is the clamant issue that can be solved through improved patient education programs.
Historical Overview
Chronic kidney disease has long been burdensome for the U.S. healthcare system. That is why many studies were focused on treatment recommendations that help to improve health outcomes. The importance of nutrition management after kidney transplant is currently recognized with numerous researches studying specific aspects of the problem. Zeltzer, Taylor, and Tang (2015) analyze these studies and conclude that the majority of publications address short-term interventions during the acute phase, while a limited group of scholars explores long-term nutrition management.
Kazley et al. (2015) claim that the issue of non-adherence to renal diets is the subject of even fewer studies. However, most of them have been conducted recently, and the tendency suggests that the attention to the problem escalates. Several studies have been published recently that asses the state of health literacy among renal patients and its impact on health outcomes. Some scholars have also designed educational interventions that explore the potential of teaching and empowerment to solve the problem of non-adherence.
Current Findings
Understanding the importance of nutrition following kidney transplantation is an essential aspect of the problem statement of this research. The exploration of the renal diet and its impact on the recovery after the surgery and long-term nutrition plan for the patients with new kidneys has been a subject of several studies. Hasse (2001) investigates the literature regarding nutrition support of the patients on different stages of transplantation and summarizes the recommendations for dietary interventions.
The researcher highlights the importance of pretransplant nutrition support aimed at the “include optimization of nutritional status and treatment of nutrition-related symptoms induced by organ failure” (p. 120). The proposed guidelines also focus on the posttransplant nutrition support that provides electrolyte management, controlling glucose levels, and enhancing wound healing.
Weight gain is a factor that compromises positive health outcomes for many posttransplant patients. Pedrollo et al. (2017) designed a randomized clinical trial to address the issue and to discover the solution. The sample of 120 patients two months after the kidney transplant complied with a specific high protein diet based on foods with low glycemic-index. The patients underwent 12 months of observation to “evaluate the effect of a high protein and low glycemic-index diet on preventing weight gain after kidney transplantation” (Pedrollo et al., 2017, p. 1). The scholars concluded that long term increased protein intake is connected to weight loss among posttransplant patients. Thus, weight control is another goal of renal diet after kidney transplantation that can be achieved through protein intake management.
Nutrition management after kidney transplantation should go beyond the post-surgery recovery period and continue during the entire patient’s life. However, Zeltzer et al. (2015) claim that there are few studies addressing long-term dietary interventions after organ transplantation. The scholars have conducted a literature review research to find evidence on the impact of nutrition management more than a year after transplantation. Zeltzer et al. (2015) claim that compliance with the dietary prescriptions is significantly lower in long-term interventions than in those that focus on the post-surgery period.
The previously discussed studies justify the effectiveness and necessity of diets for patients undergoing kidney transplantation. Nevertheless, people often do not adhere to prescribed renal diets. Scholars often connect non-compliance with dietary prescriptions to low health literacy of the population. Escobedo and Weismuller (2013) conducted a study of 44 patients in a single treatment center in California to investigate the health literacy level among patients with kidney transplantation or renal failure.
The study showed that 41% of the population had insufficient health literacy levels. The researchers report that limited health literacy poses a threat to health and is connected to poor adherence to the prescribed treatment, increased healthcare costs, and health disparities (Escobedo & Weismuller, 2013). Thus, the study proves that inadequate health literacy compromises adherence and leads to adverse health outcomes.
Given that the health literacy rates are low, it is essential to investigate the health risks of this phenomenon for kidney transplant patients. The purpose of the cross-sectional study by Kazley et al. (2015) was to “assess the relationship between health literacy and transplant outcomes” (p. 85). The sample of 92 people consisted of equal groups of dialysis, posttransplant, and pretransplant patients in a single transplant center. The researchers found a direct relationship between health literacy and positive transplant outcomes, thus highlighting the importance of this factor for patient management and education.
The previous studies provide evidence that health literacy is a pressing problem among kidney transplant patients. As there is a connection between diet and treatment non-adherence and low health literacy, patient education programs should be designed to tackle this issue.
Thus, several education interventions have been conducted recently to evaluate what measures can close the gap in health literacy. Lambert et al. (2019) suggest that difficulties in communication with healthcare professionals combined with low health literacy lead to dietary non-adherence. The scholars developed a list of questions about a renal diet that would facilitate dialogue. A qualitative study of eighteen patients showed that they found the question list to be an efficient tool to guide communication about one’s nutrition (Lambert et al., 2019). The prompt list demonstrated that the use of additional tools and resources could provide guidance for the patients, give them confidence, and motivate them to be engaged in their treatment.
Several studies consider the role of dietitians in patient education. Tsai et al. (2015) developed a survey of the specific training conducted by dietitians in addition to the routine program. Scholars found that the experimental interventions positively influenced dietary adherence (Tsai et al., 2015). Lambert, Mansfield, and Mullan (2018) have conducted a qualitative study to explore what experience renal dietitians have regarding patient education.
The interviewed healthcare professionals described the process as challenging, both professionally and emotionally. The key difficulty lies in simplifying complexity as the majority of the patients find renal diets “burdensome, challenging and overwhelming” (Lambert et al., 2018, p. 126). The participants have reported that empathy and empowering are essential when communicating with patients. A Korean-based case study by Hong et al. (2019) demonstrated that comprehensive training that combines both individual sessions and group education enhances understanding and promotes dietary adherence.
Visual aid is assumed to be a useful tool for patient education in the context of low health literacy. The research by Verseput and Piccoli (2017) has a particular value, proving the efficiency of such interventions. The scholars suggest using a specially designed ‘renal plate’ that graphically demonstrates what foods are preferable for patients with kidney disease. The research took place in South Africa in a complex cultural environment and aimed to target various population groups.
Verseput and Piccoli (2017) conclude that “simple visual aids may be of great help not only in recalling diet-related concepts but also in reassuring patients, thus ensuring empowerment and compliance even in difficult settings” (p. 11). Similar images can be used to demonstrate the principles of posttransplant nutrition, as they can provide understandable and straightforward guidelines and empowering patients to self-manage their diets.
Conclusion
The literature review section contributes to the project by providing evidence that supports the problem statement. The analyzed studies justify the importance of dietary adherence to the health outcomes of patients after kidney transplantation. The current findings prove the hypothesis that misunderstanding of the concepts and low health literacy negatively affect patient adherence to the renal diet. They also provide an overview of educational interventions that focus on adapting patient education to correspond to the requirements of patients with limited levels of health literacy.
Summary
Although renal failure and its treatment are extensively presented in the scholarly literature, it is only recently that attention has shifted towards patient education and health literacy problem. The current studies provide an analysis of these factors and their influence on adherence to diet and therapy. Based on these findings, different investigations have been developed to design interventions that remove barriers to understanding. Thus comprehensive education programs, question checklists, patient guides, ad visual aid proved to be efficient in closing the literacy breach.
References
Ellis, P., & Abbott, J. (2018). Applying Lewin’s change model in the kidney care unit: Movement. Journal of Kidney Care, 3(5), 331-333. Web.
Escobedo, W., & Weismuller, P. (2013). Assessing health literacy in renal failure and kidney transplant patients. Progress in Transplantation, 23(1), 47-54. Web.
Hasse, J. M. (2001). Nutrition assessment and support of organ transplant recipients. Journal of Parenteral and Enteral Nutrition, 25(3), 120-131. Web.
Hong, S. H., Kim, E. M., & Rha, M. Y. (2019). Nutritional intervention process for a patient with kidney transplantation: A case report. Clinical Nutrition Research, 8(1), 74. Web.
Kazley, A. S., Hund, J. J., Simpson, K. N., Chavin, K., & Baliga, P. (2015). Health literacy and kidney transplant outcomes. Progress in Transplantation, 25(1), 85-90. Web.
Lambert, K., Lau, T. K., Davison, S., Mitchell, H., Harman, A., & Carrie, M. (2019). Development and preliminary results on the feasibility of a renal diet-specific question prompt sheet for use in nephrology clinics. BMC Nephrology, 20(1), 1-8. Web.
Lambert, K., Mansfield, K., & Mullan, J. (2018). Qualitative exploration of the experiences of renal dietitians and how they help patients with end-stage kidney disease to understand the renal diet. Nutrition & Dietetics, 76(2), 126-134. Web.
Pedrollo, E. F., Nicoletto, B. B., Carpes, L. S., Júlia De Melo Cardoso De Freitas, Buboltz, J. R., Forte, C. C., … Leitão, C. B. (2017). Effect of an intensive nutrition intervention of a high protein and low glycemic-index diet on weight of kidney transplant recipients: study protocol for a randomized clinical trial. Trials, 18(1), 1-6. Web.
Tsai, W.-C., Yang, J.-Y., Luan, C.-C., Wang, Y.-J., Lai, Y.-C., Liu, L.-C., & Peng, Y.-S. (2015). Additional benefit of dietitian involvement in dialysis staffs-led diet education on uncontrolled hyperphosphatemia in hemodialysis patients. Clinical and Experimental Nephrology, 20(5), 815-821. Web.
Verseput, C., & Piccoli, G. (2017). Eating like a rainbow: The development of a visual aid for nutritional treatment of CKD patients. A South African Project. Nutrients, 9(5), 435. Web.
Zeltzer, S. M., Taylor, D. O., & Tang, W. W. (2015). Long-term dietary habits and interventions in solid-organ transplantation. The Journal of Heart and Lung Transplantation, 34(11), 1357-1365. Web.