Abstract
The report provides the results of the research carried out at two Indiana nursing homes with the help of the specially developed questionnaire. The research is focused on analyzing the impact of economic factors on the level of care provided by the facilities. The report highlights the problem of staff shortage in Indiana facilities and the importance of its solving.
Introduction
Recently Indiana has got the dramatically low ranking in terms of long-term health care: the state’s nursing houses have performed incredibly badly in terms of staff time spent per patient and increased several deficiencies, having deserved the status of the most poor-quality facilities in the USA. About 28% of Indiana’s nursing houses have been given the lowest grade of one star (Gillers, 2009). The situation has caused several cases of lethal outcomes and serious affection on the patients’ health (Gillers, Evans, Nichols, & Alesia, 2010). At the same time, the attempt to improve Indiana’s long-term health care by means of financial “injection” has failed, as the corresponding programs have not provided proper usage of the money, having “no strings attached” (“$700 M”).
The aim of the research is to analyze the impact of different factors on the facilities’ performance and the patients’ physical and mental health, as well as to outline the unhealthy tendencies in Indiana nursing and their reasons. The research has been carried out at two facilities in Indiana, a one-star Carmel Health and Living, and a five-star Stratford at West Clay. The report is more focused on Carmel, as this facility is supposed to represent the average condition of Indiana one-star for-profit homes, which have nowadays dramatically bad performance; the data characterizing Stratford’s condition are used mostly as a criterion for comparison.
Results
Services
Carmel’s clients pay $5,000 monthly for “the bed”; Stratford provides separate apartments which cost nearly $200,000 initially and $3,000-6000 monthly. The services available at the facilities and their charging are represented in Table 1.
Table 1:Facilities’ Services and Charging
Both facilities manage to provide necessary basic services for the clients, which concern cleaning, transportation, and leisure. The clients are provided with television, telephone (paid additionally), and the possibility to visit the local establishments. Stratford provides a more diverse program for leisure and education, which is rather important in terms of fighting against the aging process: cognitive, mental, and physical activity is the fundament that makes aging progress slower.
Nurse Coverage
Considering that CNAs work 24 hours a day, and a CNA cares for 8-12 patients, a patient receives 2-3 hours a day, which means 14-21 hours per week. Taking into account that the facility is one-star, and the average level is 14.7 hours per week (Gillers, Evans, Nichols, & Alesia, 2010), a number of 21 hours sounds optimistic (Table 2). Carmel’s numbers of CNAs per patient also fit the common tendency.
Table 2:Carmel’s Nurse Coverage
Even approximate calculation shows the real meaning of these numbers. If it is difficult for a patient to hold himself up and he needs help while taking bath, it may take him about 0.3 h, including reaching the bathing place, coping with the clothes, taking bath, and returning back to his bed. Thus, only a patient’s everyday bath will “cost” 2.1 CNAs working hours for a facility, which helps to understand, how miserable the data from the table is. Moreover, if the procedure needs two CNAs to participate, it will take correspondingly 4.2 h per week. When adding, for example, 3 times of assistance when a patient visits the toilet, it becomes obvious, that the residuary hours per week do not meet any sensible requirements. At the same time, many patients require perpetual care and thorough supervision: a “slight” mistake of giving a sandwich to a dementia patient who was not allowed to be given solid food caused his death (“Dismal Data”, 2010). With CNA’s huge workload, the probability of mistakes and oversights grows dramatically, and the situation threatens to burst out with numerous lethal outcomes.
RN’s coverage is much more miserable: considering the data of 16-24 patients per shift (8 hours), a patient receives 0.3-0.5 hours per shift, which means 0.9-1.5 hours per day and 6.3-10.5 hours per week. These numbers perform much better situation than those in other for-profit facilities.
Why are RNs so important for providing the facilities’ effective work? Besides their evident responsibilities, RNs have a role of a certain interlink between a patient and a doctor and monitor the patient’s mental state. CNAs are not able to provide care of RN’s level. The representative of Carmel has mentioned that the patients are monitored by three social workers, who are reported by nurses on depression or any other cases of problems. A figure of average 2.9-3.9 hours per week provided for the patients (Gillers, Evans, Nichols, & Alesia, 2010) does not imply any possibility to watch their mental condition thoroughly; in this dimension, Carmel’s 0.9-1.5 hours a day look rather decently. Besides watching the patients’ mental condition, nurses often substitute doctors, as the doctors’ coverage is also very low, and they visit the facilities in cases of emergency.
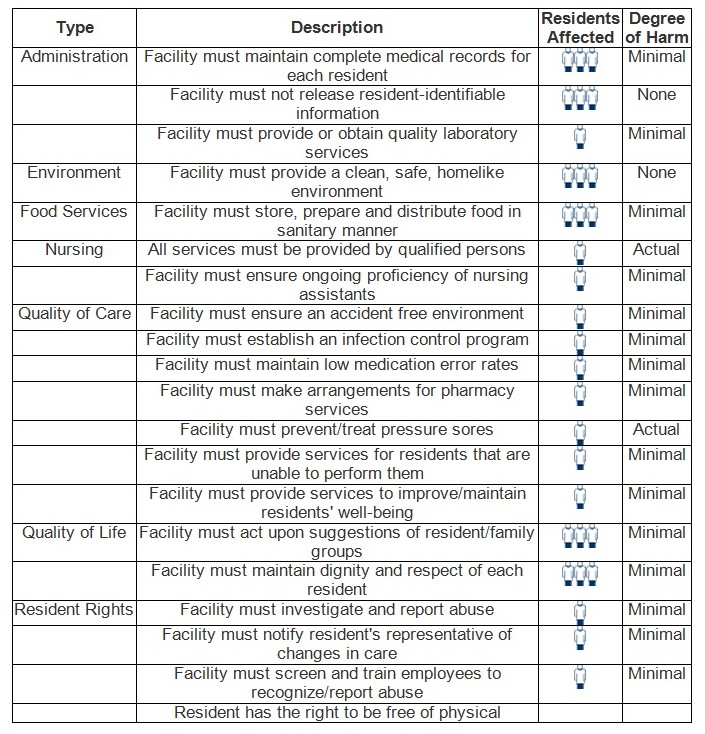
In Table 3, which shows Carmel’s deficiencies, the factors which have got the highest degree of harm are an insufficient qualification of nurses providing services and problems with preventing and treating pressure sores. Although Carmel’s overall performance is decent, these two points are a perfect illustration of the unhealthy tendencies of staff shortage. Moreover, the table shows only two “none” grades for not releasing resident-identifiable information and providing a homelike environment; the rest of the parameters have been estimated as having a minimal degree of harm, which nevertheless allows outlining the possible tendencies: for example, minimal harm grade for training employees to recognize/report abuse and ensuring ongoing proficiency of nursing assistants, together with the “actual”-graded insufficient qualification of the staff, are likely to cause the further strengthening of the negative tendencies; at the same time, several residents affected in terms of respect and not acting upon suggestions of resident/family groups can be also considered the reflection of staff shortage. Considering the 93 percent turnover rate for the CNAs in Indiana, the patients in effect are often left for the care of perpetually rotating staff, which aggravates the overall situation. Thus, the table from is a good illustration for interconnection between the number of staff and the level of care, applied for Carmel and other Indiana’s facilities.
It is difficult to compare Carmel’s coverage to that of Stratford, as the second facility does not have constant medical staff; when necessary, a client can use the services of the Home Health company, which means that he will receive guaranteed care meeting his requirements. At the same time, average staff hours at five-star nursing houses amount to 18,6 (Gillers, Evans, Nichols, & Alesia, 2010).
Influence of the Economic Condition on the Facilities
While Stratford’s management is continuing to develop marketing strategies for further selling their space, Carmel’s representative marks the negative tendency in demand: many patients have left the facility and started to live with their adult children. The economic recession has forced these families to keep money within the family budget instead of paying it to the facility. It is obvious, that the clients of one-star for-profit homes perform more elastic demand for the service than those of five-star facilities, as they feel the stronger impact of the recession upon their financial position. At the same time, it is not difficult to build the following logical sequence: losing the clients, the facilities will decrease the quality of care and service, as the CEO’s are unwilling to cut their revenues and prefer to save on staff salary and other facility’s expenditures; the low level of care will cause the further flow-out of clients who do not want to pay $5,000 monthly for bad service under the condition of recession, and the chain is closed. All mentioned above, together with the critical situation upon the nurse coverage, strengthens the idea of the necessity for the governmental regulation of the facilities’ activity.
Conclusion
A one-star nursing house Carmel Health and Living have decent performance in terms of services available and staff hours; however, it fits the overall tendency in Indiana’s long-term nursing care. Compared to a five-star Stratford at West Clay, Carmel has low indicators of nurse coverage; several potential problems concerning the future quality of care have arisen during the research. The research has provided evident argumentation for the necessity of governmental regulation on Indiana nursing houses’ activity. The unhealthy tendencies which have appeared in Indiana long-term health care are supposed to strengthen: the number of affecting cases is growing, and the further money leakage has not been hindered. At the same time, the state officials have admitted that paying no attention to the crisis tendencies has been an impermissible mistake that should be removed immediately using regulation.
References
$700M – No Strings Attached – Didn’t Help Nusring Homes. (2010). IndyStar.Com. Web.
Dismal Data Should Spur Action. (2010). IndyStar.Com. Web.
Gillers, H. (2009). Hoosier Nursing homes Score Low. IndyStar.Com. Web.
Gillers, H., T. Evans, M. Nichols, & M. Alesia. (2010). Crisis of Care. IndyStar.Com. Web.